What are the laws against Medicare fraud?
Sep 30, 2021 · What do federal agents say is a major part of Medicare fraud? A) Mistakes made by users who do not understand complex features of the program. B) The complex billing process required by law. C) Health-care providers are putting services into a higher paying category in order to increase profits.
Who investigates Medicare fraud complaints?
Jul 01, 2015 · How CMS Handles Complaints. When a beneficiary calls 1-800-Medicare to report an issue, their staff will determine if this was an error, abuse, or outright fraud. Also how the complaint is handled is based on the part of coverage including Original Medicare (Parts A & B), Medicare Advantage (Part C), or a Medicare Prescription Drug Plan (Part D).
What are the different types of Medicare fraud?
Agents are backed by forensic accountants, health care professionals and data acquisition analysts who have a pipeline to Medicare contractors' billing information. Health care fraud, and Medicare fraud in particular, are extremely high priorities, and will continue to be so," says Leslie Caldwell, head of the Justice Department's criminal division.
What is in the Medicare fraud and abuse booklet?
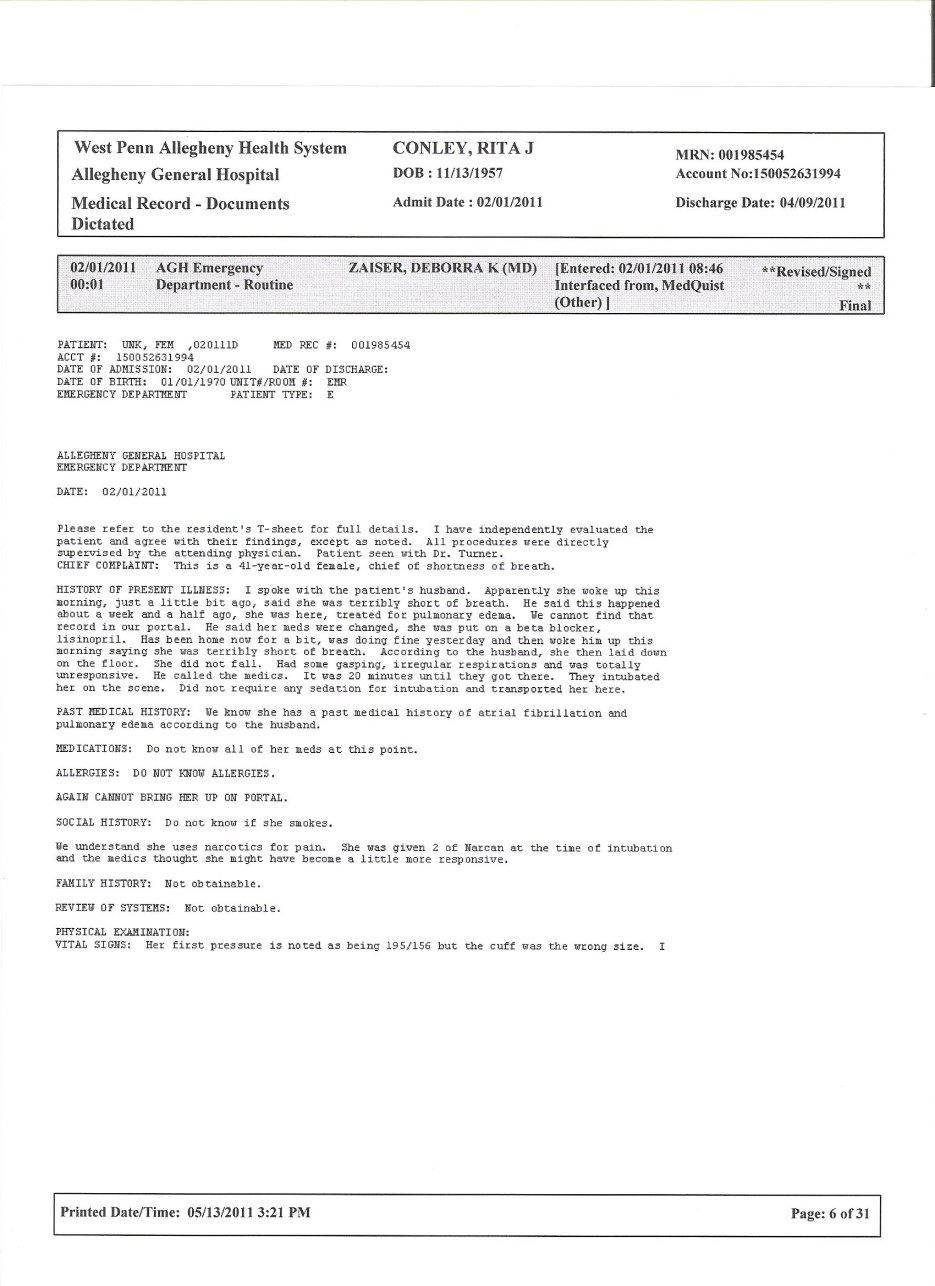
Aug 19, 2009 · Federal agents raided dozens of doctors’ offices and homes during investigations into alleged Medicare fraud. As part of the government’s effort to reform health care and save money, the federal government is focusing on Medicare fraud and what they say are millions of dollars that are fraudulently taken from the government pursuant to the Medicare laws.

What is a major part of Medicare fraud?
Beneficiaries commit fraud when they… Let someone use their Medicare card to get medical care, supplies or equipment. Sell their Medicare number to someone who bills Medicare for services not received. Provide their Medicare number in exchange for money or a free gift.
What are examples of Medicare fraud?
Additional examples of Medicare scams include: A person without Medicare coverage offering money or goods to a Medicare beneficiary in exchange for their Medicare number in order to use their Medicare benefits. A sales person offering a prescription drug plan that is not on Medicare's list of approved Part D plans.Dec 7, 2021
What is the largest Medicare fraud case?
In July 2010, the Medicare Fraud Strike Task Force announced its largest fraud discovery ever when charging 94 people nationwide for allegedly submitting a total of $251 million in fraudulent Medicare claims.
How do you identify Medicare fraud?
Billing ScamsBills from hospitals you did not visit.Bills from providers you do not know.Bills for services you did not receive.Jan 31, 2021
Is there a lot of Medicare fraud?
Somewhere around $1.3 billion. The large sums of money being scammed out of elderly people is part of the reason why Medicare Fraud Strike Force Teams across the country spend their days trying to shut down these types of dishonest healthcare professionals. In some cases, they net extremely positive results.Jan 6, 2022
What are the types of Medicare fraud?
Types of Medicare fraud 1 Phantom billing: The medical provider bills Medicare for unnecessary procedures, or procedures that are never performed; for unnecessary medical tests or tests never performed; for unnecessary equipment; or equipment that is billed as new but is, in fact, used. 2 Patient billing: A patient who is in on the scam provides his or her Medicare number in exchange for kickbacks. The provider bills Medicare for any reason and the patient is told to admit that he or she indeed received the medical treatment. 3 Upcoding scheme and unbundling: Inflating bills by using a billing code that indicates the patient needs expensive procedures.
How much did Omnicare pay to settle the Qui Tam lawsuit?
In November 2009, Omnicare paid $98 million to the federal government to settle five qui tam lawsuits brought under the False Claims Act and government charges that the company had paid or solicited a variety of kickbacks. The company admitted no wrongdoing. The charges included allegations that Omnicare solicited and received kickbacks from a pharmaceutical manufacturer Johnson & Johnson, in exchange for agreeing to recommend that physicians prescribe Risperdal, a Johnson & Johnson antipsychotic drug, to nursing home patients.
What is the Office of Inspector General?
Department of Health and Human Services, as mandated by Public Law 95-452 (as amended), is to protect the integrity of Department of Health and Human Services (HHS) programs, to include Medicare and Medicaid programs, as well as the health and welfare of the beneficiaries of those programs . ...
How much did HCA pay to the government?
In late 2002, HCA agreed to pay the U.S. government $631 million, plus interest, and pay $17.5 million to state Medicaid agencies, in addition to $250 million paid up to that point to resolve outstanding Medicare expense claims.
When did Columbia HCA get raided?
Numerous New York Times stories, beginning in 1996, began scrutinizing Columbia/HCA's business and Medicare billing practices. These culminated in the company being raided by Federal agents searching for documents and eventually the ousting of the corporation's CEO, Rick Scott, by the board of directors.
Who is Fatima Hassan?
Fatima Hassan, co-owned a company known as Jos Campau Physical Therapy with Javasundera, pleaded guilty on August 25, 2011, for her role in the Medicare fraud schemes and on May 17, 2012, was sentenced to 48 months in prison.
What is heat in Medicare?
The DOJ, OIG, and HHS established HEAT to build and strengthen existing programs combatting Medicare fraud while investing new resources and technology to prevent and detect fraud and abuse . HEAT expanded the DOJ-HHS Medicare Fraud Strike Force, which targets emerging or migrating fraud schemes, including fraud by criminals masquerading as health care providers or suppliers.
What is the role of third party payers in healthcare?
The U.S. health care system relies heavily on third-party payers to pay the majority of medical bills on behalf of patients . When the Federal Government covers items or services rendered to Medicare and Medicaid beneficiaries, the Federal fraud and abuse laws apply. Many similar State fraud and abuse laws apply to your provision of care under state-financed programs and to private-pay patients.
What does "knowingly submitting" mean?
Knowingly submitting, or causing to be submitted, false claims or making misrepresentations of fact to obtain a To learn about real-life cases of Federal health care payment for which no entitlement Medicare fraud and abuse and would otherwise existthe consequences for culprits,
What is the OIG?
The OIG protects the integrity of HHS’ programs and the health and welfare of program beneficiaries. The OIG operates through a nationwide network of audits, investigations, inspections, evaluations, and other related functions. The Inspector General is authorized to, among other things, exclude individuals and entities who engage in fraud or abuse from participation in all Federal health care programs, and to impose CMPs for certain violations.
What is the Stark Law?
Section 1395nn, often called the Stark Law, prohibits a physician from referring patients to receive “designated health services” payable by Medicare or Medicaid to an entity with which the physician or a member of the physician’s immediate family has a financial relationship , unless an exception applies.
What is the OIG exclusion statute?
Section 1320a-7, requires the OIG to exclude individuals and entities convicted of any of the following offenses from participation in all Federal health care programs:
Is there a measure of fraud in health care?
Although no precise measure of health care fraud exists, those who exploit Federal health care programs can cost taxpayers billions of dollars while putting beneficiaries’ health and welfare at risk. The impact of these losses and risks magnifies as Medicare continues to serve a growing number of beneficiaries.
What is a fraudulent billing?
Fake billing is part of a patient’s health record, which is increasingly kept electronically. In an era fraught with the loss of personal medical information, fraudulent billing has the potential to affect things such as life insurance rates and future medical treatment.
Who is Kirk Ogrosky?
Kirk Ogrosky, a former federal prosecutor who fought Medicare fraud, says the bilking of Medicare should concern everyone, even those who are not yet old enough to take advantage of the program, because they help pay for it through taxes. “Every American should be angry about it,” Ogrosky says.