An ultrasonic osteogenesis stimulator (E0760) is covered only if all of the following criteria are met: Nonunion of a fracture documented by a minimum of two sets of radiographs obtained prior to starting treatment with the osteogenesis stimulator, separated by a minimum of 90 days.
Full Answer
What are the requirements for an ultrasonic osteogenesis stimulator (e0760)?
An ultrasonic osteogenesis stimulator (E0760) is covered only if all of the following criteria are met: Nonunion of a fracture documented by a minimum of two sets of radiographs obtained prior to starting treatment with the osteogenesis stimulator, separated by a minimum of 90 days.
What is the KF modifier for e0747 and e0748?
Devices coded E0747, E0748 and E0760 are classified by the Food and Drug Administration as Class III devices; therefore, all claims for codes E0747, E0748 and E0760 must include the KF modifier. Claim lines billed without a KF modifier will be rejected as missing information.
Can a provider use CPT code 99070 without a fee?
For example, none of the “J” codes have been adopted. If an HCPCS code is billed, and the code does not have a fee assigned in the Commission schedule, the Commission will allow a provider to use CPT code 99070. The provider is entitled to 20% above invoice cost for these codes only.
Does Medicare cover ultrasonic osteogenesis stimulators?
Medicare allows ultrasonic osteogenesis stimulators only if all of the following criteria are met: nonunion of a fracture documented by a minimum of two sets of radiographs obtained prior to starting treatment with the osteogenic stimulator, separated by a minimum of 90 days; and the fracture is not of the skull or vertebrae; and
What is E0747?
What are the requirements for Medicare?
What is CMS in healthcare?
Can you use CPT in Medicare?
What is Section 1833 E?
Is a non-spinal osteogenesis stimulator medically necessary?
Where is the LCD standard documentation requirement?
See more
About this website

Are bone stimulators covered by Medicare?
The U.S. Centers for Medicare and Medicaid Services has expanded Medicare coverage for the Exogen bone healing system, according to a press release from Smith & Nephew, makers of the device. Since 2000, Medicare has reimbursed the use of the Exogen system only for nonunion cases following surgical repair.
How much does a bone stimulator cost?
Cost of Bone Stimulators An implanted electrical stimulator may cost up to $5,000.
Does United Healthcare cover bone stimulator?
Ultrasonic osteogenic stimulators are covered as medically reasonable and necessary for the treatment of nonunion fractures. In demonstrating non-union fractures, CMS expects: A minimum of 2 sets of radiographs, obtained prior to starting treatment with the osteogenic stimulator, separated by a minimum of 90 days.
What is Osteogenesis stimulator electrical non-invasive spinal applications?
An ultrasonic osteogenic stimulator is a noninvasive device that emits low intensity, pulsed ultrasound. The device is applied to the surface of the skin at the fracture site and ultrasound waves are emitted via a conductive coupling gel to stimulate fracture healing.
What is the success rate on a bone stimulator?
The reported overall success rate for the 1,382 patients was 89.6%. The results were analyzed in audited subsets comparing days of treatment time and average daily use of the electrical bone growth stimulator, using several statistical methods.
Is a bone growth stimulator covered by insurance?
Invasive bone growth stimulators are considered internal medical devices and, therefore, are covered under the core medical benefits of many plans. Refer to the customer's benefit plan document for coverage details.
How Much Does Medicare pay for bone stimulator?
For individuals receiving Medicare benefits, the cost you will have to cover is generally 20% of the Medicare allowable amount. However, this technology is expensive, and the price of a bone growth stimulation unit can range from $500 to $5,000. This means that your out of pocket copay may be as high as $1,000.
How many times a day can you use a bone stimulator?
A: Your doctor will prescribe a daily treatment time based on your needs. The SpinalStim device is typically worn a minimum of two hours a day. The CervicalStim device is worn four hours a day.
How long does a bone growth stimulator last?
Typically, the external bone growth stimulator will be worn for a period of 3 to 9 months following the surgery.
How much does a Djo bone growth stimulator cost?
Although they cost $50 to $100 to make, the stimulators retail for $5,000 and Medicare reimburses for $4,000, according to the suit.
Is a TENS unit the same as a bone growth stimulator?
While TENS units are good for treating pain, a bone growth stimulator is more effective for healing broken bones and also can provide pain relief. Bone growth stimulators heal fractures with either electrical or ultrasound energy.
Is a bone growth stimulator necessary?
Bone stimulators are currently not necessary for routine fracture healing. There is no evidence to support their use in a typical fracture as they have not been shown to improve the outcome for patients.
CPT 20974, 20975, E0747 – Electrical Bone Growth stimulator
Code Description CPT. 20974 Electrical stimulation to aid bone healing; noninvasive (non-operative). 20975 Electrical stimulation to aid bone healing; invasive (operative). HCPCS. E0747 Osteogenesis stimulator, electrical, noninvasive, other than spinal applications. E0749 Osteogenesis stimulator, electrical, surgically implanted. Electrical Bone Growth Stimulation of the Appendicular Skeleton
Osteogenesis Stimulator - Spinal and Nonspinal
DMEPOS (Medicare/Commercial/NH Medicaid) Page 3 of 6 Confidential and Proprietary Osteogenesis Stimulators – Spinal and Non Spinal An ultrasonic osteogenesis stimulator will be denied as not reasonable and
Billing Instructions - LSO and TLSO - JD DME - Noridian
The DME MACs have claims data showing that spinal orthoses are often replaced at a frequency greater than the allowed 5-year reasonable useful lifetime (RUL).
E0748 - HCPCS Code for Elec osteogen stim spinal
Durable Medical Equipment (DME) E0748 is a valid 2022 HCPCS code for Osteogenesis stimulator, electrical, non-invasive, spinal applications or just “Elec osteogen stim spinal” for short, used in Used durable medical equipment (DME).
Electrotherapy - Coding & Billing Guide
Unit Types: TENS units ‐‐ TENS is effectively used to treat all types of chronic and acute pain. Just about anything for which you would take an aspirin, Tylenol, or any other pain medication can probably be effectively relieved with a TENS unit.
KF Modifier Use - Correct Coding - CGS Medicare
August 29, 2019. KF Modifier Use - Correct Coding. Joint DME MAC Publication. Suppliers are reminded that devices classified by the Food & Drug Administration (FDA) as Class III devices must be billed using the KF modifier (ITEM DESIGNATED BY FDA AS CLASS III DEVICE).
What is a modifier in HCPCS level 2?
In HCPCS Level II, modifiers are composed of two alpha or alphanumeric characters.
What is the code for Osteogenesis?
E0760 is a valid 2021 HCPCS code for Osteogenesis stimulator, low intensity ultrasound, non-invasive or just “ Osteogen ultrasound stimltor ” for short, used in Used durable medical equipment (DME) .
What is CMS type?
The carrier assigned CMS type of service which describes the particular kind (s) of service represented by the procedure code.
How many pricing codes are there in a procedure?
Code used to identify the appropriate methodology for developing unique pricing amounts under part B. A procedure may have one to four pricing codes.
What is Medicare approved amount?
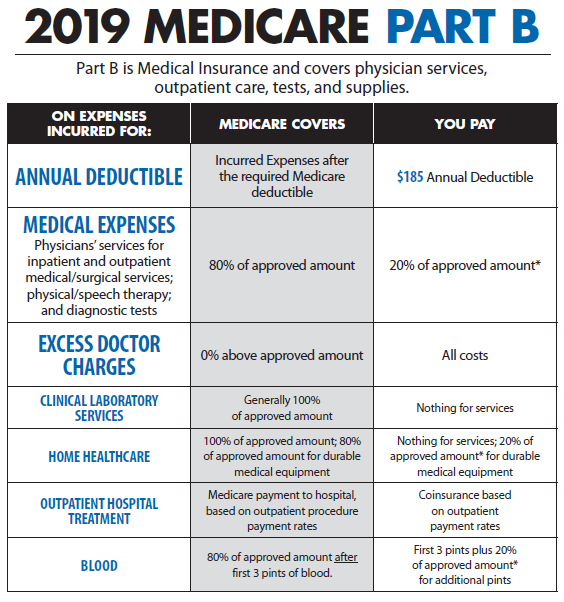
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. you pay 20% of the. Medicare-Approved Amount.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
What is the CPT code for HCPCS?
If an HCPCS code is billed, and the code does not have a fee assigned in the Commission schedule, the Commission will allow a provider to use CPT code 99070. The provider is entitled to 20% above invoice cost for these codes only.
How many HCPCS codes are there in North Carolina?
The North Carolina Industrial Commission has adopted nearly 1,100 HCPCS billing codes to describe supplies and equipment used in workers’ compensation treatment. However, the Commission has not yet incorporated into its fee schedule all of the HCPCS level codes for supplies and equipments.
What is CPB 0175?
See also CPB 0175 - High-Frequency Pulsed Electromagnetic Stimulation.
When was electrical stimulation approved?
In 1979 , the FDA approved electrical stimulation therapy devices for treatment of nonunion, congenital pseudarthrosis, and failed fusion. A number of prospective studies, including controlled clinical trials, have demonstrated the effectiveness of electrical stimulation in nonunions of long bones.
What is an osteogenesis stimulator?
An electrical osteogenesis stimulator is a device that provides electrical stimulation to augment bone repair. Electrical stimulation can be applied either from the outside of the body (noninvasive) or from the inside of the body (invasive). A noninvasive electrical stimulator is characterized by an external power source which is attached to a coil or electrodes placed on the skin or on a cast or brace over a fracture or fusion site.
Is Aetna an experimental stimulator?
Aetna considers an ultrasonic osteogenesis stimulator experimental and investigational for all other indications, including the following (not an all-inclusive list) because the medical literature does not support its use for these indications:
Is an ultrasonic osteogenesis stimulator necessary for nonunions?
Aetna considers an ultrasonic osteogenesis stimulator medically necessary for non-unions, failed arthrodesis, and congenital pseudarthrosis (pseudoarthrosis) of the appendicular skeleton if there has been no X-ray evidence of progression of healing for 3 or more months despite appropriate fracture care, and the following criteria are met:
What is E0747?
A non-spinal electrical osteogenesis stimulator (E0747) is covered only if any of the following criteria are met:
What are the requirements for Medicare?
For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Local Coverage Determinations (LCDs). CMS believes that the Internet is an effective method to share LCDs that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
What is Section 1833 E?
Section 1833 (e) of the Social Security Act precludes payment to any provider of services unless " there has been furnished such information as may be necessary in order to determine the amounts due such provider.” It is expected that the beneficiary's medical records will reflect the need for the care provided. The beneficiary's medical records include the treating practitioner's office records, hospital records, nursing home records, home health agency records, records from other healthcare professionals and test reports. This documentation must be available upon request.
Is a non-spinal osteogenesis stimulator medically necessary?
A non-spinal electrical osteogenesis stimulator will be denied as not medically necessary if none of the criteria above are met.
Where is the LCD standard documentation requirement?
The LCD-related Standard Documentation Requirements Article, located at the bottom of this policy under the Related Local Coverage Documents section.