The GZ modifier indicates that an ABN was not issued to the beneficiary and signifies that the provider expects denial due to a lack of medical necessity based on an informed knowledge of Medicare policy. According to this guidance from HHS OGC, an automated edit shall be established to deny Part A and B claim line(s) items that contain a GZ modifier.
What does GZ stand for in slang?
Jul 07, 2010 · This modifier is used to obtain a denial on a non-covered service. Use this modifier to notify Medicare that you know this service is excluded. GZ Modifier: Item or Service Expected to Be Denied as Not Reasonable and Necessary. This modifier should be applied when an ABN may be required but was not obtained.
What are the Ga, gx, gy and GZ modifiers?
Feb 27, 2020 · Modifier GZ Definition The provider expects a medical necessity denial, however, did not provide an Advance Beneficiary Notice of Noncoverage (ABN) to the patient. The line item containing the GZ modifier is denied provider-liable. Appropriate Usage Append when no ABN was provided to beneficiary and services are not medically necessary
What does GZ mean in text?
NOTE: The GZ modifier is provided for physicians and suppliers that wish to submit a claim to Medicare, that know that an ABN should have been signed but was not, and that do not want any risk of allegation of fraud or abuse for claiming services that are not medically necessary. By notifying Medicare, by the GZ modifier, that you
What is G0 modifier used for?
Aug 17, 2016 · GZ Modifier * The GZ modifier is used when you expect Medicare to deny the service and you do not have an ABN form signed. * Use this modifier when you forgot the ABN. * Expect an audit if you use this modifier Q6 Modifier * Services provided by a Locum Tenens physician * Use this modifier when you have another doctor filling in for you.
What is mod GZ?
GZ Modifier: Item or Service Expected to Be Denied as Not Reasonable and Necessary. This modifier should be applied when an ABN may be required but was not obtained.
When should a GZ modifier be used?
1.1 (Instructions for Codes With Modifiers (Carriers Only)), Part E, (Coding for Noncovered Services and Services Not Reasonable and Necessary) states, “The GZ modifier must be used when physicians, practitioners, or suppliers want to indicate that they expect that Medicare will deny an item or service as not ...Feb 4, 2011
Is GZ modifier only for Medicare?
GZ Modifier - Item or Service Expected to Be Denied as Not Reasonable and Necessary. Use this modifier to report when you expect Medicare to deny payment of the item or service due to a lack of medical necessity and no ABN was issued. This modifier is an informational modifier only.Feb 13, 2017
Can we bill patient for GZ modifier?
The GZ modifier identifies that 1) an item or service is expected to be denied as not reasonable and necessary, and 2) no advance notice of non-coverage was supplied to the member. If you bill us for services using the GZ modifier, the claim will go to provider liability and you may not bill the member.
What does GX modifier mean for Medicare?
Modifier GX The GX modifier is used to report that a voluntary Advance Beneficiary Notice of Noncoverage (ABN) has been issued to the beneficiary before/upon receipt of their item because the item was statutorily noncovered or does not meet the definition of a Medicare benefit.May 7, 2018
What are Medicare modifiers?
Modifiers can be two digit numbers, two character modifiers, or alpha-numeric indicators. Modifiers provide additional information to payers to make sure your provider gets paid correctly for services rendered.Mar 3, 2022
Can you bill Kx and Ga modifiers together?
Since the KX modifier, in most cases, should be added to a HCPCS code "only if all of the coverage criteria outlined in the Indications and Limitations of Coverage section of the applicable policy have been met," the bulletin notes that "in most cases it would not be appropriate to append the GA and KX modifiers on the ...Sep 14, 2011
What does GY modifier indicate?
Adding the GY HCPCS modifier to the CPT code indicates that an “item or service is statutorily excluded or the service does not meet the definition of Medicare Benefit.” This will automatically create a denial and the beneficiary may be liable for all charges whether personally or through other insurance.Jun 6, 2021
What does statutorily non covered Mean?
-GY – Item or service statutorily excluded, does not meet the definition of any Medicare benefit or for non-Medicare insurers, and is not a contract benefit.
What is the difference between modifier 59 and Xu?
Effective January 1, 2015, XE, XS, XP, and XU are valid modifiers. These modifiers give greater reporting specificity in situations where you used modifier 59 previously. Use these modifiers instead of modifier 59 whenever possible. (Only use modifier 59 if no other more specific modifier is appropriate.)
What is the difference between GA and GX modifier?
Modifier Modifier Definition Modifier GA Waiver of Liability Statement Issued as Required by Payer Policy. Modifier GX Notice of Liability Issued, Voluntary Under Payer Policy. Modifier GY Notice of Liability Not Issued, Not Required Under Payer Policy.Jul 14, 2021
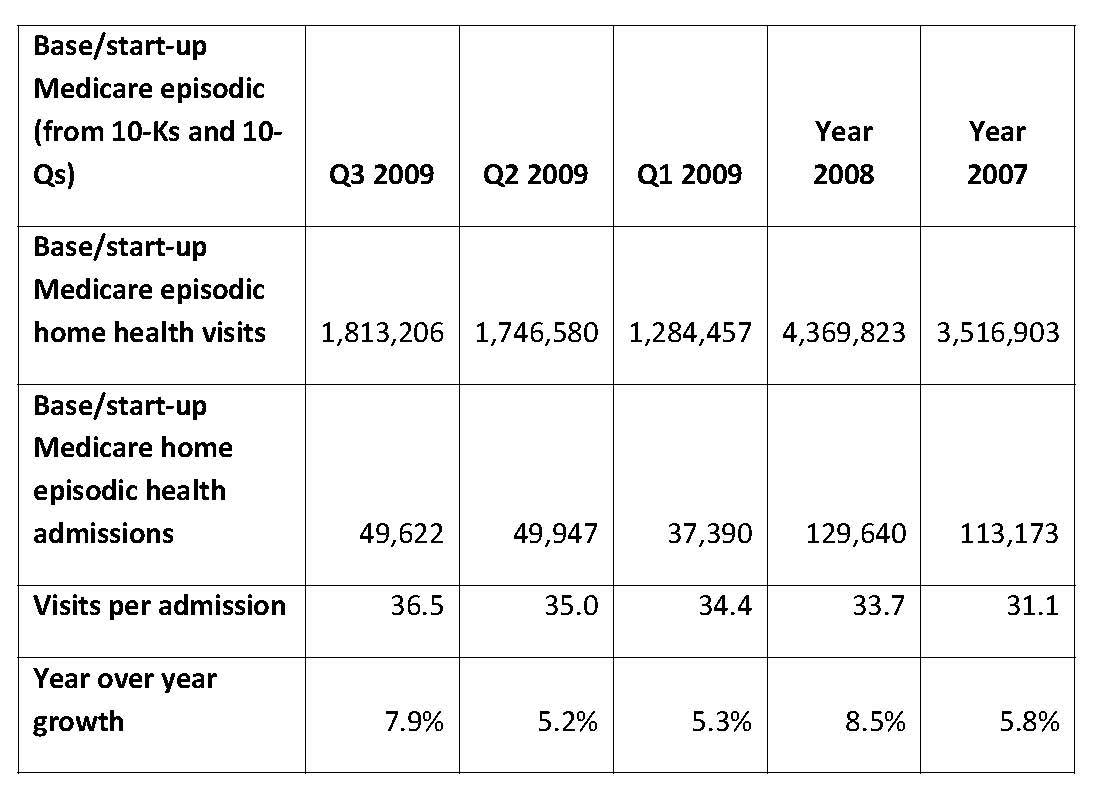
What is the percentage of beneficiaries who are in the original Medicare plan?
Currently, 44 million beneficiaries—some 15 percent of the U.S. population—are enrolled in the Medicare program. Enrollment is expected to rise to 79 million by 2030. Only one in 10 beneficiaries relies solely on the Medicare program for health care coverage.
When to use GZ modifier?
The GZ modifier must be used when physicians, practitioners, or suppliers want to indicate that they expect that Medicare will deny an item or service as not reasonable and necessary and they have not had an Advance Beneficiary Notification (ABN) signed by the beneficiary.
When did Medicare allow gy modifiers?
Beginning in January 2002, Medicare allowed providers and suppliers to use the GY modifier to indicate that a service or item is not covered by Medicare, either because it is statutorily excluded (e.g., hearing aids) or does not meet the definition of any Medicare benefit (e.g., surgical dressings that are used to clean or protect intact skin).9
What is a GY modifier?
GY – Item or service statutorily excluded or does not meet the definition of any Medicare benefit. GZ – Item or service expected to be denied as not reasonable and necessary. 2. Use of the GA, GY, and GZ Modifiers for Services Billed to Local Carriers. The GY modifier must be used when physicians, practitioners, ...
What is the A9270 code?
However, in cases where there is no specific procedure code for an item or supply and no appropriate NOC code available, the A9270 must continue to be used by suppliers to bill DMERCs for statutorily non-covered items and items that do not meet the definition of a Medicare benefit. 5. Claims Processing Instructions.
Can Medicare exclude home infusion?
These are statutorily excluded services. For services that Medicare does not allow, such as home infusion, providers need only file statutorily excluded services directly to their local plan using the GY modifier and will no longer have to submit to Medicare for consideration.
What is the GA modifier?
This GA modifier is to notify Medicare from provider that ABN is on file, and provider anticipates Medicare probably or certainly will not to cover those item or service. So by this provider indicates that patient has signed ABN form by appending GA modifier to CPT and patient will be responsible for the charges billed, if those items or service not covered by Medicare.
Why do you need to add GA modifier to CPT?
GA modifier should be append to a CPT, for which the provider had a patient sign an ABN form because there is a possibility the service may be denied because the patient’s diagnosis might not medically necessary. By this provider ensure upon Medicare denial, member will be liable to pay those services.
What is an ABN for Medicare?
ABN is also known as Waiver of Liability, signed by Medicare patients. In other way we can say a notice the hospital or doctor gives the patient before the treatment, telling the patient that Medicare may not pay for some treatment or services. This ABN document is signed by the patient, stating that, in case of Medicare is not going to pay, or not covering the payment, the patient himself is liable for the payment.
Can you use ABN modifiers on Medicare Advantage?
ABN modifiers are prohibited for Medicare advantage enrollees. As per CMS, dated on May 05, 2014 released that Advance Beneficiary notice modifiers i.e. GA, GX, GY or GZ to be used only for Medicare beneficiaries and not to be used for members of Medicare advantage plans.
Does Medicare cover CPT 15775?
CPT 15775 and 15776 performed for cosmetic reason will be denied as non-covered. Medicare does not cover cosmetic surgery codes that are performed to reshape or improve the beneficiary appearance.
What is a GZ modifier?
The GZ modifier indicates that an ABN was not issued to the beneficiary and signifies that the provider expects denial due to a lack of medical necessity based on an informed knowledge of Medicare policy. According to this guidance from HHS OGC, an automated edit shall be established to deny Part A and B claim line(s) items that contain a GZ modifier.
When to use modifier 26?
Modifier 26 is used when reporting the physician component of a service separately. If this modifier is used with a Column II code that is reported with a Column I code, carriers deny the Column II code with the modifier.
What is the appropriate CPT code to bill?
When cytopathology codes are billed, the appropriate CPT code to bill is that which describes, to the highest level of specificity, what services were rendered. Accordingly, for a given specimen, only one code from a family of progressive codes (subsequent codes include services described in the previous CPT code, e.g., 88104-88107, 88160-88162) is to be billed. If multiple services on different specimens are billed, the “-91” modifier should be used to indicate that different levels of service were provided for different specimens. This should be reflected in the cytopathologic reports.
What is the CPT code for chemotherapy?
It is recognized that frequently combination chemotherapy is provided by different routes at the same session. When this is the case, using the CPT codes 96408, 96410, and 96414, the “-59” modifier (different substance) should be attached to the lesser valued technique indicating that separate agents were administered by different techniques.
What does 59 mean in medical terms?
Definition - The “-59” modifier is used to indicate a distinct procedural service. The physician may need to indicate that a procedure or service was distinct or independent from other services performed on the same day. This may represent a different session or patient encounter, different procedure or surgery, different site, or organ system, separate incision/excision, or separate injury (or area of injury in extensive injuries).
Does the revision date apply to red italicized material?
Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents.