Full Answer
What happens if Medicare denies my claim?
If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all. They may “change or reverse the denial.” You can appeal if:
What to do if you receive a Medicare denial letter?
After you receive a denial letter, you have the right to appeal Medicare’s decision. The appeals process varies depending on which part of your Medicare coverage was denied. Let’s take a closer look at the reasons you might receive a denial letter and the steps you can take from there. Why did I receive a Medicare denial letter?
How do I appeal a denied Medicare claim?
Here’s how to appeal a denied Medicare claim depending on the parts of Medicare involved. To appeal a denied Medicare Part A or Medicare Part B claim, you must start the appeal process within 120 days of initial notification. You will use the Medicare Redetermination Form to file your claim.
What to do if Medicare refuses to pay for a drug?
Medicare refuses to pay the amount you must pay for a drug. Medicare stops paying for all or part of a service you think you still need. If you need help with an appeal, call the Medicare Advocacy Project at 1-800-323-3205 to apply for assistance. Take action right away. You must appeal by the deadline.
Why does my Medicare Plan Get Denied?
Before moving on with the reasons for a claim denial, we first have to understand that your claim can either be rejected or denied.
What does it mean when a Medicare claim is rejected?
According to the Medicare Administrative Contractor WPS-GHA, a rejected claim means, “Any claim with the incomplete or missing required information or any claim that contains complete and necessary information; however, the information provided is invalid.
What is Medicare?
Medicare is a federal health insurance program for certain individuals in the country. Medicare’s main goal is to subsidize healthcare services for select individuals that need the most help. These include the following:
What Happens When I Submit a Claim Beyond the Filing Limit?
Any claims submitted beyond this filing window are denied and can’t be appealed. There are cases, however, when consideration is given if the person can prove a Medicare representative is the cause of the delay.
How to reverse a Medicare rejection?
How To Reverse a Denial or Rejection from Medicare. In order to fix rejections, you just have to resubmit your email with the correct information. When you get a rejected claim, the missing or wrong information will be identified so you can adjust easily. Denials, on the other hand, are a bit tricky.
How long do you have to appeal a CER?
To appeal, you need to write a letter and there are five appeal levels you can pursue. You have 120 days from the date of the receipt of your remittance advance to write an appeal to the first stage.
Does Medicare cover kidney failure?
People who are suffering from end-stage renal disease (people who are experiencing permanent kidney failure and require dialysis or transplant) Medicare has different plans that can cover different healthcare situations. Some of these come at a cost to the person being insured.
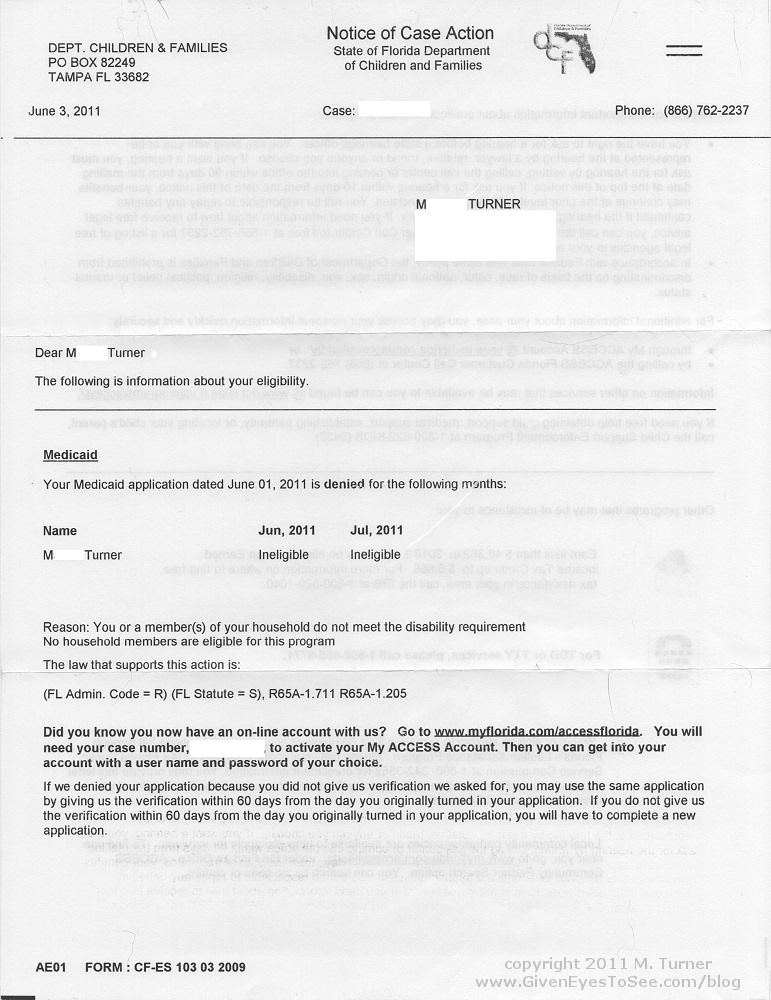
What happens if you are denied Medicare?
When a Medicare claim is denied, you will receive a letter notifying you that a specific service or item is not covered or no longer covered. This can also happen if you are already receiving care but have exhausted your benefits.
What does it mean if Medicare denied my claim?
Though Medicare is designed to give seniors and certain disabled individuals the most unobstructed access to healthcare possible , there are some rare circumstances that may unfortunately lead to a Medicare claim denial.
What are the key things to remember when considering a Medicare denied claim appeal?
In addition, take the time to review your coverage plan and your denial letter thoroughly.
How long does it take to appeal a Medicare claim?
To appeal a denied Medicare Part A or Medicare Part B claim, you must start the appeal process within 120 days of initial notification. You will use the Medicare Redetermination Form to file your claim. If the appeal is denied, you will need to move on to level 2 reconsideration.
What is a denial letter for skilled nursing?
This type of denial letter is intended to notify you that an upcoming healthcare service or item received via a skilled nursing facility will not be covered by Medicare.
How many types of denial letters are there for Medicare?
There are four main types of Medicare denial letters that you may receive depending on the specific reasoning behind your claim’s denial. At MedicareInsurance.com, we’re here to help you take a closer look at why your Medicare claim was denied and what you might be able to do about it going forward.
Can Medicare deny a claim?
Medicare may deny your claim based on a few different factors. The exact reasoning behind your denied Medicare claim will be explained to you in the context of your denial letter. Learn more about the four main types of denial letters right here.
What happens if Medicare denies coverage?
If you feel that Medicare made an error in denying coverage, you have the right to appeal the decision. Examples of when you might wish to appeal include a denied claim for a service, prescription drug, test, or procedure that you believe was medically necessary.
Why did I receive a denial letter from Medicare?
Example of these reasons include: You received services that your plan doesn’t consider medically necessary. You have a Medicare Advantage (Part C) plan, and you went outside the provider network to receive care.
What is an integrated denial notice?
Notice of Denial of Medical Coverage (Integrated Denial Notice) This notice is for Medicare Advantage and Medicaid beneficiaries, which is why it’s called an Integrated Denial Notice. It may deny coverage in whole or in part or notify you that Medicare is discontinuing or reducing a previously authorized treatment course. Tip.
How to avoid denial of coverage?
In the future, you can avoid denial of coverage by requesting a preauthorization from your insurance company or Medicare.
How many steps does Medicare appeal go through?
After you receive your Medicare denial letter and decide to appeal it, your appeal will usually go through five steps. These include:
How long does it take to get an appeal from Medicare Advantage?
your Medicare Advantage plan must notify you of its appeals process; you can also apply for an expedited review if you need an answer faster than 30–60 days. forward to level 2 appeals; level 3 appeals and higher are handled via the Office of Medicare Hearings and Appeals.
What happens if you don't follow Medicare rules?
You may receive a Medicare denial letter if you do not follow a plan’s rules or if your benefits have run out.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How to appeal Medicare summary notice?
If you have Original Medicare, start by looking at your " Medicare Summary Notice" (MSN). You must file your appeal by the date in the MSN. If you missed the deadline for appealing, you may still file an appeal and get a decision if you can show good cause for missing the deadline.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What to do if you decide to appeal a health insurance plan?
If you decide to appeal, ask your doctor, health care provider, or supplier for any information that may help your case. See your plan materials, or contact your plan for details about your appeal rights.
What happens if Medicare doesn't pay?
What if Medicare will not pay for something? If Medicare refuses to pay for something, they send you a “denial” letter. The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.”.
What is it called when you think Medicare should not pay?
If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial .”. If you appeal a denial, Medicare may decide to pay some or all of the charge after all. They may “change or reverse the denial.”. You can appeal if:
What happens if you don't get a favorable decision?
If you do not receive a favorable decision, you may appeal to an Administrative Law Judge, then to the Medicare Appeals Council then to Federal Court.
What happens if you appeal Medicare?
If you appeal, Medicare will write back to you and tell you their decision. If they still deny your claim, the letter will include instructions for how to file the next step of the appeal.
How often do you get a Medicare statement?
If you have Part B Original Medicare, you should get a statement every three months. The statement is called a Medicare Summary Notice (MSN). It shows the services that were billed to Medicare. It also shows you if Medicare will pay for these services.
How to contact Medicare Advocacy Project?
If you need help with an appeal, call the Medicare Advocacy Project at 1-800-323-3205 to apply for assistance.
Can Medicare reverse a denial?
They may “change or reverse the denial.”. You can appeal if: Medicare refuses to pay for a health care service, supply or prescription that you think you should be able to get. Medicare refuses to pay the bill for health care services or supplies or a prescription drug you already got.
What Happens When Your Medicare Enrollment Application Is Denied or Rejected?
Whether you are a prospective supplier / provider seeking enrollment for the first time, or are seeking enrollment following a revocation or exclusion, your application will result in one of three actions:
Why is it important to appeal a denial of Medicare?
Because enrollment in Medicare and the ability to bill federal programs can be critical to practitioners, suppliers, and medical practices, ensuring you take the right steps to limit exposure to regulatory risks the first time around is critical. Even more so, seeking the help of experienced health care attorneys when appealing a denial from Medicare can help you make the most of your rights and limited opportunities to rectify a difficult situation.
What happens if a CMS enrollment is rejected?
If an application is formally rejected, applicants must re-initiate the enrollment process, complete a new CMS-855 form, and re-submit all supplementary documentation. Providers / suppliers who have their enrollment applications rejected do not have the right to appeal.
How long does it take for a CMS denial to be reversed?
If, for example, an applicant was denied due to the adverse actions of a managing employee or anyone in the practice / company, CMS can reverse the denial if applicants submit proof that they terminated relationships with those individuals within 30 days of receiving a denial notice.
When was Medicare first created?
At the time Medicare was first created in 1965 , lawmakers felt placing overly restrictive conditions on enrollment would hinder the program’s viability. Until recently, there were few barriers to enrolling in Medicare, as either a supplier or a provider. Following a crack-down on Medicare fraud, CMS powers progressively strengthened.
Is Medicare debt overpayment a felony?
Existing Medicare debt / overpayment. Convictions for certain crimes, including any conviction within the past 10 years involving a felony crime (i.e. crimes against a person), a felony which places beneficiaries or the program at risk (i.e. criminal negligence / misconduct), and certain financial crimes (i.e.
Can a provider be denied Medicare?
There are a number of reasons why a provider / supplier may be denied enrollment in Medicare. Some examples include:
What happens if you don't check your Medicare provider number?
Incorrect Information Could Lead to the Termination of Your Medicare Provider Number. The consequences of not checking your information on file are severe, and can include termination of your Medicare provider number and billing privileges. – You are prohibited from reapplying to Medicare for at least two years.
How long can you reapply for Medicare after termination?
The effect of this termination includes: – You are prohibited from reapplying to Medicare for at least two years. – You may have to pay back any money received from the Medicare program since the effective date of the termination (often many months prior to the notification letter).
Does Medicare deny DME?
The Centers for Medicare and Medicaid Services (CMS) will deny Medicare applications of physicians, medical groups, home health agencies (HHAs), pharmacies and durable medical equipment (DME) suppliers because the name on file with the National Plan & Provider Enumeration System (NPPES) is not the same legal business name as reported to the Internal Revenue Service (IRS).
