
Aetna Medicare Advantage plans that include dental benefits can cover preventive and routine services like exams, X-rays, cleanings and fluoride treatments, typically with a small copay or no copay at all required when performed by an in-network dentist.
Full Answer
Does Aetna have a good dental plan?
Oct 07, 2021 · What’s covered under Medicare Advantage dental plans. Some of the covered dental services may include (be sure to check with your plan for details): Oral exams; Cleanings; X-rays; Fillings; Root canal treatments; Tooth extractions; Crowns, …
What insurances does Aetna offer?
Oct 19, 2021 · Certain Aetna Medicare Advantage plans may offer coverage for dental care. Medicare Part A will pay for certain dental services when you’re in the hospital. It doesn’t cover routine dental care. Aetna Medicare Advantage plans offer the same coverage as Original Medicare, and some plans may offer additional benefits that cover routine dental services like …
Is Aetna a Medicare Advantage plan?
May 09, 2022 · Many Aetna Medicare Advantage plans also include prescription drug coverage and may cover medications prescribed by your dentist following oral surgery or other procedures. Exact coverage may vary by plan, but some of the other covered dental services included in an Aetna Medicare Advantage plan can include: Exams; X-rays; Cleanings; Fillings; …
What dental plans are offered by Aetna?
Oct 21, 2018 · For the purposes of Aetna’s coverage in its Medicare Advantage plans, the following services may be considered routine: Oral examinations in a dentist’s office. X-rays, including panoramic and bite wing views. Pulp vitality tests. Cleaning, scaling, and polishing the teeth. Oral hygiene consultations.
Do Medicare supplements include dental and vision?
Is Aetna Medicare Advantage the same as Medicare?
Is Aetna Medicare considered an advantage plan?
In addition to PPO plans, Aetna offers you other Medicare Advantage plan options — many with a $0 monthly plan premium.Jan 6, 2022
Does Aetna Medicare Advantage have the give back benefit?
Why do doctors not like Medicare Advantage plans?
What are the negatives of a Medicare Advantage plan?
Who Has the Best Medicare Advantage Plan for 2022?
What is Aetna Advantage?
What is the most popular Medicare Part D plan?
| Rank | Medicare Part D provider | Medicare star rating for Part D plans |
|---|---|---|
| 1 | Kaiser Permanente | 4.9 |
| 2 | UnitedHealthcare (AARP) | 3.9 |
| 3 | BlueCross BlueShield (Anthem) | 3.9 |
| 4 | Humana | 3.8 |
How do you qualify to get $144 back on your Medicare?
- Are enrolled in Part A and Part B.
- Do not rely on government or other assistance for your Part B premium.
- Live in the zip code service area of a plan that offers this program.
- Enroll in an MA plan that provides a giveback benefit.
Who is the largest Medicare Advantage provider?
What is the income limit for extra help in 2021?
What is EOC dental?
Check your plan’s Explanation of Coverage (EOC) to see exactly what dental coverage benefits may be offered by your plan. If your Aetna Medicare Advantage plan offers dental benefits, the costs for your covered dental services may be included in the plan’s premium or as an Optional Supplemental Benefit, which means you would need ...
What dental services are covered by Aetna?
What dental services may be covered by an Aetna Medicare plan? If you enroll in an Aetna Medicare Advantage plan that includes dental coverage, some of the services that may be covered include: Teeth cleaning, scaling and polishing. Office visits for oral examinations. Non-surgical extractions. Fillings.
How to contact Medicare 2021?
If you'd like to speak with an agent right away, we're standing by for that as well. Give us a call! 1-877-890-1409 TTY 711, 24/7 LICENSED AGENTS AVAILABLE NOW.
Does Aetna cover dental insurance?
An Aetna Medicare Advantage plan that covers dental care may offer the benefits through an allowance or via a network of approved dental care providers.
Does Aetna Medicare cover dental?
Medicare Part A will pay for certain dental services when you’re in the hospital. It doesn’t cover routine dental care. Aetna Medicare Advantage plans offer the same coverage as Original Medicare, and some plans may offer additional benefits that cover routine dental ...
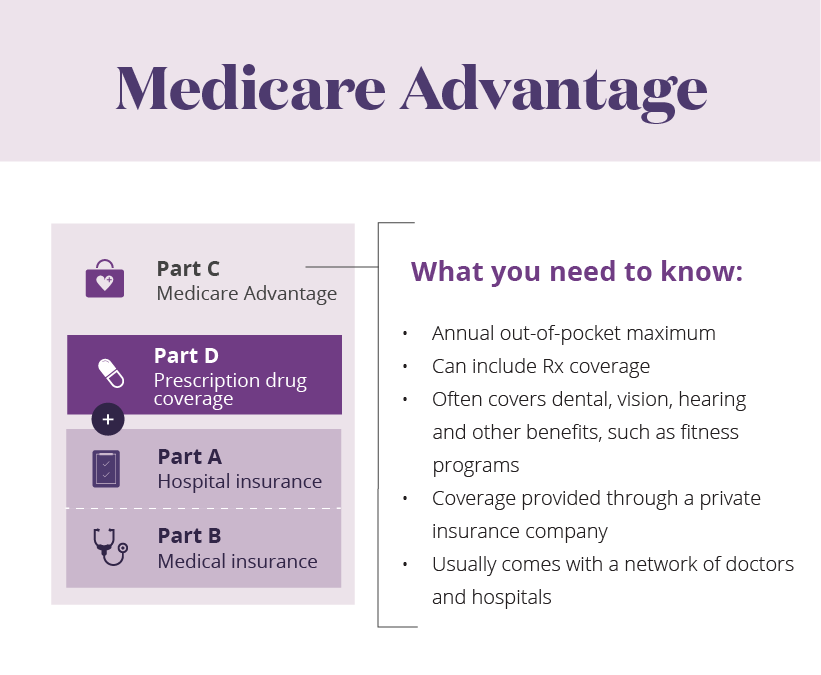
What is Medicare Advantage?
Medicare Advantage, otherwise known as Medicare Part C, is an alternative way to receive your Original Medicare coverage while also receiving some additional benefits not included in Medicare Part A or B.
Is dental care covered by Medicare?
Depending on the plan, there may be deductibles, copays or coinsurance costs for some covered care. Preventive dental care is often fully covered by Medicare Advantage plans, with some restrictions.
Does Aetna Medicare include dental insurance?
Not all Aetna Medicare plans include dental coverage. For those that do not, a supplemental dental package may be purchased and added to the plan. The dental package may also be added to plans that already include dental benefits for members who wish to enhance their coverage further.
Does Aetna pay for dental insurance?
Some Aetna Medicare plans give members a set amount of money each year (often called a plan allowance) to spend on dental care. You’ll typically pay for your dental care up front and then submit your receipt to Aetna and get reimbursed for covered care up to your plan allowance limit.
Is Aetna a PPO or HMO?
Aetna Medicare Advantage plans may come in the form of HMO or PPO plans, among some other types of plan.
Does Aetna cover dental care?
Preventive dental care – which can include dental exams, X-rays, teeth cleanings and more – can be covered by many Aetna Medicare plans. Your Aetna Medicare Advantage plan may have an annual deductible along with copayments or coinsurance requirements for dental services, depending on the plan.
Does Aetna Medicare cover dental?
Most Aetna Medicare Advantage plans include dental coverage. Learn more about these plans, the dental benefits they may offer and how you may apply for an Aetna Medicare plan that covers dental benefits.
What services do you need to be on Medicare Advantage?
Routine dental services. Routine vision and hearing care. Prescription drugs. Wellness programs. Also, you need to know that when you’re enrolled in a Medicare Advantage plan, you’re still in the Medicare program, and you need to continue paying your monthly Medicare Part B premium, in addition to any plan premium.
What are the services that Aetna covers?
For the purposes of Aetna’s coverage in its Medicare Advantage plans, the following services may be considered routine: Oral examinations in a dentist’s office. X-rays, including panoramic and bite wing views. Pulp vitality tests. Cleaning, scaling, and polishing the teeth. Oral hygiene consultations.
Does Aetna cover dental?
Do Medicare Advantage Plans from Aetna Cover Routine Dental Services? There is no coverage for routine dental services under Original Medicare ( Part A and Part B ); however, if you choose to receive your Part A and Part B benefits through the Medicare Part C program — through an Aetna Medicare Advantage plan, for example — you might get routine ...
Does Medicare cover dental care?
If you need dental services as part of Medicare-covered inpatient hospital treatment, or you need complex or emergency dental services, Medicare Part A may cover certain services while you are an inpatient in a hospital. These services, however, are not considered routine.
Does Aetna offer Medicare Advantage?
Keep in mind that not all plans may be offered in every city and state, and that benefits beyond Original Medicare – as well as costs – may vary from one Aetna Medicare Advantage plan to another. It’s also important to note that coverage may depend on staying with your plan’s network of preferred providers; your out-of-pocket costs may be higher if you go out-of-network for your care.
Is hospice covered by Medicare Advantage?
The only exception is hospice care, which is still covered by Part A. Medicare Advantage plans offer you an alternative way to access your Original Medicare benefits, but they are administered by private health insurance companies approved by Medicare. As such, each company, including Aetna, determines which extra benefits it will cover, if any, and your out-of-pocket costs for Medicare-covered services.
Does Medicare Offer Dental Coverage
No, Original Medicare, which is managed by the federal government, does not cover most routine dental care, dental procedures or supplies. People insured by Medicare have to pay the full cost of cleanings, fillings, tooth extractions and dentures.
Plan Benefits For 2022 Aetna Medicare Elite Plan
Aetna Medicare Elite Plan H5521-120 is a 2022 Medicare Advantage Plan or Medicare Part-C plan by Aetna Medicare available to residents in New York. This plan includes additional Medicare prescription drug coverage. The Aetna Medicare Elite Plan has a monthly premium of $0 and has an in-network Maximum Out-of-Pocket limit of $7,550 .
Best Online Tools: Humana
Humana is our top pick for a dental plan with robust online tools. They have a handy mobile app and allow users to list medications, view claims, and even earn rewards for healthy actions.
What Do Aetna Medicare Advantage Plans Offer
Aetna Medicare Advantage plans vary based on your location, but many plans offer opportunities to make access to your day-to-day necessities as simple as possible.
Can Aetna Medicare Plans Cover Additional Dental Services
Aetna Medicare Advantage plans that include dental benefits can cover preventive and routine services like exams, X-rays, cleanings and fluoride treatments, typically with a small copay or no copay at all required when performed by an in-network dentist.
Which Medicare Advantage Plans Offer Dental Coverage
Not all Medicare Advantage Plans offer dental coverage. When they do, the services can vary greatly, even within companies. A company may offer dental in one state, but not another, Hill says. If youre looking for dental, you can look up a specific company youre interested in and check with their network of dentists to see which one you like best.
Option : Medicare Advantage Plans With Dental Coverage
Dental coverage varies widely by Medicare Advantage plan. In some cases, you have to pay extra to have dental care included in your plan. There could also be options for basic or premium coverage, letting you choose the dental plan that works for you.
How to find out what dental plans are available in your area?
To see which plans are available in your area, visit the Medicare plan finder tool and enter your ZIP code. Read more about each plan to find out what dental services they offer, and check yearly allowances, copays, and monthly premiums.
Can you get dental insurance with Medicare Advantage?
If you qualify for Medicare Advantage, you qualify for dental coverage if they offer it.
Does Aetna cover dental services?
dentures or partials. Along with these benefits, Aetna Medicare dental coverage is the same as original Medicare, which includes dental services provided in a hospital, such as after a facial injury or due to oral cancer.
Does Medicare Advantage cover dental?
Medicare Advantage plans may offer dental coverage along with vision and hearing services. These policies also provide basic medical and prescription drug coverage.
Does Medicare cover dental insurance?
Does original Medicare provide dental coverage? Original Medicare does not provide coverage for routine dental care like oral exams and dental cleanings. Medicare Part A will offer benefits to cover specific dental procedures. If you need dental care due to an injury or illness, original Medicare may pay for it.
Does Aetna pay for out of network dentists?
If you visit an in-network dentist, they’ll bill Aetna directly. When you access out-of-network care, you’ll pay upfront and submit a claim with reimbursement up to your plan’s yearly allowance for dental services.
Can you tack on benefits to your Advantage plan?
You can tack on these other benefits to your Advantage plan premium and then pay for everything in one convenient bill.
Does Aetna offer prescription drug coverage?
Many of Aetna’s Medicare Advantage plans also include prescription drug coverage. Some plans also offer extra benefits, like routine dental or vision care, membership in fitness programs, or bathroom safety devices. Not every plan offers the same extra benefits, and some plans might not offer any extra benefits.
Does Aetna cover dental?
Aetna’s Medicare Advantage plans and dental coverage. Some of Aetna’s Medicare Advantage plans may include routine dental care. Why might that be important? Well, Original Medicare, Part A and Part B, don’t typically include routine dental care. Part A may cover certain dental services if you need them as part of your care as a hospital inpatient.
Is Aetna a PPO?
Aetna Medicare is a HMO , PPO plan with a Medicare contract. Our SNPs also have contracts with State Medicaid programs. Enrollment in our plans depends on contract renewal. This information is not a complete description of benefits. Call <TFN (TTY: 711)> for more information.
Network plans
These plans require you to see a network provider. You may have a different network for medical benefits than for dental, eyewear or hearing services. The EOC can help you find the right network for your plan.
Direct Member Reimbursement (DMR)
A DMR is an annual allowance to see any licensed provider in the U.S. that has not opted out of Medicare. Members will pay out of pocket and then submit a form to get reimbursed up to the plan’s allowance.
2022 Dental benefits
Plans that offer benefits through a network cover preventive care such as oral exams, cleanings and X-rays.* Some plans include comprehensive services such as fillings and extractions. You can find specific benefit information in the Evidence of Coverage.
What is preventive dental care?
The Preventive Dental Care Benefit (for members under 12 years of age) is a standard benefit in many Aetna HMO-based plans. In addition, some HMO-based medical plans include a dental services rider. Refer to the individual plan documents for a description of covered services;
What is covered by dental insurance?
Dental treatment needed to remove, repair, replace, restore or reposition natural teeth damaged, lost, or removed due to an injury occurring while the person is covered under the medical plan. Standard traditional plans also cover dental work to restore, repair, remove, reposition or replace] other body tissues of the mouth fractured or cut. Any such teeth must be free from decay, in good repair and firmly attached to the jawbone at the time of injury. In general, most plans require restoration or replacement in the calendar year of the accident or the next calendar year. Coverage requires prior authorization in plans that have such provisions. The cost of installing the first denture, crown, in-mouth appliance and/or fixed bridgework to replace teeth lost due to accidental injury. Orthodontic therapy used in the first course of treatment to correct a malocclusion caused by accidental injury (this does not include benefits for full mouth orthodontic therapy unless review by a dental director or OMS director authorizes coverage for these services). Charges for repairing or replacing the first free-standing crown or abutment for fixed bridge prostheses, but only when accidental injury requires re-preparation of the natural tooth. Note: Charges to remove, repair, replace, restore or reposition teeth lost or damaged in the course of biting or chewing are not covered medical expenses. Sound natural teeth are defined as teeth that were stable, functional, free from decay and advanced periodontal disease, and in good repair at the time of the accident.
Why is orthodontics considered medically necessary?
To be considered medically necessary, orthodontic services must be needed to treat, correct or ameliorate a medical defect or condition , and an essential part of an overall treatment plan developed by both the physician and the dentist in consultation with each other.
What are some examples of dental services?
Examples of dental services that are integral to medical procedures include the following: Extraction of teeth prior to radiation therapy of the head and neck. Note: Dental reconstruction for the replacement of extracted teeth is not covered by the medical plan.
What is the medical management of a child with cleft palate?
Medical management of children with cleft palate may involve what might otherwise be considered dental care. The following policies apply to the correction of this congenital defect.
Why is it important to remove broken teeth?
Removal of broken teeth necessary to reduce a jaw fracture.
Does Aetna cover facial bone fractures?
Reduction of any facial bone fractures is covered under all Aetna medical plans. Standard HMO and traditional plans cover the removal of tumors, treatment of dislocations, facial and oral wounds/lacerations, and removal of cysts or tumors of the jaws or facial bones, or other diseased tissues.
