Medicare Allowed Amount Definition Maximum amount on which payment is based for covered health care services. This may be called “eligible expense,” “payment allowance” or “negotiated rate.” If your provider charges more than the medicare allowed amount, patient no need to pay that amount when they are participating with Medicare insurance.
What factors determine Medicare rates?
Medigap Premium Rates Are Impacted by Multiple Factors
- Your Gender. You might have been unaware that your gender can be a determining factor in your Medigap rates. ...
- Your Age. Depending on the rating method used by your Medigap carrier, your age may be used to determine your rates.
- Tobacco Use. ...
- Household Discounts. ...
- Rate Increase History. ...
- Rate Locks. ...
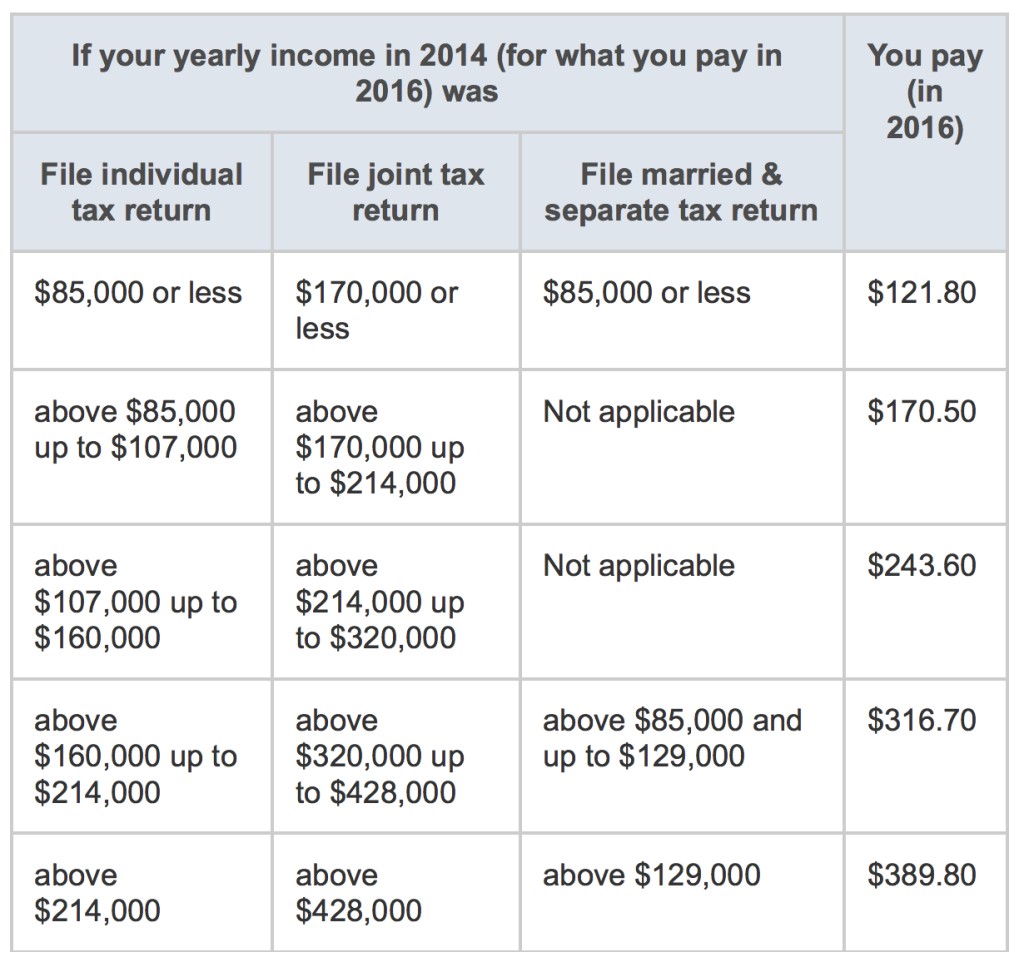
What are the Medicare premiums and coinsurance rates?
If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $259 ($274 in 2022). Days 91 and beyond: $742 ($778 for 2022) coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime)
What is the Medicare PFS payment rates formula?
The Medicare PFS payment rates formula shows how a payment rate for an individual service is determined, and we provide a description for each component below the formula. Each of the three RVUs are adjusted to account for geographic variations in the costs of practicing medicine in different areas within the country.
What is the maximum rate payable?
- (1) DHS uses the United States Office of Personnel Management 's salary rates, computed under 5 U.S.C. 5504, as the basis for the maximum pay rate schedule. ...
- (2) The Office of Personnel Management (OPM) publishes salary and locality pay schedules each calendar year. (i) Physicians. ...
- (3) Review and update. ...
- (4) Initial rates and subsequent revisions. ...
What is Medicare allowable rate?
The allowable fee for a non-participating provider is reduced by five percent in comparison to a participating provider. Thus, if the allowable fee is $100 for a participating provider, the allowable fee for a non-participating provider is $95. Medicare will pay 80% of the $95.
How do I find the Medicare allowable rate?
You can search the MPFS on the federal Medicare website to find out the Medicare reimbursement rate for specific services, treatments or devices. Simply enter the HCPCS code and click “Search fees” to view Medicare's reimbursement rate for the given service or item.
What is the Medicare allowable for 99213?
CPT CODE 2016 Fee 2017 FEE99201$35.96 $43.699205$169.54 $208.299211$20.07 $19.6399212$37.17 $43.199213$58.89 $72.75 more rows
What are Medicare Part B payments based on and how is the allowable charge calculated?
What are the Medicare Part B payments based on, and how is the allowable charge calculated? It is based on diagnosis- related group (DRG's), they determine appropriate reimbursement.
What is the 2021 Medicare conversion factor?
$34.8931This represents a 0.82% cut from the 2021 conversion factor of $34.8931. However, it also reflects an increase from the initial 2022 conversion factor of $33.5983 announced in the 2022 Medicare physician fee schedule final rule.
What is the Medicare allowable for 99214?
A 99214 pays $121.45 ($97.16 from Medicare and $24.29 from the patient). For new patient visits most doctors will bill 99203 (low complexity) or 99204 (moderate complexity) These codes pay $122.69 and $184.52 respectively.
What is the Medicare allowable rate for 99215?
Procedure Code 99215 Reimbursement Rates – MedicareCPT CodeService TimeRate9921210 minutes$46.139921315 minutes$68.109921425 minutes$110.439921540 minutes$148.33
How Much Does Medicare pay for a routine office visit?
Medicare Part B covers 80 percent of the cost of doctor's visits for preventive care and medically necessary services. Not all types of doctors are covered. In order to ensure coverage, your doctor must be a Medicare-approved provider.
What Are Medicare Reimbursement Rates?
Medicare reimburses health care providers for services and devices they provide to beneficiaries. Learn more about Medicare reimbursement rates and how they may affect you.
What percentage of Medicare is reimbursed?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare’s reimbursement rate on average is roughly 80 percent of the total bill. 1. Not all types of health care providers are reimbursed at the same rate.
What is Medicare coded number?
Medicare uses a coded number system to identify health care services and items for reimbursement. The codes are part of what’s called the Healthcare Common Procedure Coding System (HCPCS).
Is it a good idea to use HCPCS codes?
Using HCPCS codes. It’s a good idea for Medicare beneficiaries to review the HCPCS codes on their bill after receiving a service or item. Medicare fraud does happen, and reviewing Medicare reimbursement rates and codes is one way to help ensure you were billed for the correct Medicare services.
Why is Medicare fee higher than non-facility rate?
In general, if services are rendered in one's own office, the Medicare fee is higher (i.e., the non-facility rate) because the pratitioner is paying for overhead and equipment costs. Audiologists receive lower rates when services are rendered in a facility because the facility incurs ...
How to get Medicare fee schedule?
You may request a fee schedule adjusted for your geographic area from the Medicare Administrative Contractor (MAC) that processes your claims. You can also access the rates for geographic areas by going to the CMS Physician Fee Schedule Look-Up website. In general, urban states and areas have payment rates that are 5% to 10% above the national average. Likewise, rural states are lower than the national average.
What is the Medicare Physician Fee Schedule?
The Medicare Physician Fee Schedule (MPFS) uses a resource-based relative value system (RBRVS) that assigns a relative value to current procedural terminology (CPT) codes that are developed and copyrighted by the American Medical Association (AMA) with input from representatives of health care professional associations and societies, including ASHA. The relative weighting factor (relative value unit or RVU) is derived from a resource-based relative value scale. The components of the RBRVS for each procedure are the (a) professional component (i.e., work as expressed in the amount of time, technical skill, physical effort, stress, and judgment for the procedure required of physicians and certain other practitioners); (b) technical component (i.e., the practice expense expressed in overhead costs such as assistant's time, equipment, supplies); and (c) professional liability component.
Why do audiologists get lower rates?
Audiologists receive lower rates when services are rendered in a facility because the facility incurs overhead/equipment costs. Skilled nursing facilities are the most common applicable setting where facility rates for audiology services would apply because hospital outpatient departments are not paid under the MPFS.
What is RVU in Medicare?
The Centers for Medicare and Medicaid Services (CMS) determines the final relative value unit (RVU) for each code, which is then multiplied by the annual conversion factor (a dollar amount) to yield the national average fee. Rates are adjusted according to geographic indices based on provider locality. Payers other than Medicare that adopt these relative values may apply a higher or lower conversion factor.
What are the two categories of Medicare?
There are two categories of participation within Medicare. Participating provider (who must accept assignment) and non-participating provider (who does not accept assignment). You may agree to be a participating provider (who does not accept assignment). Both categories require that providers enroll in the Medicare program.
Do you have to bill Medicare for a physician fee?
You may agree to be a participating provider with Medicare. Once enrolled, you are required to bill on an assignment basis and accept the Medicare allowable fee as payment in full. Medicare will accept 80% of the allowable amount of the Medicare Physician Fee Schedule (MPFS) and the patient will pay a 20 % co-insurance at the time services are rendered or ask you to bill their Medicare supplemental policy. Both participating and non-participating providers are required to file the claim to Medicare.
What is Medicare reimbursement rate?
The reimbursement rates are the monetary amounts that Medicare pays to health care providers, hospitals, laboratories, and medical equipment companies for performing certain services and providing medical supplies for individuals enrolled in Medicare insurance. To receive reimbursement payments at the current rates established by Medicare, health care professionals and service companies need to be participants in the Medicare program. While non-participating professionals and companies are able to submit claims and receive reimbursements for their services, their reimbursements will be slightly lower than the rates paid to participants.
How much does Medicare pay for medical services?
The Medicare reimbursement rates for traditional medical procedures and services are mostly established at 80 percent of the cost for services provided. Some medical providers are reimbursed at different rates. Clinical nurse specialists are paid 85 percent for most of their billed services and clinical social workers are paid 75 percent ...
What is the Medicare coinsurance?
Today, Medicare enrollees who use the services of participating health care professionals will be responsible for the portion of a billing claim not paid by Medicare. The majority of enrollee responsibility will be 20 percent, often referred to as coinsurance. With clinical nurse specialists that responsibility would be 15 percent and 25 percent for clinical social workers.
How many specialists are on the Medicare committee?
Medicare establishes the reimbursement rates based on recommendations from a select committee of 52 specialists. The committee is composed of 29 medical professionals and 23 others nominated by professional societies.
Why use established rates for health care reimbursements?
Using established rates for health care reimbursements enables the Medicare insurance program to plan and project for their annual budget. The intent is to inform health care providers what payments they will receive for their Medicare patients.
What percentage of Medicare bill is not paid?
The majority of enrollee responsibility will be 20 percent , often referred to as coinsurance.
What is Medicare establishment rate schedule?
The establishment rate schedules are complex, multifunctional, and revised annually. The schedules for Medicare reimbursement rates are pre-determined base rates developed using a variety of factors that include the following.
What Is the Average Medicare Reimbursement Rate?
The Medicare reimbursement rate varies according to the service or item being provided as well as the type of health care provider that is delivering the care and other factors.
How much more can a health care provider charge than the Medicare approved amount?
Certain health care providers maintain a contract agreement with Medicare that allows them to charge up to 15% more than the Medicare-approved amount in what is called an “excess charge.”.
What is the coinsurance rate for Medicare Part B?
Looking up the reimbursement rates can also help you calculate how much you can expect to be billed for using the standard 20% coinsurance rate that applies to most services and items covered by Medicare Part B .
What is a CPT code?
CPT codes are the numeric codes used to identify different medical services, procedures and items for billing purposes. When a health care provider bills Medicare to seek reimbursement, they will use CPT codes to list the various treatments they delivered. The CPT codes used to bill for medical services and items are part ...
How many digits are in a CPT code?
CPT codes consist of 5 numeric digits, while HCPCS codes are an alphabetical number followed by 4 numeric digits.
How many Medicare codes can you enter at once?
You may enter up to five codes at a time or a range of codes. You may also select either the national payment amount or a specific Medicare Administrative Contractor (MAC), as reimbursement rates can vary within specific localities.
How much does Medicare pay for coinsurance?
In fact, Medicare’s reimbursement rate is generally around only 80% of the total bill as the beneficiary is typically responsible for paying the remaining 20% as coinsurance. Medicare predetermines what it will pay health care providers for each service or item. This cost is sometimes called the allowed amount but is more commonly referred ...
What percentage of Medicare deductible is paid?
After you have met your Part B deductible, Medicare will pay its portion of the approved amount. However, under Part B, you still owe 20 percent of the Medicare-approved amount for all covered items and services.
How much is Medicare Part A deductible?
If you have original Medicare, you will owe the Medicare Part A deductible of $1,484 per benefit period and the Medicare Part B deductible of $203 per year. If you have Medicare Advantage (Part C), you may have an in-network deductible, out-of-network deductible, and drug plan deductible, depending on your plan.
How does the Medicare-approved amount work?
To understand exactly what the Medicare-approved amount refers to, it’s important to also understand the difference between different types of Medicare providers.
What is Medicare Advantage?
Medicare Part B covers you for outpatient medical services. Medicare Advantage covers services provided by Medicare parts A and B, as well as: prescription drugs. dental.
What are the services covered by Medicare?
No matter what type of Medicare plan you enroll in, you can use Medicare’s coverage tool to find out if your plan covers a specific service, test, or item. Here are some of the most common Medicare-approved services: 1 mammograms 2 chemotherapy 3 cardiovascular screenings 4 bariatric surgery 5 physical therapy 6 durable medical equipment
What is excess charge for Medicare?
These excess charges can cost up to an additional 15 percent of the Medicare-approved amount. If you have a Medigap plan, this amount may be included in your coverage.
Does Medicare bill for coinsurance?
The provider will bill Medicare for your services and only charge you the deductible and coinsurance amount specified by your plan. The Medicare-approved amount may be less than the participating provider would normally charge. However, when the provider accepts assignment, they agree to take this amount as full payment for the services.
What is the allowed amount for out of network health insurance?
If you used an out-of-network provider, the allowed amount is the price your health insurance company has decided is the usual, customary, and reasonable fee for that service. An out-of-network provider can bill any amount he or she chooses and does not have to write off any portion of it. Your health plan doesn’t have a contract with an out-of-network provider, so there’s no negotiated discount. But the amount your health plan pays will be based on the allowed amount, not on the billed amount. And that's assuming your health plan covers out-of-network care at all. Some do not, unless it's an emergency situation.
What is balance billing?
This is called balance billing and it can cost you a lot. (In some circumstances, the balance bill comes as a surprise to the patient, because they were using an in-network hospital and didn't realize that one or more of the physicians (or other healthcare providers) who provided treatment was actually out-of-network.
How much coinsurance do you have to pay for out of network care?
Let’s say your health plan requires that you pay 50% coinsurance for out-of-network care. Without a pre-negotiated contract, an out-of-network provider could charge $100,000 for a simple office visit. If your health plan didn’t assign an allowed amount, it would be obligated to pay $50,000 for an office visit that might normally cost $250.
Do you have to make up the difference between the allowed amount and the actual amount billed?
You don’t have to make up the difference between the allowed amount and the actual amount billed when you use an in-network provider; your provider has to just write off whatever portion of their billed amount that's above the allowed amount. That’s one of the consumer protections that comes with using an in-network provider.
Does my insurance pay for anything above my deductible?
And if it's a service for which the deductible is applicable and you've already met your deductible, your insurer will pay some or all of the bill.) Anything billed above and beyond the allowed amount is not an allowed charge. The healthcare provider won’t get paid for it, as long as they're in your health plan's network.
Standard 20% Co-Pay
- All Part B services require the patient to pay a 20% co-payment. The MPFS does not deduct the co-payment amount. Therefore, the actual payment by Medicare is 20% less than shown in the fee schedule. You must make "reasonable" efforts to collect the 20% co-payment from the beneficiary.
Non-Participating Status & Limiting Charge
- There are two categories of participation within Medicare. Participating provider (who must accept assignment) and non-participating provider (who does not accept assignment). You may agree to be a participating provider (who does not accept assignment). Both categories require that providers enroll in the Medicare program. You may agree to be a participating provider with …
Facility & Non-Facility Rates
- The MPFS includes both facility and non-facility rates. In general, if services are rendered in one's own office, the Medicare fee is higher (i.e., the non-facility rate) because the pratitioner is paying for overhead and equipment costs. Audiologists receive lower rates when services are rendered in a facility because the facility incurs overhead/equipment costs. Skilled nursing facilities are the …
Geographic Adjustments: Find Exact Rates Based on Locality
- You may request a fee schedule adjusted for your geographic area from the Medicare Administrative Contractor (MAC) that processes your claims. You can also access the rates for geographic areas by going to the CMS Physician Fee Schedule Look-Up website. In general, urban states and areas have payment rates that are 5% to 10% above the national average. Likewise, r…
Multiple Procedure Payment Reductions
- Under the MPPR policy, Medicare reduces payment for the second and subsequent therapy, surgical, nuclear medicine, and advanced imaging procedures furnished to the same patient on the same day. Currently, no audiology procedures are affected by MPPR.