As a DME supplier, we use modifier KX for items below the waist: knee braces, AFO's, etc. Crutches would never require this modifier because they do not have these special coverage rules. I do not believe you can bill crutches or boots if you are not a DME supplier.
Full Answer
What does modifier Kx mean?
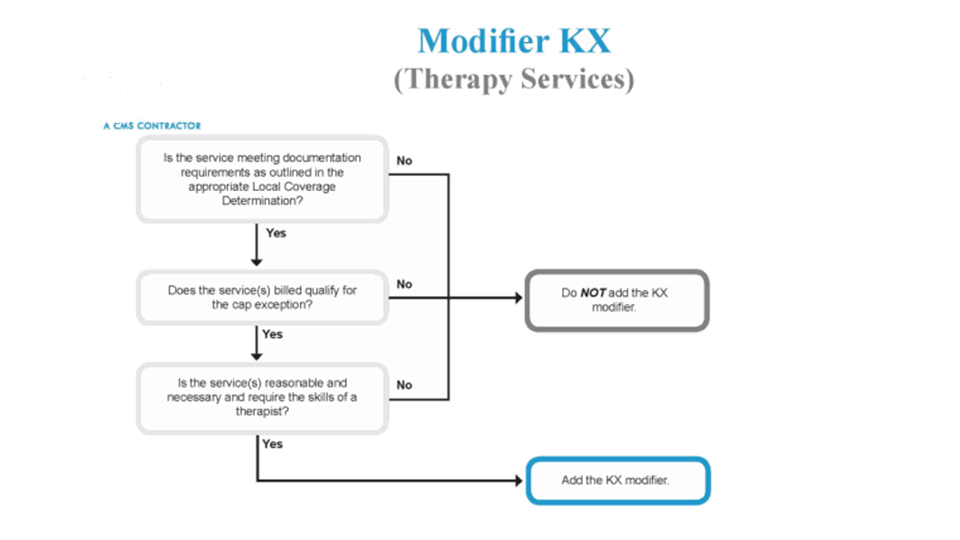
May 04, 2018 · Use of the KX modifier indicates that the supplier has ensured coverage criteria for the DMEPOS billed is met and that documentation does exist to support the medical necessity of item. Documentation must be available upon request. It is recommended for suppliers to obtain a working knowledge of specific documentation requirements for specific medical policy prior to …
When to use the KX modifier?
HCPCS Code KX Modifier: HCPCS Code List . ... LCD Article Contractor DME MAC L33788 Manual Wheelchair Bases A52497 Manual Wheelchair Bases – Policy Article CGS . AL, AR, CO, FL, GA, IL, IN, KY, LA, ... KX Modifier – Medicare Advantage Policy Guideline ...
How to add Kx modifier?
Policy Appendix: Applicable Code List KX Modifier: HCPCS Codes . This list of codes applies to the Medicare Advantage Policy Guideline titled KX Modifier. Approval Date: November 10, 2021 . Applicable Codes . The following list(s) of procedure and/or diagnosis codes is provided for reference purposes only and may not be all inclusive.
When is modifier Kx used?
May 06, 2010 · Below is a list of LCDs which include a KX modifier requirement for some or all items within that specific LCD. use of the KX modifier with any other DMEPOS is inappropriate usage. * Ankle-Foot/Knee-Ankle-Foot Orthosis * Automatic External Defibrillators * Cervical Traction Devices * Commodes * External Infusion Pumps * Glucose Monitors

When should the KX modifier be used?
The KX modifier, described in subsection D., is added to claim lines to indicate that the clinician attests that services at and above the therapy caps are medically necessary and justification is documented in the medical record.
Is the KX modifier only for Medicare?
Therapists should continue to affix the KX modifier to all medically necessary services above the designated limit ($2,010 in 2018), thus signaling Medicare to pay the claim.Oct 8, 2018
What modifier is needed for DME?
UE — USED DURABLE MEDICAL EQUIPMENT PURCHASE. This modifier is used for used DME items that are purchased. When using the UE modifier, you are indicating you have furnished the beneficiary with a used piece of equipment.
Does modifier KX affect payment?
When the KX modifier is appended to a therapy HCPCS code, the contractor will override the CWF system reject for services that exceed the caps and pay the claim if it is otherwise payable.Jan 25, 2019
What is modifier KX used in DME?
Modifier KX Use of the KX modifier indicates that the supplier has ensured coverage criteria for the billed is met and that documentation does exist to support the medical necessity of item. Documentation must be available upon request.May 4, 2018
What is the KX modifier threshold?
For 2021 this KX modifier threshold amount is: $2,110 for PT and SLP services combined, and. $2,110 for OT services.
What is the TW modifier?
Durable Medical Equipment. Effective for dates of service on and after June 1, 2004, providers are required to use modifier —TW“ when requesting prior authorization (PA) and submitting claims for back-up or secondary equipment. Modifier —TW“ for Back-up Durable. Medical Equipment.
What is KF modifier for Medicare?
Modifier KF is a pricing modifier. The HCPCS codes for DME designated as class III devices by the FDA are identified on the DMEPOS fee schedule by presence of the KF modifier.
What is MS modifier?
Modifier MS Six month maintenance and servicing fee for reasonable and necessary parts and labor which are not covered under any manufacturer or supplier warranty.May 7, 2018
Where do you put the KX modifier?
The KX modifier is appended on claims at or very close to the $1920 cap, and should not applied from the first visit, even if the therapist knows that the cap will likely be exceeded. At least one MAC has notified therapists that a pattern of early application of the KX modifier may be consider an abuse practice.Jan 14, 2014
How do I install KX modifier?
By adding modifier KX to a claim, you are stating that your claim has met specific documentation requirements in the policy, and would be available upon request from the Medicare Administrative Contractor (MAC). Add this modifier to each procedure code once the specific therapy cap has been met.Oct 21, 2021
Does Medicare accept physical status modifiers?
Physical status modifiers are not recognized by Medicare.Nov 1, 2016
When did the KX modifier expire?
Section 202 of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) extended the therapy cap exceptions process through December 31, 2017. As a reminder, excessive use of the KX modifier including routine use of the modifier prior to reaching the cap limits may indicate abusive billing.
What is the KX modifier?
A: The KX modifier is added to claim lines to indicate that the clinician attests that services are medically necessary and justification is documented in the medical record. Even though no special documentation is submitted to the contractor for automatic process exceptions, the clinician is responsible for consulting guidance in the Medicare manuals and in the professional literature to determine if the beneficiary qualifies for the automatic process exception. In addition, the clinician’s opinion is not binding on the Medicare contractor; the Medicare contractor makes the final determination concerning whether the claim is payable.#N#Q: When are exceptions to the therapy caps for services provided in a SNF setting considered?#N#Revised 09/2015
When exceptions are in effect and the beneficiary qualifies for a therapy cap exception, the provider shall add
When exceptions are in effect and the beneficiary qualifies for a therapy cap exception, the provider shall add a KX modifier to the therapy HCPCS code subject to the cap limits. The KX modifier shall not be added to any line of service that is not a medically necessary service; this applies to services that, according to a local coverage determination by the contractor, are not medically necessary services.
What is documentation justifying services?
A: Documentation justifying the services shall be submitted in response to any Additional Documentation Request (ADR) for claims that are selected for medical review. If medical records are requested for review, clinicians may include, at their discretion, a summary that specifically addresses the justification for therapy cap exception and they should follow the documentation requirements listed
When did CMS change the fee schedule?
On June 11, 2018 , CMS announced a change to the way that fee schedule amounts for DME are established, indicating that prices paid by other payers may be used to establish the Medicare fee schedule amounts for new technology items and services.
When will DME be enforced?
Due to concerns that some providers and suppliers may need additional time to establish operational protocols necessary to comply with face-to-face encounter requirements mandated by the Affordable Care Act (ACA) for certain items of Durable Medical Equipment (DME), CMS will start actively enforcing and will expect full compliance with the DME face-to-face requirements beginning on October 1, 2013.
What is a DMEPOS file?
The DMEPOS public use file contains fee schedules for certain items that were adjusted based on information from the DMEPOS Competitive Bidding Program in accordance with Section 1834 (a) (1) (F) of the Act.
When does the Cares Act end?
Section 3712 (a) of the CARES Act extends the current adjusted fee schedule methodology that pays for certain items furnished in rural and non-contiguous non-CBAs based on a 50/50 blend of adjusted and unadjusted fee schedule amounts through December 31, 2020 or through the duration of the PHE, whichever is later.
What is the Cares Act?
Section 3712 (a) of the CARES Act extends the current adjusted fee schedule methodology that pays for certain items furnished in rural and non-contiguous non-CBAs based on a 50/50 blend of adjusted and unadjusted fee schedule amounts through December 31, 2020 or through the duration of the PHE , whichever is later. Section 3712 (b) of the Act requires the calculation of new, higher fee schedule amounts for certain items furnished in non-rural contiguous non-CBAs based on a blend of 75 percent of the adjusted fee schedule amount and 25 percent of the unadjusted fee schedule amount for the duration of the PHE.
When will CMS reprocess claims?
Claims for these accessories submitted prior to July 1, 2020, with dates of service from January 1, 2020 through June 30, 2020, will need to be reprocessed to ensure that CMS pays the unadjusted fee schedule amounts, as required by section 106 of the Further Consolidated Appropriations Act, 2020.
What is the 106 of the 106?
116-94) was signed into law on December 20, 2019. Section 106 of the Further Consolidated Appropriations Act, 2020 mandates the non-application of fee schedule adjustments based on information from competitive bidding programs for wheelchair accessories (including seating systems) and seat and back cushions furnished in connection with complex rehabilitative manual wheelchairs (HCPCS codes E1161, E1231, E1232, E1233, E1234 and K0005) and certain manual wheelchairs currently described by HCPCS codes E1235, E1236, E1237, E1238, and K0008 during the period beginning on January 1, 2020 and ending June 30, 2021.