What is the difference between Medicare an and B?
(DME MACs), termed “Satellites,” and located in a defined geographic area (sector). Each MAC within the sector is linked to its Host via telecommunications through their respective CMS Virtual Data Center (VDC). The Medicare Part A, B or DME processing system creates a nightly CWF file out of the MACs processing region, containing claims data.
What does the B in Medicare number mean?
Medicare Part B billing codes are available to report BHI services furnished to beneficiaries during a calendar month service period. As of January 1, 2017, Medicare makes separate payments to physicians and non-physician practitioners for BHI services they furnish to beneficiaries over a calendar month service period.
How do I apply for Medicare B?
Medicare Part A is hospital coverage that covers certain costs incurred during an inpatient hospital admission. This includes things such as your room fees, meals, operating room, and rehabilitation services, together with lab tests and X-rays. Medicare Part A also covers necessary medical supplies and drugs that are given during your hospital ...
Should I get Medicare B?
· Best Answer. Copy. Medicare beneficiaries. Wiki User. ∙ 2011-04-26 19:23:16. This answer is: Helpful ( 0) Not Helpful ( 0) Add a Comment.

Which of the following expenses would be paid by Medicare Part B?
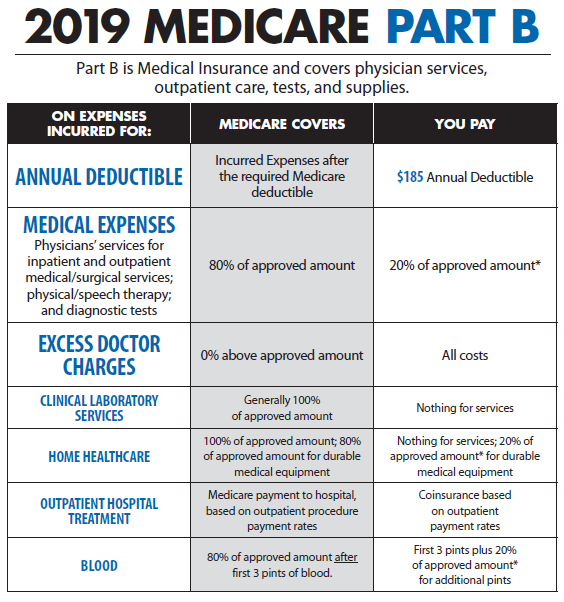
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services.
What is the Medicare Secondary Payer debt?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare.
How do I bill Medicare for physical therapy?
You must complete at least eight minutes of treatment be paid for one 15-minutes increment. So, for example, if you completed 17 minutes of treatment, Medicare would be billed for 15 minutes, or one unit. However, if you completed 23 minutes of treatment, Medicare would be billed for two units of treatment.
What is a Medicare demand letter?
When the most recent search is completed and related claims are identified, the recovery contractor will issue a demand letter advising the debtor of the amount of money owed to the Medicare program and how to resolve the debt by repayment. The demand letter also includes information on administrative appeal rights.
Is it better to have Medicare as primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Does Medicare automatically send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.
What is the 8 minute rule in physical therapy?
A therapist must provide direct one-to-one therapy for at least 8 minutes to receive reimbursement for a time based treatment code. When only one service is provided in a day, you shouldn't bill for services performed for less than 8 minutes.
What is the Medicare cap for physical therapy for 2021?
For 2021 this KX modifier threshold amount is: $2,110 for PT and SLP services combined, and. $2,110 for OT services.
What will the Medicare premium be in 2021?
The Centers for Medicare & Medicaid Services (CMS) has announced that the standard monthly Part B premium will be $148.50 in 2021, an increase of $3.90 from $144.60 in 2020.
Do you have to repay Medicare?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
How long does Medicare have to recoup payments?
(1) Medicare contractors can begin recoupment no earlier than 41 days from the date of the initial overpayment demand but shall cease recoupment of the overpayment in question, upon receipt of a timely and valid request for a redetermination of an overpayment.
Are Medicare liens negotiable?
The Nature of the Medicare Medical Lien This means that if you get a settlement, you will have to pay back Medicare before anything else gets taken out. While you can get the lien reduced, paying back Medicare after a settlement is not optional. The only path around a Medicare lien is to negotiate the lien to zero.
What is a referral for BHI?
The BHI services require that there must be a presenting psychiatric or behavioral health condition that, in the clinical judgment of the treating physician or other qualified health professional, warrants “referral” to the behavioral health care manager for further assessment and treatment through provision of psychiatric CoCM services or General
What is a BHI code?
The BHI codes allow for remote provision of certain services by the psychiatric consultant and other members of the care team. For CoCM, the behavioral health care manager must be available to provide face-to-face services in person, but provision of face-to-face services is not required. The BHI codes do not describe services that are subject to the rules for Medicare telehealth services in the narrow meaning of the term (under section 1834(m) of the Social Security Act).
What is a behavioral health care manager?
As noted in the CY 2017 PFS final rule, (81 FR 80231), the behavioral health care manager is a designated member of the care team with formal education or specialized training in behavioral health (which would include a range of disciplines, for example, social work, nursing, and psychology), but Medicare did not specify a minimum education requirement. They may or may not be a professional who meets all the requirements to independently furnish and report services to Medicare. The behavioral health care manager must be available to provide services face-to-face with the beneficiary, have a continuous relationship with the beneficiary, and have a collaborative, integrated relationship with the rest of the care team. He or she must also be able to engage the beneficiary outside of regular clinic hours as needed.
What is the difference between BHI and CCM?
There are substantial differences in the potential number and nature of conditions, types of individuals providing the services, and time spent providing services. CCM involves care planning for all health issues and includes systems to ensure receipt of all recommended preventive services, whereas BHI care planning focuses on individuals with behavioral health issues, systematic care management using validated rating scales (when applicable), and does not focus on preventive services. CCM requires use of certified electronic health information technology, whereas BHI does not. In most cases, we believe it would not be difficult to determine which set of codes (BHI or CCM) more accurately describe the patient and the services provided. As we state in the final rule, the code(s) that most specifically describe the services being furnished should be used. If a BHI service code more specifically describes the service furnished (service time and other relevant aspects of the service being equal), then it is more appropriate to report the BHI code(s) than the CCM code(s).
Can BHI be used in both facility and non-facility settings?
Yes, the BHI codes are priced in both facility and non-facility settings. The POS on the claim should be the location where the billing practitioner would ordinarily provide face-to-face care to the beneficiary.
Can BHI codes be used for substance use disorders?
No, as provided in the CY 2017 PFS Final Rule (81 FR 80232), the BHI codes may be used to treat patients with any mental, behavioral health or psychiatric condition that is being treated by the billing practitioner, including substance use disorders. We did not limit billing and payment for the BHI codes to a specified set of behavioral health conditions. The services require that there must be a presenting mental, psychiatric or behavioral health condition(s) that, in the clinical judgment of the billing practitioner, warrants BHI services. The diagnosis or diagnoses could be either pre-existing or made by the billing practitioner and may be refined over time.
Can a behavioral health care manager report to Medicare?
Yes. As noted in the CY 2017 PFS Final Rule, (81 FR 80231-80232) if the behavioral health care manager is eligible to independently furnish and report services to Medicare, then that individual could report separate services furnished to a beneficiary receiving BHI services in the same calendar month such as psychiatric evaluation, psychotherapy, and alcohol or substance abuse intervention services. Time spent by the behavioral health care manager on activities for services reported separately could not be included in the time applied to any BHI service code (in other words, time and effort cannot be counted more than once).
What is Medicare Part A and B?
1.Both Medicare Part A and B are federally funded plans that come with different coverages. #N#2.Part A is free, and the patients need not pay a premium for the coverage. People have to pay some premium for availing themselves of the Part B coverage.#N#3.Part A can be called hospital insurance whereas Part B can be termed as medical insurance.#N#4.Part A covers inpatient care, nursing facilities, hospital facilities, and critical access to hospitals. Part A also covers home health and hospice. Part B insurance will compensate for all medically necessary supplies and services. It also covers outpatient care, physical/occupational therapists, doctor’s services, and home health care.#N#5.For getting Medicare coverage, one should be 65 years old and must have paid to Social Security or to the Railroad 6.Retirement Fund when they were employed. But for Part B, there is no need for any Social Security credits.
What is Part B insurance?
Part B insurance will compensate for the all medically necessary supplies and services. People have to pay some premium for availing themselves of the Part B coverage. Part B insurance covers outpatient care, physical/occupational therapists, doctor’s services, and home health care.
What are the different types of Medicare?
The Medicare policy is divided into two types: Original Medicare Plan and Medicare Advantage Plan. Each of these consists of four subdivisions: Part A, B, C, and D. Both Medicare Part A and B are federally funded plans that comes with different coverage. Part A can be called hospital insurance whereas Part B can be termed as medical insurance.
What is the difference between Part A and Part B?
Part A can be called hospital insurance where as Part B can be termed as medical insurance. Part A is free, and the patients need not pay a premium for the coverage. This facility covers inpatient care, nursing facilities, hospital facilities, and critical access to hospitals. Part A also covers home health and hospice.
How old do you have to be to get Medicare?
It also covers outpatient care, physical/occupational therapists, doctor’s services, and home health care. 5.For getting Medicare coverage, one should be 65 years old and must have paid to Social Security or to the Railroad 6.Retirement Fund when they were employed.
What does Part A cover?
4.Part A covers inpatient care, nursing facilities, hospital facilities, and critical access to hospitals. Part A also covers home health and hospice. Part B insurance will compensate for all medically necessary supplies and services. It also covers outpatient care, physical/occupational therapists, doctor’s services, and home health care.
Is OIVIT covered by Medicare?
Therefore, services OIVIT and services comprising and OIVIT regimen are nationally non-covered by Medicare.
Is OIVIT a reasonable indication for Social Security?
Therefore, CMS determines that OIVIT is not reasonable and necessary for any indication under section 1862(a)(1)(A) of the Social Security Act. Services comprising an Outpatient Intravenous Insulin Therapy regimen are nationally non-covered under Medicare when furnished pursuant to an OIVIT regimen (see subsection A. above).
How much is the penalty for Medicare Part B?
Later on if you wish to add Medicare Part B, you may be subject to a penalty of 10% per year for every year that you waited to enroll.
Does Boomer Benefits cover Medicare?
Boomer Benefits provides free claims support for life for all of our Medigap and Medicare Advantage policyholders so that you are never alone in dealing with Medicare.
