If Medicare decides to reject the claim, you can challenge the decision. This is called an appeal. In the United States, people have the right to appeal a denied claim for up to six months after hearing about this decision.
How do I search for a rejected Medicare claim?
Jan 09, 2020 · If you have Medicare health insurance, your healthcare practitioner will usually submit claims directly to Medicare for payment. If Medicare decides to reject the claim, you can challenge the decision. This is called an appeal. In the United States, people have the right to appeal a denied claim for up to six months after hearing about this decision.
How do I know if a claim/line item has been rejected?
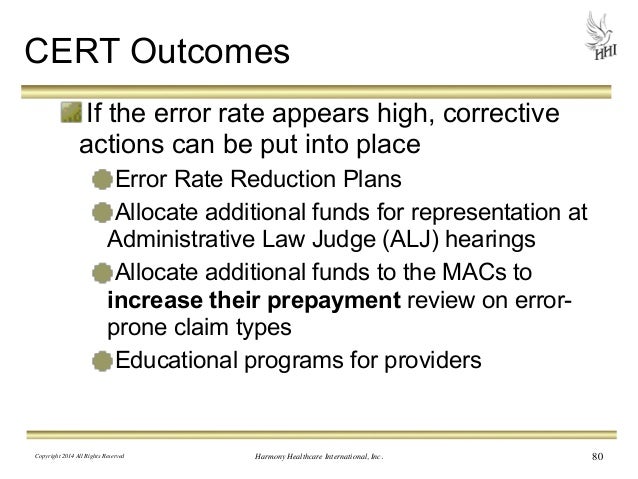
Feb 28, 2021 · When a claim is denied for reasons that cannot be addressed with a CER then it should be appealed. To appeal, you need to write a letter and there are five appeal levels you can pursue. Level 1 – Redetermination by a Medicare Administrative Contractor (MAC) Level 2 – Reconsideration by a Qualified Independent Contractor (QIC)
What can I do if my Medicare plan is denied?
Mar 02, 2022 · A: Occasionally, claim rejects will post to the beneficiary’s records on the Common Working File (CWF). The most common effected rejection reason code range is 34XXX (Medicare secondary payer). If a claim reject has posted to the CWF, a new claim submission is subject to duplicate editing.
Why did my home health claim get rejected?
Jan 21, 2020 · Select the rejected claim you are researching by typing an "S" in the SEL field next to the Medicare ID number of the claim and press
When a claim is rejected by Medicare can you resubmit?
The most common effected rejection reason code range is 34XXX (Medicare secondary payer). If a claim reject has posted to the CWF, a new claim submission is subject to duplicate editing. Claim rejects that have posted to the CWF may be adjusted within the appropriate timeframe.Mar 2, 2022
How do I find out why my Medicare claim was denied?
A Medicare Summary Notice (MSN) is a summary of the health care services you have received over the past three months, sent to you by mail. It shows what Medicare paid for each service and what you owe for the service, and it will show if Medicare fully or partially denied a medical claim.Jan 9, 2020
Can you adjust a denied Medicare claim?
Please note: Adjustments cannot be made to any part of a denied line item on a partially paid claim.Nov 25, 2020
How do I resubmit my Medicare claim?
Open the patient file, and select Transactions. Right-click the appropriate transaction and select 'Medicare Online', followed by the type of claim to be submitted (Patient Claim, Medicare BB or DVA). Complete the Medicare/DVA claiming wizard to resubmit the claim using the corrected information. Congratulations!
What is CWF initiated adjustment claim?
Upon receipt of an unsolicited response, the Fiscal Intermediary Standard System (FISS) creates a CWF initiated adjustment claim (type of bill xxG). In certain circumstances during processing, these CWF initiated adjustment claims may encounter other edits and be returned to the provider (RTP).Oct 29, 2004
Can you correct a rejected claim in DDE?
1. To adjust paid or rejected claims, enter the Claims Adjustments option (21,23, or 25) that matches your provider type and press Enter.Aug 25, 2014
How do Medicare adjustments work?
The Medicare system adjusts fee-for-service payment rates for hospitals and practitioners1 according to the geographic location in which providers practice, recognizing that certain costs beyond the providers' control vary between metropolitan and nonmetropolitan areas and also differ by region.
Tips For Avoiding Claims from Rejecting
1. Always check a beneficiary's eligibility using the ELGH or ELGA eligibility systems prior to admission and billing Medicare. Access Chapter 2 -...
Electronically Adjusting A Rejected Claim
If the original claim information has posted to the CWF (TPE-TO-TPE field is blank), you will need to adjust the original claim. Resubmitting a new...
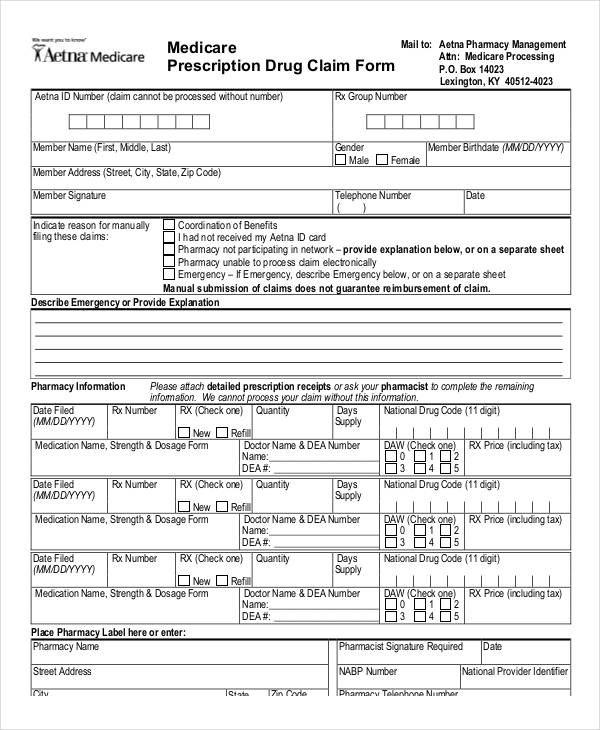
Submitting A Paper Claim Adjustment
In the rare circumstance that an electronic adjustment is not possible, the alternative option is to submit a paper adjustment (UB-04). Because the...
Tips for Avoiding Claims from Rejecting
Always check a beneficiary's eligibility using the ELGH or ELGA eligibility systems prior to admission and billing Medicare. Access Chapter 2 - Checking Beneficiary Eligibility of the Fiscal Intermediary Standard System (FISS) Guide for more information about verifying eligibility information for Medicare beneficiaries.
Resubmitting a New Claim
If the claim information did not post to the CWF, submit a new claim with corrected information. Typically, home health claims that overlap a beneficiary's hospice election or a Medicare Advantage (MA) Plan enrollment period do not post information to CWF when they reject.
Electronically Adjusting a Rejected Claim
If the original claim information has posted to the CWF (TPE-TO-TPE field is blank), you will need to adjust the original claim. Resubmitting a new claim may cause the claim to reject as a duplicate.
Submitting a Paper Claim Adjustment
In the rare circumstance that an electronic adjustment is not possible, the alternative option is to submit a paper adjustment (UB-04). Because the rejected claim posted the episode information out on CWF, HHAs should not submit a new Request for Anticipated Payment (RAP) for the episode prior to submitting the adjustment.
How many levels of appeals are there?
All appeals must be made in writing, and there are five appeal levels a provider can pursue: Level 1 – Redetermination by a Medicare Administrative Contractor (MAC) Level 2 – Reconsideration by a Qualified Independent Contractor (QIC) Level 3 – Decision by Office of Medicare Hearings and Appeals (OMHA)
Do Medicare claims have to be processed correctly?
Ideally, claims submitted to Medicare are always entered and processed correctly and then paid on time according to the Medicare fee schedule. But since we live in the real world, where mistakes can and do happen at any point in the billing process, here are four tips to help you identify and correct billing errors on Medicare claims.
Is "rejection" a synonym for "denial"?
Let’s face it: rejections and denials don’t sound all that different. In fact, if you look up “denial” in a thesaurus, “rejection” is listed among the acceptable synonyms. But in Medicare parlance, the two words mean different things.
What is a CER in insurance?
When a claim is denied because the information submitted was incorrect, often the claim can be reopened using a Clerical Error Reopening (CER). CERs can be used to fix errors resulting from human or mechanical errors on the part of the party or the contractor.
Who is Charity Singleton?
Charity Singleton Craig is a freelance writer and editor who provides communications and marketing services for CIPROMS. She is responsible for creating, editing, and managing all content, design, and interaction on the company website and social media channels in order to promote CIPROMS as a thought leader in healthcare billing and management.
Can a rejected claim be appealed?
Claims rejected as unprocessable cannot be appealed and instead must be resubmitted with the corrected information. The rejected claim will appeal on the remittance advice with a remittance advice code of MA130, along with an additional remark code identifying what must be corrected before resubmitting the claim.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
What to do if you decide to appeal a health insurance plan?
If you decide to appeal, ask your doctor, health care provider, or supplier for any information that may help your case. See your plan materials, or contact your plan for details about your appeal rights.
How many levels of appeals are there?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.