Full Answer
What is the difference between Medicare an and B?
Medicare parts A and B cover different types of health services. Generally, Part A covers inpatient treatments, and Part B covers visits to doctors, some medical supplies, and some devices.
Does Medicare B cover drugs?
Medicare Part B may cover drugs that are given in a doctor’s office and aren’t typically self-administered. Examples include vaccines and chemotherapy. Routine vision care: Original Medicare won’t cover most routine vision services and supplies, including eye exams, eyeglasses, contacts, and exams to get fitted for contacts and glasses.
What is the maximum premium for Medicare Part B?
The standard monthly premium for Part B, which covers outpatient care and durable equipment ... or offers a different copay and an out-of-pocket maximum (a Medicare Advantage Plan). The Aduhelm situation highlights the ripple effect that expensive drugs ...
What are the advantages of Medicare Part B?
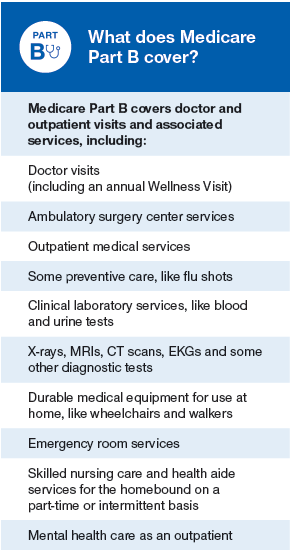
What does Medicare Part B cover?
- Doctor visits
- Certain cancer screenings
- Certain lab tests
- An annual wellness visit with your primary care provider
- A one-time Welcome to Medicare visit with your primary care provider
- Diabetes screening, supplies, and certain services
- A diabetes prevention program for those who qualify
- Alcohol abuse screening and counseling for those who qualify
- Flu shots

What main things are covered under Medicare Part B?
Part B covers things like:Clinical research.Ambulance services.Durable medical equipment (DME)Mental health. Inpatient. Outpatient. Partial hospitalization.Limited outpatient prescription drugs.
What does Medicare Plan B offer?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services.
Does Medicare Part B cover 100 percent?
Generally speaking, Medicare reimbursement under Part B is 80% of allowable charges for a covered service after you meet your Part B deductible. Unlike Part A, you pay your Part B deductible just once each calendar year. After that, you generally pay 20% of the Medicare-approved amount for your care.
Does Medicare Part B cover doctor visits?
Medicare Part B pays for outpatient medical care, such as doctor visits, some home health services, some laboratory tests, some medications, and some medical equipment. (Hospital and skilled nursing facility stays are covered under Medicare Part A, as are some home health services.)
Does Medicare Part B pay for prescriptions?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers a limited number of outpatient prescription drugs under certain conditions. A part of a hospital where you get outpatient services, like an emergency department, observation unit, surgery center, or pain clinic.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Which service is not covered by Part B Medicare?
But there are still some services that Part B does not pay for. If you're enrolled in the original Medicare program, these gaps in coverage include: Routine services for vision, hearing and dental care — for example, checkups, eyeglasses, hearing aids, dental extractions and dentures.
Who pays the 20% of a Medicare B claim?
After the beneficiary meets the annual deductible, Part B will pay 80% of the “reasonable charge” for covered services, the reimbursement rate determined by Medicare; the beneficiary is responsible for the remaining 20% as “co-insurance.” Unfortunately, the “reasonable charge” is often less than the provider's actual ...
Is there a max out of pocket for Medicare Part B?
Medicare Part B out-of-pocket costs You will also pay an annual deductible in addition to the monthly premiums, and you must pay a portion of any costs after you meet the deductible. There is no out-of-pocket maximum when it comes to how much you may pay for services you receive through Part B.
Does Medicare cover eye exams?
Eye exams (routine) Medicare doesn't cover eye exams (sometimes called “eye refractions”) for eyeglasses or contact lenses. You pay 100% for eye exams for eyeglasses or contact lenses.
What surgeries are covered by Medicare?
Medicare covers most medically necessary surgeries, and you can find a list of these on the Medicare Benefits Schedule (MBS). Since surgeries happen mainly in hospitals, Medicare will cover 100% of all costs related to the surgery if you have it done in a public hospital.
Do you have copays with Medicare?
What Is a Medicare Copayment? There are generally no copayments with Original Medicare — Medicare Part A and Part B — but you may have coinsurance costs. You may have a copayment if you have a Medicare Advantage plan or Medicare Part D prescription drug plan.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is Medicare Advantage?
Medicare Advantage (Part C) plans are offered by private insurance companies who contract with Medicare to provide your Part A and Part B benefits.
Is Medicare Part B deductible?
Most people are automatically enrolled in premium-free Part A (Hospital Insurance) if they paid taxes for a certain period of time. Many Medicare recipients choose to enroll in Part B (Medical Insurance) when they are first eligible. There is a monthly premium and an annual deductible for Part B coverage. Medicare Part B (Medical Insurance) is ...
What is Medicare Part B?
It consists of several parts, one of which is Part B. Medicare Part B is the part of Medicare that provides medical insurance. You can use it to cover various outpatient services.
What is part B in medical?
occupational therapy. other testing, such as imaging tests and echocardiograms. outpatient hospital and mental health care. physical therapy. transplants. Part B also covers somepreventative services as well.
What is a Part B?
Part B covers a wide variety of medically necessary outpatient services. A service is determined medically necessary if it’s needed to effectively diagnose or treat a health condition. Some examples of servicescovered by Part B are: emergency ambulance transportation. chemotherapy.
What is the monthly premium for Part B insurance in 2021?
Your monthly premium is what you pay each month for Part B coverage. For 2021, the standard Part B monthly premium is $148.50. People with higher yearly incomes may have to pay higher monthly premiums. Your yearly income is determined based off of your tax return from two years ago.
What happens if you don't enroll in Part B?
When you need to pay the late enrollment penalty, your monthly premium can increase up to 10 percent of the standard premium for each 12-month period that you were eligible for Part B but didn’t enroll.
Who is covered by Part A and Part B?
All people with Part A and/or Part B who meet all of these conditions are covered: You must be under the care of a doctor , and you must be getting services under a plan of care created and reviewed regularly by a doctor.
What is an ABN for home health?
The home health agency should give you a notice called the Advance Beneficiary Notice" (ABN) before giving you services and supplies that Medicare doesn't cover. Note. If you get services from a home health agency in Florida, Illinois, Massachusetts, Michigan, or Texas, you may be affected by a Medicare demonstration program. ...
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).