Full Answer
What is the proper format for a progress note for Medicare?
There is no particular format required by Medicare as long as all the above is contained in the note as long as it happens at least once every 10 treatment visits. When co-treating a patient with a PTA or OTA the PT or OT must personally provide one full billable service on one date of service (DOS) within that progress note period.
What is a Medicare Progress Report and why is it important?
Let’s start with the reasoning behind this documents. From Medicare’s perspective, the primary purpose of all Part B documentation is to demonstrate that the care fully supports the medical necessity of the services provided. That means a Progress Report must clearly describe how the services are medically necessary for that patient.
Is a progress report considered a treatment note?
Like all documentation, Medicare considers it included in the payment for the treatment time charge. Progress Reports do not need to be a separate document from a daily treatment note. As long as the treatment note contains all the elements (listed below) of a Progress Report, Medicare will consider you to be in compliance with their requirements.
What do the dates on a Medicare notice mean?
Under the Medicare number is the print date of the notice. And under that is the dates of service this notice covers. Please pay attention to that date range. It is possible you are looking at claims from provider visits that are further back in the past than you may be expecting. Under the gray box is your deductible status.
What information is included in the progress notes?
Progress notes can and should be relatively brief, focusing on developments since the previous note, and recapitulating only relevant, ongoing, active problems. Cutting and pasting from previous notes without editing or updating is not permitted, and outdated and redundant information should be eliminated from notes.
What does progress notes mean in medical terms?
Progress Note. Description. Represents a patient's interval status during a hospitalization, outpatient visit, treatment with a post-acute care provider, or other healthcare encounter.
Does Medicare require progress note every 30 days?
Progress Reports Medicare requires a Progress Report be completed at least every 10 treatment days. The next reporting period begins on the next treatment day after the Progress Report was performed.
What factors are included in a patient progress note?
The majority of the medical record consists of progress notes documenting the care delivered and the clinical events relevant to diagnosis and treatment for a patient. They should be readable, easily understood, complete, accurate, and concise.
What is the most common form of Progress Note charting?
SOAP notes. Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records.
What should be included in nursing progress notes?
Elements to include in a nursing progress noteDate and time of the report.Patient's name.Doctor and nurse's name.General description of the patient.Reason for the visit.Vital signs and initial health assessment.Results of any tests or bloodwork.Diagnosis and care plan.More items...•
What are the Medicare requirements for documenting levels of assistance?
Requirements: Documentation must show objective loss of joint motion (degrees of motion), strength (strength grades), or mobility (levels of assistance) Documentation must show how these therapeutic exercises are helping the patient progress towards their stated, objective and measurable goals.
How often should progress notes be written?
once every 10 treatment visitsProgress Reports need to be written by a PT/OT at least once every 10 treatment visits.
Do progress notes need to be signed?
While CMS does not require an order for a clinical diagnostic test, the physician must document the intent for each test performed and specify the type of test. The progress notes must contain a handwritten or electronic signature.
How do you document progress notes?
What progress notes should includeAll treatment provided to the patient in chronological order, along with length of session.Precise assessments of the patient's response to the treatment (progress and/or lack of progress), and needs.Significant events, emergencies and action taken.More items...•
How do you make a Progress Note medical?
What makes a great progress note? Here are three tips:Tip #1: Write a story. When an individual comes to a health professional with a problem, they will begin to describe their experience. ... Tip #2: Remember that a diagnosis is a label. ... Tip #3: Write a specific plan. ... Alright, as a quick recap...
What are the four parts of a SOAP note?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan. Each heading is described below. This is the first heading of the SOAP note....ObjectiveVital signs.Physical exam findings.Laboratory data.Imaging results.Other diagnostic data.Recognition and review of the documentation of other clinicians.
What is a progress note?
Progress notes supporting medical necessity of diagnostic services. If "testing facility" is billing for the diagnostic services, it is their responsibility to get these notes from the treating physician. A "testing facility" is a Medicare provider or supplier that furnishes diagnostic tests.
What documentation supports rendering/billing provider indicated on claim?
Documentation that supports rendering/billing provider indicated on claim is healthcare professional providing service . Medicare must identify rendering provider of a service not only for use in standard claims transactions but also for review, fraud detection, and planning policies.
What happens if you have illegible records?
Incomplete or illegible records can result in denial of payment for services billed to Medicare. In order for a claim for Medicare benefits to be valid, there must be sufficient documentation in the provider's or hospital's records to verify the services performed were "reasonable and necessary" and required the level of care billed.
What is a telephone call?
A telephone call by treating physician/practitioner or his/her office to testing facility (If the order is communicated via telephone, both the treating physician/practitioner or his/her office, and the testing facility must document the telephone call in their respective copies of the beneficiary's medical records.
Can Medicare overpayment be recovered?
Additionally, if there is insufficient documentation on the claims that have already been adjudicated by Medicare, reimbursement may be considered an overpayment and the funds can be partially or fully recovered. Medical records should be complete, legible, and include the following information.
What is a plan of care for Medicare?
When treating Medicare patients, the Plan of Care refers to the written treatment plan for which the intended therapy services must specifically relate to. The Plan of Care is established at the time of the first visit with the patient and is derived from the clinical information gathered during the Initial Therapy Evaluation.
Can Medicare deny POCs?
Since Medicare could potentially deny or claw back payment if the above time frames are not met, it is essential that your practice establish a workflow to keep track of Medicare POCs and Progress Reports. If your EMR does not offer a tracking system, then this may end up being a manual process using home grown spreadsheets or some other recording method. However, if you are an OptimisPT user, you can take advantage of the embedded alerts, reminders and reports that can track this for you.
How long after a service is rendered can a provider recall?
It is not reasonable to expect that a provider would recall the specifics of a service more than 48 hours after the service was rendered. To properly execute a medical record addendum the PROVIDER must, at a minimum write the following details in the medical record: - the date the record is being amended.
Can you submit a diagnosis that was not originally captured?
For risk coding, you are allowed to submit diagnoses that were not originally captured, as long as they are documented in the patient record and addressed at some point during the attestation period, even if the plan was to do nothing, aka "monitor," or another provider is treating the condition.
Is an addendum a routine part of medical records?
Medical record addendums should be the exception rather than a routine or recurring part of medical record documentation. Failure to properly amend the medical record may give the appearance of falsifying documentation, which is considered fraudulent.
Can a nurse add a note to a physician's note?
A nurse can add a nursing note but they cannot make a change or addendum to a physician note.
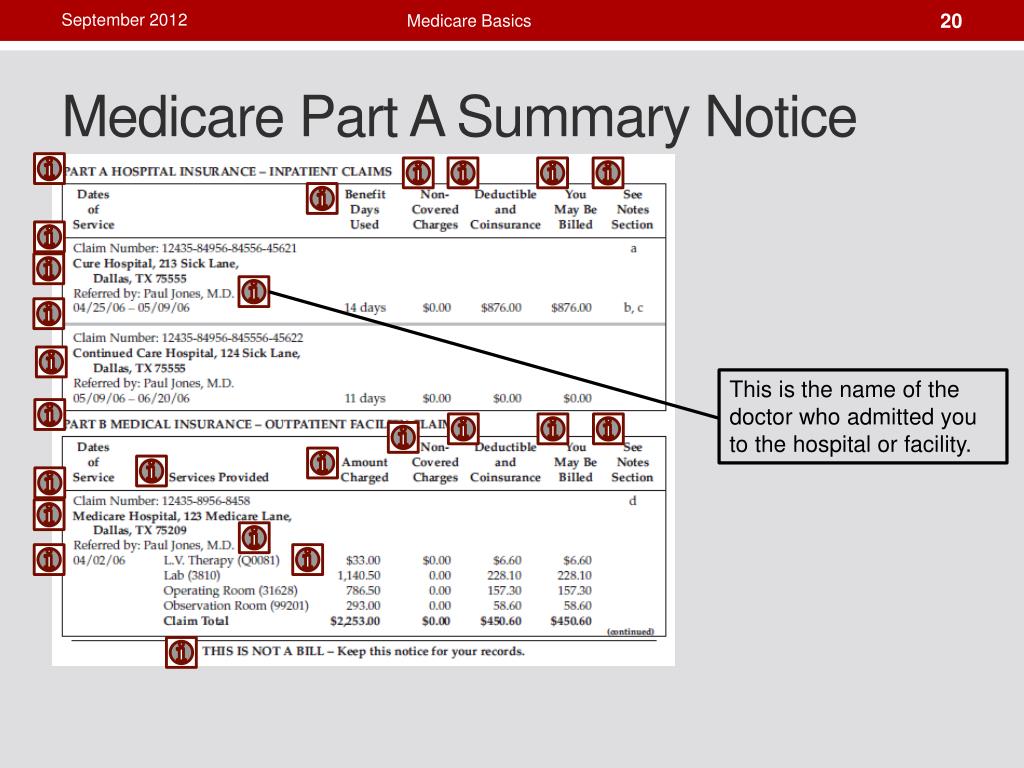
What is the summary notice for Medicare?
This summary is in the right-hand column and lets you know if Medicare denied coverage for any services that quarter and how much you can expect to be billed. Page 3 provides a more detailed summary of each service and its charges.
How often do you get a Medicare summary notice?
The Medicare Summary Notice. If you are on Original Medicare (Part A and Part B), you will receive a Medicare Summary Notice (MSN) quarterly, i.e., every 3 months. You will receive separate MSNs for Part A and Part B coverage.
What is an ABN for Medicare?
The ABN is an acknowledgment that Medicare may not cover the service and that you are willing to pay out of pocket for the service. If you did sign an ABN, it is not valid if it is illegible, if it is signed after the service was performed, or if it is otherwise incomplete.
What is MSN bill?
An MSN is a detailed statement about services that have been charged to Medicare during that time frame but is not a bill in and of itself. THIS IS NOT A BILL will be printed in bold capitalized letters at the top of the statement.
How much can a non-participating provider charge for a limiting charge?
Non-participating providers can add a limiting charge up to 15% more than what is recommended on the fee schedule. Medicare Approved Amount: This lets you know the dollar amount for any services approved for coverage by Medicare. Medicare does not cover the limiting charge.
What to do if your Medicare records don't match?
Whenever you see something that does not match up with your records, reach out to your doctor or medical office for clarification. There could have been a misunderstanding or a true billing error. In the worst-case scenario, it could be a sign of Medicare fraud and abuse.
Is balance billing against the law?
That is called balance billing and it is against the law. Check to see if you signed an Advanced Beneficiary Notice (ABN) for any services Medicare did not approve. You are not liable to pay for these services unless you signed an Advanced Beneficiary Notice beforehand.
What is the most important part of a Medicare notice?
Let’s talk a bit about the notes column. In our opinion, the footnotes are the most important part of the notice. Medicare is required to give an explanation for every claim that is denied, every charge you may be incurring. Each charge usually has one footnote, sometimes even more than that.
What is the gray box on Medicare Part A?
Under the gray box is your deductible status. Please do not get the deductibles for Medicare Part A and Part B confused. A deductible period for part A can happen multiple times in a year and is significantly higher than the Medicare Part B deductible.
What is a Medicare Part A deductible?
Remember the definition of deductible: this is the amount that someone must pay before Medicare pays its share.
What does "assigned claim" mean?
An assigned claim means a doctor has agreed to accept Medicare’s charges in full and may not bill you the difference. Please be aware this is not the same as the typical 20% amount owed. That may still be charged as it is part of the assignment-agreed upon amount. Under the top section are definitions.
Is Part A an annual period?
This is especially important under the Part A notice, because many people are unaware how Part A’s benefit period works. It is not an annual period. The last section on page two is a message from Medicare. Medicare typically has two or three advisories on each notice for you each time you get one.
Do Medicare Advantage members get notices?
Please note that Medicare Advantage members will NOT receive notices like these. If you have a Medicare Advantage plan and need help understanding your bills, it will be in your best interest to speak with your qualified insurance broker or a member of that company’s customer service team for assistance.
What is the progress period for Medicare?
Since 2013, Medicare defines the progress reporting period as, at a minimum, the tenth (10th) treatment visit or sooner if required. Medicare’s intent is that the therapist consistently reviews the plan of care and goals for appropriateness in an on-going fashion.
What is a significant change in a patient's care plan?
A significant change could be a decline in the patient’s condition since the start of therapy or a significant improvement in the patient’s condition that may now necessitate a significant change in the plan of care. The re-evaluation will be used to determine the new plan of care.
What is the difference between a re-evaluation and an initial evaluation?
The only difference between them is as follows: The initial evaluation is completed to assess a new problem for a patient who is not currently under the care of the therapist. The re-evaluation is completed to assess new problems or new clinical findings, ...
What is a re-evaluation?
A re-evaluation requires the same professional skills as an initial evaluation. Indications for a re-evaluation include new clinical findings, a significant change in the patient’s condition, or failure to respond to the therapeutic interventions outlined in the plan of care. A significant change could be a decline in the patient’s condition ...
When is re-evaluation required?
Re-evaluation is separately payable and is periodically indicated during an episode of care when the professional assessment of a clinician indicates a significant improvement, or decline, or change in the patient's condition or functional status that was not anticipated in the plan of care.
When did functional limitation reporting end?
Historically under Medicare Part B, this also marked the time when functional limitation reporting (G-codes) were to be completed, that is until they are abolished as of January 1st, 2019. And this should be billed as…..whatever treatment was already occurring, NOT AS A RE-EVALUATION!
Is Medicare re-evaluation payable?
Medicare states in the Medicare Benefit Policy Manual - Chapter 15 – Covered Medical and Other Health Services, “Routine weekly assessment of expected progression in accordance with the plan are not payable as re-evaluations.”.
How long is reasonable for Medicare?
Compliance Tips: Medicare has clearly stated that “reasonable” means 24 to 48 hours. Understand that anything beyond 48 hours could be considered unreasonable. Providers should comply with this requirement and complete documentation in a timely manner.
What happens if a medical record is illegible?
Illegible documentation may result in medication errors and incorrect diagnoses being assigned to the patient. The medical record must be legible to an individual who is not familiar with the provider’s handwriting. Notes should be timed and dated appropriately, as well.
What is an addendum to a medical record?
A statement that the entry is an addendum to the medical record (An addendum should not be added to the medical record without identifying it as such.) The medical record should be amended within a reasonable time that would allow the service provider to recall the specific details of the patient encounter.
How long is a delay in a note?
Delayed entries within a reasonable time frame (24 to 48 hours) are acceptable for purposes of clarification, error correction, the addition of information not initially available, and if certain unusual circumstances prevented the generation of the note at the time of service.”.
When is medical documentation cloned?
5. “Documentation is considered cloned when each entry in the medical record for a patient is worded exactly alike or similar to the previous entries. Cloning also occurs when medical documentation is exactly the same from patient to patient.
When should a medical record be amended?
The medical record should be amended within a reasonable time that would allow the service provider to recall the specific details of the patient encounter. Medical record addenda should be an exception, rather than a routine or recurring part of medical record documentation.
Do addenda need to be made to the original medical record?
It’s also important to remember that medical record addenda need to be made to the original medical record, not just to the billing copy. “All entries must be legible to another reader to a degree that a meaningful review may be conducted. All notes should be dated, preferably timed, and signed by the author.”.
When to Use A Progress Report vs. A Plan of Care When Treating Medicare Patients
Plan of Care
- When treating Medicare patients, the Plan of Care refers to the written treatment plan for which the intended therapy services must specifically relate to. The Plan of Care is established at the time of the first visit with the patient and is derived from the clinical information gathered during the Initial Therapy Evaluation. Per Medicare, the minimal information required in the Plan of Car…
Progress Reports
- A Progress Report provides justification for the medical necessity of the skilled therapy being provided to the patient. Per Medicare, a Progress Report should include: 1. Objective evidence to support the need for skilled treatment 1.1. This includes such things as validated functional outcome measures and standardized patient assessment tools. Th...
Staying Compliant with Time Frames
- Since Medicare could potentially deny or claw back payment if the above time frames are not met, it is essential that your practice establish a workflow to keep track of Medicare POCs and Progress Reports. If your EMR does not offer a tracking system, then this may end up being a manual process using home grown spreadsheets or some other recording method. However, if y…