When to use patient discharge status code 03 or 04?
1.4 Definitions of Medicare Code Edits September 2011 1. Invalid diagnosis or procedure code The Medicare Code Editor checks each diagnosis including the admit-ting diagnosis and each procedure against a table of valid ICD-10-CM and ICD-10-PCS codes. If an entered code does not agree with any code on the internal list, it is assumed to be invalid.
What is a Medicare denial code?
Discharged/transferred to skilled nursing facility (SNF) with Medicare certification: 04: Discharged/transferred to a facility that provides custodial or supportive care: 05: Discharged/transferred to a designated cancer center or children's hospital: 06
What is the discharge code for a nursing home?
· The current review reason codes and statements can be found below: List of Review Reason Codes and Statements. Please email [email protected] for suggesting a topic to be considered as our next set of standardized review result codes and statements. Page Last Modified: 12/01/2021 07:02 PM. Help with File Formats and Plug-Ins.
What is a group code for Medicare?
This group code shall be used when the adjustment represent an amount that may be billed to the patient or insured. This group would typically be used for deductible and copay adjustments 1 Deductible Amount 2 Coinsurance Amount 3 Co-payment Amount 4 The procedure code is inconsistent with the modifier used or a required modifier is missing.
What does condition code C5 mean?
Any medical reviewC5 Any medical review will be completed after the claim is paid. UB04 Condition Code. C6 The QIO authorized this admission/procedure but has not reviewed the services provided.
What are the Medicare condition codes?
Condition codesCondition CodeDescriptionD5Cancel to correct Medicare Beneficiary ID number or provider IDD6Cancel only to repay a duplicate or OIG overpaymentD7Change to make Medicare the secondary payerD8Change to make Medicare the primary payer7 more rows•Oct 13, 2021
What is Medicare condition code 04?
Condition code 04 (information only bill) Condition code 69 (teaching hospitals only - code indicates a request for a supplemental payment for Indirect Medical Education/Graduate Medical Education/Nursing and Allied Health)
What are value codes?
When reporting numeric values that do not represent dollars and cents, put whole numbers to the left of the dollar/cents delimiter and tenths to the right of the delimiter. Most common Semi-Private Rate - to provide for recording hospital's most common semi- private rate.
What is condition code C5 on UB?
Post payment review applicableQIO ApprovalCodeDescriptionC3Partial approval.C4Admission denied.C5Post payment review applicable.C6Pre-admission/pre-procedure authorized but3 more rows•Dec 21, 2020
What are the condition codes?
Currently, Condition Codes are designed to allow the collection of information related to the patient, particular services, service venue and billing parameters which impact the processing of an Institutional claim.
What does condition code D2 mean?
D1 - Changes in charges. D2 - Changes in revenue code/HCPC. D3 - Second or subsequent interim PPS bill. D4 - Change in Grouper input (DRG) D5 - Cancel only to correct a patient's Medicare ID number or provider number.
What is a Medicare no pay claim?
The no-pay claim is required for those patients who are no longer receiving a skilled level of care but they continue to reside in a certified bed within the facility. The no-pay claim is reported to Medicare as a "noncovered" claim.
What is condition code C3?
Providers must annotate these claims with condition code C3, which is defined “QIO partial approval” and with occurrence span code M0, which is defined “QIO approved stay dates” and the dates provided by the QIO/QIC.
What is value code D5?
• Value code D5: Result of last Kt/V reading. For in-center hemodialysis patients, this is the last reading. taken during the billing period. For peritoneal dialysis patients (and home hemodialysis patients), this. may be before the current billing period but should be within 4 months of the claim date of service.
What is Medicare Value code 12?
1 VALUE CODES FL 39-41 Enter the value codes “12” to indicate Working Aged insurance, or “43” to indicate Disability insurance and the amount you were paid by the primary insurance.
What is a value code 01?
The value codes to be submitted when billing private room revenue codes according to the UB-04 Specifications Manual are: “01” (semi-private room facility) must be accompanied by the semi-private room rate when facility offers semi-private rooms and the patient's stay is in a private room.
When did CMS standardize reason codes?
In 2015 CMS began to standardize the reason codes and statements for certain services. As a result, providers experience more continuity and claim denials are easier to understand.
What is Medicare review contractor?
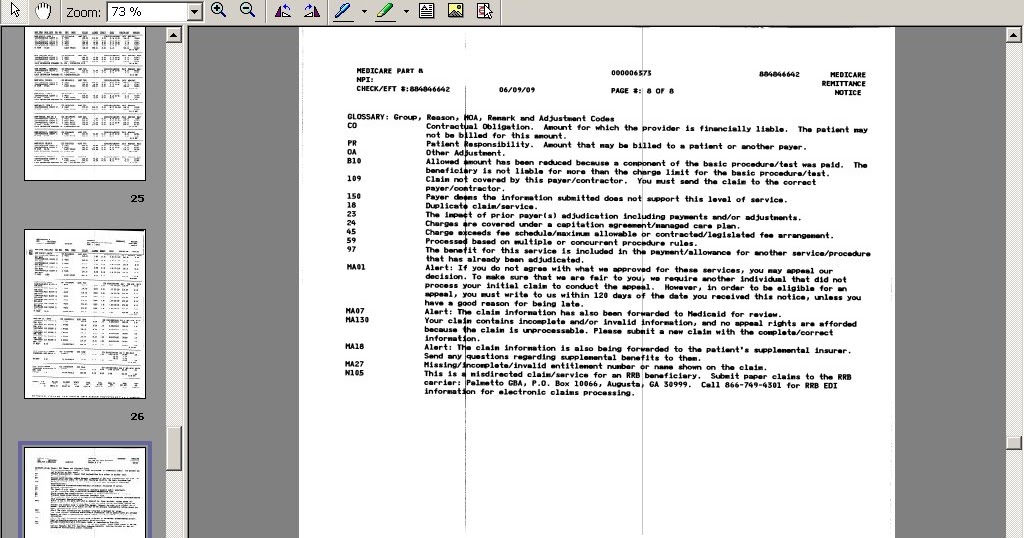
Historically, Medicare review contractors (Medicare Administrative Contractors, Recovery Audit Contractors and the Supplemental Medical Review Contractor) developed and maintained individual lists of denial reason codes and statements. If you deal with multiple CMS contractors, understanding the many denial codes and statements can be hard. In 2015 CMS began to standardize the reason codes and statements for certain services. As a result, providers experience more continuity and claim denials are easier to understand.
What does CMS review?
CMS contractors medically review some claims (and prior authorizations) to ensure that payment is billed (or authorization requested) only for services that meet all Medicare rules.
What is a Medicare denial code?
Medicare denial code - Full list - Description. Medicare denial code and Description. A group code is a code identifying the general category of payment adjustment. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service.
What is a CO code?
CO or contractual obligations is the group code that is used whenever the contractual agreement existing between the payee and payer or the regulatory requirement has resulted in a proper adjustment.
How many charges are adjusted for failure to obtain second surgical opinion?
61 Charges adjusted as penalty for failure to obtain second surgical opinion.
Do 40 charges meet the criteria for emergent care?
40 Charges do not meet qualifications for emergent/urgent care.
What precedes the date of service?
13 The date of death precedes the date of service.
Is a 47 diagnosis covered?
47 This (these) diagnosis ( es) is ( are) not covered, missing, or are invalid.
What does code mean in Medicare?
Code indicates the amount of Medicare additional payment for new technology.
When reporting numeric values that do not represent dollars and cents, what do you do?
When reporting numeric values that do not represent dollars and cents, put whole numbers to the left of the dollar/cents delimiter and tenths to the right of the delimiter.
What is the primary payer code for Medicare Part A?
Beneficiary must have Medicare Part A entitlement (enrolled in Part A) for this provision to apply. Primary Payer Code = G.
What is primary payer code?
Primary Payer Codes Primary Payer codes are not reported by the provider via electronic submission of a MSP claim. Primary Payer codes are applied to the claim upon transfer to the Fiscal Intermediary Standard System (FISS) based on the corresponding electronic data reported. Primary Payer Codes of A to L (except C) must match MSP VC reported on claim. For example, MSP VC 12 = Primary Payer Code A, etc.
What is a date of denied insurance?
Date Insurance denied - Date of receipt of a denial of coverage by a higher priority payer. This could be date of primary payer's Explanation of Benefit (EOB) statement, letter or other documentation. Date is required on all Conditional Payment claims.
What is the VC code for accident related to employment?
Accident/Employment-Related - Date of an accident/injury related to beneficiary's employment. Reported with VC 15 or VC 41. If filing for a Conditional Payment, report with Occurrence Code 24.
What is the code for no fault insurance?
Reported with VC 14 or 47. If filing for a Conditional Payment, report with Occurrence Code 24.
What is the VC code for conditional payment?
Accident/Medical Payment Coverage – Date of accident/injury for which there is medical payment coverage. Reported with VC 14 or VC 47. If filing for a Conditional Payment, report with Occurrence Code 24.
Is EGHP secondary to Medicare?
To navigate directly to a particular type of code, click on the type of code from the following list: Beneficiary's and/or spouse's EGHP is secondary to Medicare. Beneficiary and/or spouse are employed and there is an EGHP that covers beneficiary but either:
Thursday, December 2, 2010
Note : When using “AT05”, indicating a Medicare payment, please remember to properly complete and attach the "Supplemental Medicare Attachment for Providers" form (MA-539).
AT 05, AT99, AT26 adjustment remark codes
Note : When using “AT05”, indicating a Medicare payment, please remember to properly complete and attach the "Supplemental Medicare Attachment for Providers" form (MA-539).
How often do Medicare summary notices come out?
Medicare Summary Notices are sent out four times a year — once a quarter — but you don't have to wait for your notice to arrive in the mail. You can also check your account online at MyMedicare.gov. Claims typically appear on your electronic statement 24 hours after processing. 6.
What is deductible status 8?
Your Deductible Status 8 Your deductible is what you must pay for most health services before Medicare begins to pay.
How to get a medical billing statement?
Medical procedures and services are assigned billing codes. You have the right to receive an itemized billing statement that lists each medical service you received. If you need an itemized statement, contact your doctor. Compare the billing code on your MSN with the code that appears on the billing statement you received from your doctor. If the codes are different, or if you didn't receive the medical service indicated, contact the doctor who is making the claim. It may be a simple mistake that the doctor's office can easily correct. If the office does not resolve your concerns, call Medicare at 1-800-MEDICARE (1-800-633-4227).
How to contact Medicare if you have questions about your doctor?
If you have questions, contact the doctor who is filing the claim. If the doctor's office cannot resolve your concerns, contact Medicare at 1-800-MEDICARE (1-800-633-4227).
How much is deductible for Medicare?
Each year you must pay a deductible ($183 in 2017) for health services before Medicare begins to pay. This section shows how much of this annual deductible you have paid.
How to contact Medicare for more information?
Call 1-800-MEDICARE (1-800-633-4227) for more information about a coverage or payment decision on this notice, including laws or policies used to make the decision.
Does Medicare send quarterly statements?
Medicare sends out statements like this example quarterly. If you didn't use any medical services in a particular three-month period, a statement won't be sent. Your Medicare Summary Notice shows all services billed to your Medicare Part B account for doctors' services, tests, outpatient care, home health services, durable medical equipment, preventive services and other medical services.
What is discharge status code 50?
Patient discharge status Code 50 should be used if the patient went to his/her own home or an alternative setting that is the patient’s “home,” such as a nursing facility, and will receive in-home hospice services.
When to use a leave of absence code?
This code is used when the patient is still within the same facility and is typically used when billing for leave of absence days or interim bills. It can be used for both inpatient or outpatient claims.
What is LTCH code?
This code is for hospitals that meet the Medicare criteria for LTCH certification. LTCHs are facilities that provide acute inpatient care with an average length of stay of 25 days or greater.
Can a nursing facility certify a bed under Medicare?
Nursing facilities may elect to certify only a portion of their beds under Medicare, and some nursing facilities choose to certify all of their beds under Medicare. Still others elect not to certify any of their beds under Medicare.