What does EOB stand for in Medicare EOB?
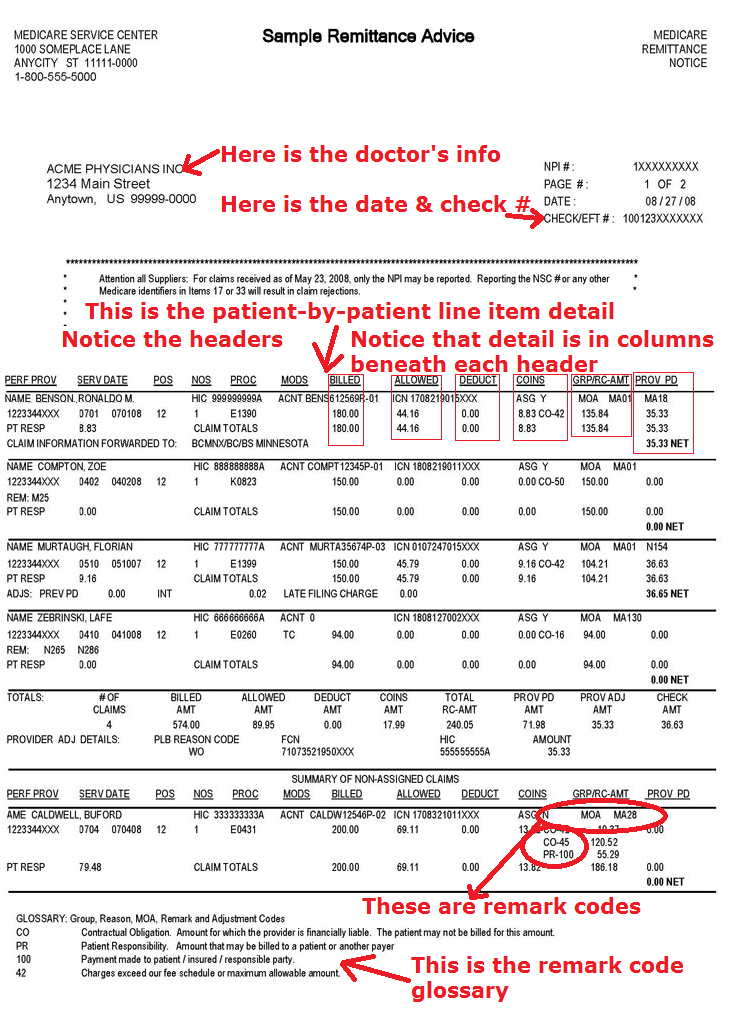
Medicare EOB - Detailed Review - Medical Billing and Coding - Procedure code, ICD CODE. Serv Date: This field provides the service from and to dates as well as the patient’s responsibility.
Does the insurance EOB correspond to the dates of service/services?
The Insurance EOB Does Not Correspond To The Dates Of Service/servicesBeing Billed. Denied. These Supplies/items Are Included In The Purchase Of The Dme Item Billed On The Same Date Of Service (DOS).
What is the difference between billed and covered on an EOB?
The difference is indicated in some way on the EOB, with either an amount not covered, or a total covered amount that's lower than the billed charge. Amount the Health Plan Paid: This is the amount that your health insurance plan actually paid for the services you received.
What does PLB FB mean in Medicare?
Used to reflect a balance being moved forward to a future remit or a balance that is brought forward from a prior Medicare Remittance Advice (RA). • When a balance is moving forward to a future RA, the PLB FB contains the check or Electronic Funds Transfer (EFT) trace number from the current 835 transaction.
When the monies can be recovered from future payment, the forwarding balance (FB) will be returned with the?
What is a FB on an 835?
What is the 835 PLB segment?
What does FCN mean in insurance?
What does negative mean on a Medicare remittance?
When the adjustment shows a corrected payment of less than the original claim payment, an FB reflects a answer?
What does forwarding balance mean?
See more

What does FB mean in medical billing?
FB – Forwarding Balance – Reflects the difference in the payment between the original claim and the overpayment/adjustment to the original claim.
What does wo mean on a Medicare remit?
MID ColumnContentDescriptionWOIf the A/R If the A/R CCN is NOT tied to an , the Medicare ID will correspond to the Medicare ID entered during setup of the A/R. If the Medicare ID is not entered during setup, the Medicare ID field will be blank.3 more rows•Mar 29, 2022
What is a provider level adjustment?
A Provider Level Adjustment is an option in MacPractice when addressing Insurance Payments where you can credit some or all of an insurance payment to a specific Provider. This is useful in situations where the Insurance may overpay due to being late in remitting payment, or other similar reasons.
What are claim adjustment reason codes?
Claim adjustment reason codes (CARCs) communicate an adjustment, meaning that they must communicate why a claim or service line was paid differently than it was billed.
What does adjustment code FB mean?
Forward BalanceForward Balance (FB) The FB amount does not indicate funds have been withheld from the provider's payment for this remittance advice. It only indicates that a past claim has been adjusted to a different dollar amount.
What is J1 on Medicare remit?
This remark code shows that we are changing the "status" of that service from "overpayment" to not an overpayment. The J1 message informs you that payment has been suppressed.
What is the difference between claim level and line level?
Data should be reported at the higher level with the Claim Level being the higher level and the Line Level being the lower level. Claim Level data reported is accepted for all lines of service in the claim and any information reported at the Line Level supersedes the data reported at the Claim Level.
What does CS adjustment mean?
CS – Adjustment This code is used to inform you that we have identified an overpayment of $50 or more. We recommend checking your books to confirm details. You may elect to submit a refund to BCBSIL, or do nothing, in which case the payment recovery will occur automatically.
What is a provider level balance?
Provider-Level Balance (PLB) Supplement to the Electronic Remittance Advice 835 Transaction Companion Guide. The PLB segment is used to transmit information about Provider-Level Adjustments - that is, payments and debts that are not specific to a particular claim or service.
What are reason codes?
Reason codes, also called score factors or adverse action codes, are numerical or word-based codes that describe the reasons why a particular credit score is not higher. For example, a code might cite a high utilization rate of available credit as the main negative influence on a particular credit score.
How do you read an EOB for dummies?
1:342:35How to Read Your Medical EOB - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe amount you pay for the service this is the amount that you will be billed. Remember the EOB isMoreThe amount you pay for the service this is the amount that you will be billed. Remember the EOB is not a bill it just shows you how the costs are distributed. If you have any questions by your EOB.
Where are claim adjustment reason codes found?
Locate the Adjustment Reason Codes in the last column on the right side of the claim line. Examples of Claim Adjustment Reason Codes are: 45 = $xx. xx; a common informational code letting providers know that their charges exceed the fee schedule maximum allowable by the amount indicated.
Forward balance and withholding | Medical Billing and Coding ...
All the contents and articles are based on our search and taken from various resources and our knowledge in Medical billing. All the information are educational purpose only and we are not guarantee of accuracy of information.
Provider-level adjustments basics - FB, WO, withholding, Internal ...
Locating PLBs • Provider-level adjustments can increase or decrease the transaction payment amount. • Adjustment codes are located in PLB03-1, PLB05-1, PLB07-1, PLB09-1, PLB11-1 and PLB13-1.
Reading your Explanation of Benefits - CMS
Customer service: 1-800-123-4567 Member name: description of the health care Address:
CMS Manual System Department of Health & Human Transmittal 812
CMS Manual System Department of Health & Human Services (DHHS) Pub 100-20 One-Time Notification Centers for Medicare & Medicaid Services (CMS) Transmittal 812 Date: November 12, 2010 Change Request 7068. SUBJECT: Instructions for PLB Code Reporting on Remittance Advice and a Crosswalk Between the
Medicare Part A Common Remittance Advice Questions
First Coast Service Options Page 8 of 14 “An FB is the amount that has been paid on a previously processed claim. This amount does not indicate funds have been withheld from the facility’s payment for that remittance advice.
Medicaid denial reason code list | Medicare denial codes, reason ...
Medicaid Claim Denial Codes 1 Deductible Amount 2 Coinsurance Amount 3 Co-payment Amount 4 The procedure code is inconsistent with the modifier used or a required modifier is missing.
What is the PLB in remittance?
Provider Level Balance (PLB) Reason Code Forward Balance (FB) The FB amount does notindicate funds have been withheld from the provider’s payment for this remittance advice. It only indicates that a past claim has been adjusted to a different dollar amount. The FB indicated does notchange the amount of the payment for this remittance advice. Financial Control Number (FCN): The adjusted claim internal control number (ICN) This number will match the invoice number listed on the attachment of the demand letter.
What is offset remittance advice?
The offset remittance advice is to inform you of the amount of money deducted from the total amount paid. The corresponding claim information must be found within the overpayment letter received or the previous notification remittance advices. Click the Next button to view a sample of the offset remittance advice.
How to find out if you overpaid a PLB?
You can locate information about your overpayment ($57.24) by notation of “FB” in the PLB reason code followed by the corresponding FCN and MID of the overpayment. This is located in the summary section of the remittance. However, no money has been deducted from this remittance payment for this claim. Roll your cursor over the highlighted green and orange boxes for more information.
What is the first notification remittance advice?
The first notification remittance advice displays the approved amount on the initial claim. Click the Next button to view a sample of the first notification remittance advice.
What is a PLB in Medicare?
Provider-Level Adjustment (PLB) reason codes describe adjustments the Medicare Contractor makes at the provider level, instead of a specific claim or service line. Some examples of provider-level adjustments include:
What does WO mean in a transaction?
WO prevents the prior claim payment from being deducted from the transaction.
When is a group medical plan used?
Used when the service provider is also the employer group and they request that monies be applied towards the Group Medical Plan coverage premium instead of the claim.
Is reference ID included in PLB L6?
No Reference ID is included with the PLB L6. The amount reported is a sum of the AMT*1 segments.
What is the billing field on Medicare?
Billed: This field also contains the billed amount per procedure. If the patient account number is reported on the claim, Medicare will display that number in this field.
What does NOS mean in billing?
NOS: The number of service field shows how many services were billed per procedure code.
What is bill amet?
Billed Amt: Total amount billed on the SPR.
What is claim information forwarded to?
Claim Information Forwarded To: This represents the patient’s secondary insurance carrier.
What is a serv date?
Serv Date: This field provides the service from and to dates as well as the patient’s responsibility.
What is the reference ID in PLB 72?
The Reference ID in the PLB 72 contains the beginning date of service from the claim and the patient account number (Commercial and Medicare Solutions platforms).
What is the value of a voided check in PLB?
When a check is voided, the amount of the voided check is reported as a positive value in the PLB WO and a negative value in the PLB 72.
When do we report a reversal of a claim?
When we identify a claim overpayment, we report a reversal to the original claim and a corrected claim if there are sufficient funds from other claim payments to recover the amount of the overpayment. If sufficient funds are not available, we handle the overpayment with a manual recovery process after a certain amount of time.
Is reference ID included in PLB L6?
No Reference ID is included with the PLB L6. The amount reported is a sum of the AMT*I segments.
What is EOB in Medicare?
An Explanation of Benefits (EOB) is the notice that your Medicare Advantage Plan or Part D prescription drug plan typically sends you after you receive medical services or items. You only receive an EOB if you have Medicare Advantage or Part D. An EOB is not the same as a Medicare Summary Notice.
Is EOB the same as Medicare?
An EOB is not the same as a Medicare Summary Notice. It is also important to remember that an EOB is not a bill. EOBs are usually mailed once per month. Some plans give you the option of accessing your EOB online. Your EOB is a summary of the services and items you have received and how much you may owe for them.
What is EOB in medical billing?
Your EOB is a window into your medical billing history. Review it carefully to make sure you actually received the service being billed, that the amount your doctor received and your share are correct, and that your diagnosis and procedure are correctly listed and coded.
What is EOB in healthcare?
Updated on July 19, 2020. An explanation of benefits (EOB) is a form or document provided to you by your insurance company after you had a healthcare service for which a claim was submitted to your insurance plan. Your EOB gives you information about how an insurance claim from a health provider (such as a doctor or hospital) ...
What does EOB mean for medical?
Your EOB will generally also indicate how much of your annual deductible and out-of-pocket maximum have been met. If you're receiving ongoing medical treatment, this can help you plan ahead and determine when you're likely to hit your out-of-pocket maximum. At that point, your health plan will pay for any covered in-network services you need for the remainder of the plan year.
What is EOB information?
Your EOB has a lot of useful information that may help you track your healthcare expenditures and serve as a reminder of the medical services you received during the past several years.
What is an EOB?
Your EOB gives you information about how an insurance claim from a health provider (such as a doctor or hospital) was paid on your behalf—if applicable—and how much you're responsible for paying yourself.
What does "not covered" mean on an EOB?
Not Covered Amount: The amount of money that your insurance company did not pay your provider. Next to this amount you may see a code that gives the reason the healthcare provider was not paid a certain amount. A description of these codes is usually found at the bottom of the EOB, on the back of your EOB, or in a note attached to your EOB. Insurers generally negotiate payment rates with healthcare provider, so the amount that ends up being paid (including the portions paid by the insurer and the patient) is typically less than the amount the provider bills. The difference is indicated in some way on the EOB, with either an amount not covered, or a total covered amount that's lower than the billed charge.
What is billed charge?
Charge (Also Known as Billed Charges): The amount your provider billed your insurance company for the service. Not Covered Amount: The amount of money that your insurance company did not pay your provider. Next to this amount you may see a code that gives the reason the doctor was not paid a certain amount.
What is EOB in Medicare?
An Explanation of Benefits (EOB) is the notice that your Medicare Advantage Plan or Part D prescription drug plan typically sends you after you receive medical services or items. It is also important to remember that an EOB is not a bill. EOBs are usually mailed once per month.
How do I get a copy of my Medicare summary notice?
Similarly, how do I get a copy of my Medicare Summary Notice? You can view and print your MSNs online at MyMedicare.gov by signing up for electronic MSNs (eM SNs). With eMSNs, you won't have to wait 3 months to get your paper MSNs. You'll get an email each month letting you know that your eMSNs are ready to view and print.
When the monies can be recovered from future payment, the forwarding balance (FB) will be returned with the?
When the monies can be recovered from future payment, the forwarding balance (FB) will be returned with the monies expressed as a positive. (To identify what claims are associated to the PLB where TRN02CheckA is referenced, refer back to the original 835 where TRN02CheckA first occurred.)
What is a FB on an 835?
The following applies in situations where the recoupment will occur at the time a reversed and corrected claim record populates the 835. When the adjustment is less than the original paid amount, the difference will be subtracted from the check. When the monies can’t be recovered in full, a forwarding balance (FB) is created in the PLB segment. Per the guide, the FB reference ID must be the current TRN02 (check number) value. The monies unable to be recovered will be identified as a forwarding balance (FB) with the monies expressed as a negative.
What is the 835 PLB segment?
835 Electronic Remittance Advice PLB Segment: TheASC X12 Standards for Electronic Data Interchange Technical Report Type 3 has specific rules for reporting overpayment recovery in the 835. The following information should be referenced to understand the formatting of the PLB segments of the 835 for recoupment of funds and when forward balance situations occur.
What does FCN mean in insurance?
FCN – Indicates the Financial Control Number (FCN) that this adjustment relates to when the adjustment refers to a claim that appeared on a previous RA. This usually matches the ICN field of a previous claim. If the adjustment in question does not relate to a previous claim, this field is left blank.
What does negative mean on a Medicare remittance?
A negative value represents a balance that will be moved forward to a future remittance payment advice. This means that an overpayment for a specific claim or claims (on this remittance) has been created because Medicare has paid for a service that should not have been allowed or has paid too much for a service. Your remittance notice will show the corrected allowed amounts for the adjusted claim (s).
When the adjustment shows a corrected payment of less than the original claim payment, an FB reflects a answer?
When the adjustment shows a corrected payment of less than the original claim payment, an FB reflects a negative amount. When the adjustment shows a corrected payment of more than the original claim payment, the FB reflects a positive amount.
What does forwarding balance mean?
Answer: Forwarding balance means that a negative value represents a balance moving forward to a future payment advice. A positive value represents a balance being applied from a previous RA. A reference number (the original ICN and HIC) is applied for tracking purposes.
