Most people over age 65 are eligible for Medicare coverage. You must be a U.S. citizen or a legal permanent resident for at least 5 consecutive years. Certain people under 65 may be eligible for Medicare, if they meet specific criteria.
Who is eligible for Medicare at 62?
You qualify for full Medicare benefits under age 65 if:
- You have been entitled to Social Security disability benefits for at least 24 months (that need not be consecutive); or
- You receive a disability pension from the Railroad Retirement Board and meet certain conditions; or
- You have Lou Gehrig’s disease, also known as amyotrophic lateral sclerosis (ALS), which qualifies you immediately; or
What makes you eligible for Medicare?
You qualify for full Medicare benefits if:
- You are a U.S. ...
- You are receiving Social Security or railroad retirement benefits or have worked long enough to be eligible for those benefits but are not yet collecting them.
- You or your spouse is a government employee or retiree who has not paid into Social Security but has paid Medicare payroll taxes while working.
What are the eligibility requirements for Medicare?
Medicare Eligibility. You qualify for Medicare if you are 65 or older, a U.S. citizen or a permanent legal resident who’s been in the United States for at least five years, have worked 10 years and paid Medicare taxes. You may also qualify if you are younger than 65 but are disabled or have certain medical conditions.
What is Medicare dual eligible and how do I qualify?
What type of coverage do you get if you are dual eligible for Medicare and Medicaid?
- Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments.
- Specified Low-Income Medicare Beneficiary (SLMB) Program. The SLMB program helps pay for Medicare Part B premiums.
- Qualifying Individual (QI) Program. ...
- Qualified Disabled Working Individual (QDWI) Program. ...

What does Medicare eligible mean?
You are eligible for Medicare if you are a citizen of the United States or have been a legal resident for at least 5 years and: You are age 65 or older and you or your spouse has worked for at least 10 years (or 40 quarters) in Medicare-covered employment.
How do you know if you are Medicare eligible?
You're 65 or older. You are a U.S. citizen or a permanent legal resident who has lived in the United States for at least five years and. You are receiving Social Security or railroad retirement benefits or have worked long enough to be eligible for those benefits but are not yet collecting them.
What is the difference between entitled and eligible for Medicare?
So, for practical purposes, being eligible for Medicare means that a person can enroll because of turning 65 or, if a person is under 65, disabled, and receiving Social Security benefits. Being entitled for Medicare means you have already enrolled.
What would make you ineligible for Medicare?
Did not work in employment covered by Social Security/Medicare. Do not have 40 quarters in Social Security/Medicare-covered employment. Do not qualify through the work history of a current, former, or deceased spouse.
Does everyone get Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Do I automatically get Medicare when I turn 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
What is the difference between entitled and eligible?
But often entitled implies that someone has the right to do something, while eligible means that they satisfy certain requirements in order to do something. The words are not always interchangeable.
Who is eligible for Medicare Part B?
You automatically qualify for Medicare Part B once you turn 65 years old. Although you'll need to wait to use your benefits until your 65th birthday, you can enroll: 3 months before your 65th birthday.
Do you automatically get Medicare with Social Security?
You automatically get Medicare because you're getting benefits from Social Security (or the Railroad Retirement Board). Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
Do I have to pay for Medicare?
Most people don't have to pay a monthly premium for their Medicare Part A coverage. If you've worked for a total of 40 quarters or more during your lifetime, you've already paid for your Medicare Part A coverage through those income taxes.
Do you have to take Part B Medicare?
Medicare Part B isn't a legal requirement, and you don't need it in some situations. In general, if you're eligible for Medicare and have creditable coverage, you can postpone Part B penalty-free. Creditable coverage includes the insurance provided to you or your spouse through work.
Is Medicare Part B free for anyone?
Your income must be no more than the federal poverty level to be eligible for this program, which was an annual income of $12,760 for a single person and an annual income of $17,240 for a married couple in 2020.
What is Medicare Advantage?
Medicare Advantage plans are private insurance health plans that provide all Part A and Part B services. Many also offer prescription drug coverage and other supplemental benefits. Similar to how Medicaid works with Original Medicare, Medicaid wraps around the services provided by the Medicare Advantage plan andserves as a payer of last resort.
When will Medicare become the main health insurance?
July 08, 2020. Most Americans understand that when they turn 65, Medicare will become their main health insurance plan. However, many Americans are less familiar with another health care program, Medicaid, and what it means if they are eligible for both Medicare and Medicaid. If you are dual eligible, Medicaid may pay for your Medicare ...
What is dual eligible?
The term “full dual eligible” refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as “partial dual eligible.”.
What is dual eligible for medicaid?
Qualifications for Medicaid vary by state, but, generally, people who qualify for full dual eligible coverage are recipients of Supplemental Security Income (SSI). The SSI program provides cash assistance to people who are aged, blind, or disabled to help them meet basic food and housing needs.
What is Medicaid managed care?
Medicaid managed care is similar to Medicare Advantage, in that states contract with private insurance health plans to manage and deliver the care. In some states, the Medicaid managed care plan is responsible for coordinating the Medicare and Medicaid services and payments.
What is a PACE plan?
Similar to D-SNPs, PACE plans provide medical and social services to frail and elderly individuals (most of whom are dual eligible). PACE operates through a “health home”-type model, where an interdisciplinary team of health care physicians and other providers work together to provide coordinated care to the patient. PACE plans also focus on helping enrollees receive care in their homes or in the community, with the goal of avoiding placement in nursing homes or other long-term care institutions.
Does Medicare cover Part A and Part B?
Some Medicare beneficiaries may choose to receive their services through the Original Medicare Program. In this case, they receive the Part A and Part B services directly through a plan administered by the federal government, which pays providers on a fee-for-service (FFS) basis. In this case, Medicaid would “wrap around” Medicare coverage by paying for services not covered by Medicare or by covering premium and cost-sharing payments, depending on whether the beneficiary is a full or partial dual eligible.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
What is the standard Part B premium for 2020?
The standard Part B premium amount in 2020 is $144.60. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover all of the costs of health care?
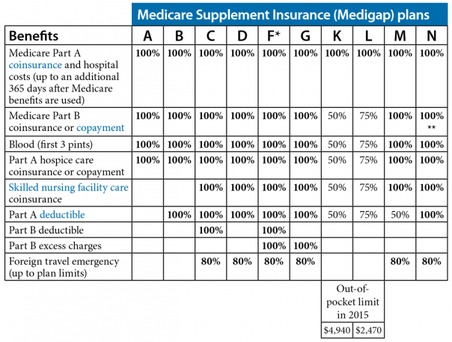
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is Medicare card?
The Medicare card is used to identify the individual as being entitled and also serves as a source of information required to process Medicare claims or bills. It displays the beneficiary's name, Medicare number, and effective date of entitlement to hospital insurance and/or medical insurance. The Social Security Administration's Social Security Office assists in replacing a lost or destroyed Medicare cards.
When does dialysis eligibility start?
Entitlement usually begins after a 3-month waiting period has been served, i.e., with the first day of the third month after the month in which a course of regular dialysis begins. Entitlement begins before the waiting period has expired if the individual receives a transplant or participates in a self-dialysis training program during the waiting period.
How long is the grace period for SMI?
grace period has been provided for payment of premiums by those who are billed directly. The period extends for 90 days after the month in which the bill is mailed. If the premiums are not received in that prescribed time, entitlement terminates at the end of the grace period. This 90-day grace period for paying overdue SMI premiums and continuing SMI coverage may be extended by CMS for good cause for up to an additional 90 days. Good cause, for example, is found if the enrollee was mentally or physically incapable of paying his or her premiums timely, or had some reasonable basis to believe that payment had been made, or the failure to pay was due to administrative error.
How long does premium hospital insurance last?
Persons may enroll for premium hospital insurance by filing a request during the IEP which begins the third month before the month of first eligibility and lasts for 7 months. The individual's IEP for premium hospital insurance is in most cases the same 7-month period as the IEP for SMI.
How do I qualify for premium free HI?
To be eligible for premium-free HI, an individual must be "insured" based on his or her own earnings or those of a spouse, parent, or child. To be insured, the worker must have a specific number of quarters of coverage (QCs); the exact number required is dependent upon whether the person is filing for HI on the basis of age, disability, or end stage renal disease. QCs are earned through payment of payroll taxes under the Federal Insurance Contributions Act (FICA) during the person's working years. QCs earned by an individual who pays the full FICA tax are usable to insure the person for both monthly social security benefits and HI.
What is hospital insurance?
Hospital insurance (HI), as well as supplementary medical insurance (SMI), is available to three basic groups of "insured individuals"- the aged, the disabled, and those with end stage renal disease. Following is an explanation of how an individual becomes "insured" as well as an explanation of the eligibility requirements for each group.
Who is eligible for HI?
Individuals of any age with end stage renal disease (ESRD) who receive dialysis on a regular basis or a kidney transplant are eligible for HI (and are deemed enrolled for Supplementary Medical Insurance (SMI) unless such coverage is refused) if they file an application. They must also meet certain work requirements for insured status under the social security or railroad retirement programs, or be entitled to monthly social security benefits or an annuity under the Railroad Retirement Act, or be the spouse or dependent child of an insured or entitled person.
What is a benefit period?
benefit period is a period of time for measuring the use of hospital insurance benefits. It is a period of consecutive days during which covered services furnished to a patient, up to certain specified maximum amounts, may be paid for by the hospital insurance plan. For example, a patient is eligible for 90 days of hospital care in a benefit period and 100 days of extended care services during the same benefit period. A patient may be eligible for as many as l50 days of hospital care in a benefit period if he/she draws on his/her lifetime reserve. As long as a person continues to be entitled to hospital insurance, there is no limit on the number of benefit periods he/she may have. The term "benefit period" is synonymous with spell of illness. Since the term "spell of illness" could connote a single illness or a particular "spell" of sickness, the term benefit period is used in communications with the public.
Is whole blood deductible for Part A?
Program payment may not be made for the first 3 pints of whole blood or equivalent units of packed red cells received under Part A and Part B combined in a calendar year. However, blood processing (e.g., administration, storage) is not subject to the deductible.
What is Medi-Cal for Medicare?
Medi-Cal (for People with Medicare) Medi-Cal, the Medicaid program in California, provides health coverage to people with low-income and asset levels who meet certain eligibility requirements. While there are several ways to qualify for Medi-Cal, this section focuses only on Medi-Cal beneficiaries who also qualify for Medicare — individuals who are ...
How much does a person need to be to qualify for Medi-Cal?
To qualify for SSI, you must be age 65 or older, blind or disabled. Your countable monthly income may not exceed $954.72 for an individual or $1,598.14 for a couple (higher income levels apply for individuals who are blind).
What is Medicare Part D?
2. Prescription Drugs. If you are receiving both Medicare and Medi-Cal benefits, the Medicare Part D drug benefit will provide your prescription-drug coverage instead of Medi-Cal. You must be enrolled in a Medicare Part D drug plan or a Medicare Advantage prescription drug plan to get these benefits.
How much does Medi-Cal pay for SOC?
For example, if you have an individual monthly income of $1,300, Medi-Cal subtracts $600 for a SOC of $700 . This means you must pay at least $700 in covered medical expenses and/or health care premiums in a given month before Medi-Cal covers any of your health care costs for that month.
How much does Medi-Cal pay for medical expenses?
Your SOC is determined according to your monthly income, using the following formula: Medi-Cal subtracts $600 (for an individual) or $934 (for a couple) from your monthly income, and any other health-insurance premiums you may be paying.
Which MA plan works best for people with Medicare and Medi-Cal?
If you choose an MA plan, the MA plan that works best for people with both Medicare and Medi-Cal is the Special Needs Plan (SNP) for dual eligibles or D-SNP. If you’re enrolled in a D-SNP, you do not have copays, coinsurance or premiums associated with other types of MA plans.
How long does it take to get Medi-Cal?
Processing your application can take several weeks because Medi-Cal must first determine eligibility by verifying your income and personal assets before coverage can be approved. You may request Medi-Cal to pay retroactively for the three months prior to the month in which you apply. back to top.