“GG” – “Performance and payment of a screening mammography and diagnostic mammography on same patient same day” – This is billed with the Diagnostic Mammography code to show the test changed from a screening test to a diagnostic test. Contractors will pay both the screening and diagnostic mammography tests.
What is section GG in nursing?
Section GG is a set of standardized patient assessment elements that the Improving Post-Acute Care Transformation Act (IMPACT) mandated for collection in all post-acute care settings. The items are meant to measure functional changes in self-care and mobility and will be publicly reported in the near future.
What does GG mean on a mammogram Bill?
“GG” – “Performance and payment of a screening mammography and diagnostic mammography on same patient same day” – This is billed with the Diagnostic Mammography code to show the test changed from a screening test to a diagnostic test. Contractors will pay both the screening and diagnostic mammography tests.
Is the care item set the same as section GG?
A: No. Section GG is required by CMS but the CARE Item Set is not. Section GG does contain CARE items, which is why some therapy providers are choosing to require staff to complete the CARE Item Set as well. Q: What are the differences between Section GG and the CARE Item Set?
What is a GG code for nursing home?
First, GG codes are a portion of the CMS, Resident Assessment Instrument, or RAI. According to the Centers for Medicare & Medicaid Services, Long-Term Care Facility Resident Assessment Instrument 3.0 User’s Manual: Version 1.16.

What does section GG stand for?
Section GG is a set of standardized patient assessment elements that the Improving Post-Acute Care Transformation Act (IMPACT) mandated for collection in all post-acute care settings. The items are meant to measure functional changes in self-care and mobility and will be publicly reported in the near future.
What is Section GG on MDS?
SECTION GG: FUNCTIONAL ABILITIES AND GOALS Intent: This section includes items about functional abilities and goals. It includes items. focused on prior function, admission performance, discharge goals, and discharge performance.
What is GG functional score?
Section GG scoring states that the higher the score, the more independent the resident is. Additionally in section GG, several items are combined to determine an average score.
What is the difference between Section G and Section GG?
Section G: The guidance is to code the most amount of assistance provided within a 7 day look-back. In Section GG: Guidelines are to code the baseline performance ability within the first three days following admission and before treatment begins.
Is GG the same as care tool?
A: No. Section GG is required by CMS but the CARE Item Set is not. Section GG does contain CARE items, which is why some therapy providers are choosing to require staff to complete the CARE Item Set as well.
When should GG tab be completed?
For an eval only that is completed at least 2 days after the facility admission, Rehab Optima will require an admission GG assessment and discharge GG assessment to be completed. For this situation enter dashes in all performance areas.
How do I use a GG code?
4:371:59:51Section GG: Functional Abilities and Goals - YouTubeYouTubeStart of suggested clipEnd of suggested clipCode one dependent if the helper completed the activities. For the patient or the assistance of twoMoreCode one dependent if the helper completed the activities. For the patient or the assistance of two or more helpers was required for the patient to complete the activities.
What are the 5 levels of assistance?
Levels of AssistanceDependent: During dependent mobility, you are unable to help at all. ... Maximal Assist: ... Moderate Assist: ... Minimal Assist: ... Contact Guard Assist: ... Stand-by Assist: ... Independent:
What is the range for nursing function score?
0 through 24The PDPM Function Score for PT Payment ranges from 0 through 24.
What is the care tool?
The Continuity Assessment Record and Evaluation (CARE) Item Set: As a part of the Medicare Post-Acute Care Payment Reform Demonstration (PAC-PRD), a standardized patient assessment tool was developed for use at acute hospital discharge and at post-acute care admission and discharge.
What is the time frame for the admission performance period for section GG0130 and GG0170?
three-dayGG0130 Self-Care and GG0170 Mobility Steps for Assessment Assess the resident's performance based on direct observation, incorporating resident self-reports and reports from qualified clinicians, care staff, or family documented in the resident's medical record during the three-day assessment period.
Who is supposed to report and enter information into Section GG?
CMS expects that MDS data will be collected and entered by Qualified Clinicians. CMS describes who the Qualified Clinician is on page GG-9 of the Centers for Medicare & Medicaid Services, Long-Term Care Facility Resident Assessment Instrument 3.0 User’s Manual. Version 1.16. October 2018: “…Healthcare professionals practicing within their scope of practice and consistent with Federal, State, and local law and regulations”.
What is the purpose of MDS and GG codes?
MDS and GG codes help CMS understand the functional abilities and progress of patients receiving post-acute care. Data must be entered into the MDS by Qualified Clinicians. Historically, the MDS nursing staff entered this data, and the training material and RAI manual provided by CMS continue to utilize language that continues to support this practice; however, the definition of Qualified Clinician could allow a therapist to be the designated person to enter this data.
How long is the CMS assessment period?
CMS anticipates that an interdisciplinary team of qualified clinicians is involved in assessing the resident during the three-day assessment period.
What is Section G guidance?
Section G: The guidance is to code the most amount of assistance provided within a 7 day look-back.
Is feeding tube considered a section GG?
Guidelines instruct to score admission performance and discharge goal for “Eating” as: The ability to use suitable utensils, to bring food and/or liquid to the mouth, and swallow food and/or liquid once the meal is placed before a resident. Intake via feeding tube is not a consideration in Section GG, as it is in Section G.
Who is responsible for completing Section GG?
Thus, the SNF is ultimately responsible for completing Section GG. However, due to the nature of the requirements, all core staff (including therapy) working with patients will be affected.
How many alpha scores does Section GG have?
Section GG has three numeric score options that can be used to classify the reasons for an activity not being attempted, whereas the CARE Item Set has four alpha scores. Section GG includes a slightly different set of items than are used in the CARE Item Set.
What is the QRP measure?
This requirement is met by documenting at least one discharge goal item on Section GG for at least one self care or mobility item. The discharge goal does not have to be created by therapy (in some cases, that would not be appropriate) and should be based on results of the initial Section GG assessment and collaboration with the care plan team.
Do you have to complete GG on Medicare?
A: Section GG must be completed on Medicare A PPS patients.
Is GG required by CMS?
A: No. Section GG is required by CMS but the CARE Item Set is not. Section GG does contain CARE items, which is why some therapy providers are choosing to require staff to complete the CARE Item Set as well.
What is GH modifier?
This modifier is for tracking purposes only. “ GH ” – “Diagnostic mammogram converted from screening mammogram on same day.”.
What are the modifiers for mammography?
Mammography Services modifier s GG AND GH. A radiologist who interprets a screening mammography is allowed to order and interpret additional films based on the results of the screening mammogram while the beneficiary is still at the facility for the screening exam.
Is a GH claim a screening?
Statistics will be collected based on the presence of modifier “-GH.” The claim will be billed and paid as a diagnostic mammography instead of a screening mammography. However, since the original intent for the exam was for screening, for statistical purposes, the claim is considered a screening.
What do the Medicare letters mean?
The four different parts of Medicare are each identified by a letter: A, B, C and D. The number displayed on your Medicare card, however, is known as the Medicare Beneficiary Identifier and is randomly generated for you.
What do the letters on my Medicare card mean?
What do the letters on your Medicare card mean? The Medicare number displayed on Medicare cards (known as an MBI, or Medicare Beneficiary Identifier) is 11 characters long: The 2nd, 5th, 8th and 9th characters are always a letter, and the 3rd and 6th characters are sometimes a letter. All other characters will be numbers, and the letters S, L, O, ...
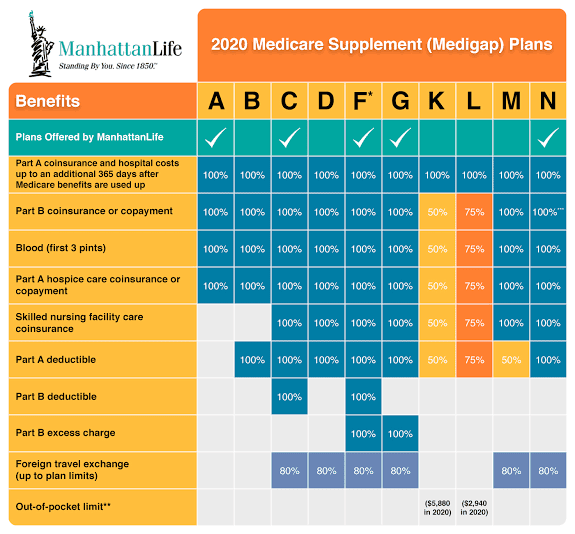
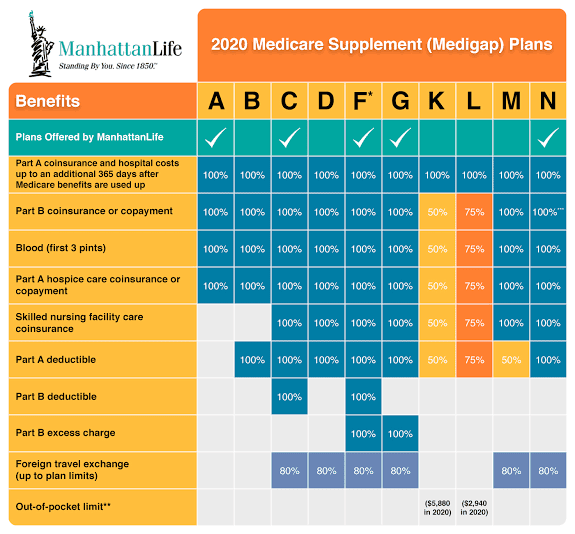
What is Medicare Supplement Insurance?
Medicare Supplement Insurance, also called Medigap, uses a letter system to identify its plans. Medicare Supplement Insurance is used in conjunction with Part A and Part B of Medicare to provide coverage for certain out-of-pocket expenses like some Medicare deductibles and coinsurance.
How many Medicare Supplement Plans are there?
There are 10 Medicare Supplement Plans to choose from, identified by letters: Plan A, B, C, D, F, G, K, L, M and N. Note that Medigap coverage options are referred to as “plan” (e.g., Medigap Plan A) as opposed to “part” (Medicare Part A hospital insurance).
What is Medicare Part B?
Medicare Part B is medical insurance and provides coverage for outpatient doctor’s appointments and medical devices. Medicare Part C, also known as Medicare Advantage, provides coverage for everything found in Part A and Part B through one plan provided by a private insurer.
How many parts of Medicare are there?
The four different parts of Medicare are each identified by a letter.
Does Medicare cover dental insurance?
Many Medicare Advantage plans may also cover additional benefits not covered by Part A and Part B, such as prescription drugs, dental, vision, hearing, wellness programs like SilverSneakers and more. Medicare Part D provides coverage exclusively for prescription drugs.