
The CO16 denial code alerts you that there is information that is missing in order for Medicare to process the claim. Due to the CO (Contractual Obligation) Group Code, the omitted information is the responsibility of the provider and, therefore, the patient cannot be billed for these claims.
What is the co-16 denial code for Medicare?
In my experience with Medicare, the denial code CO-16 is typically used when more information is needed pertaining to the claim. This is not a specific type of information, and it could be different information is needed for each claim denied with this code.
What is the denial code for Medicare claim?
Medicare denial code CO 16, M67, M76, M79, MA120, MA 130, N10. CO - 16 denial and remark code. Claim/service lacks information which is needed for adjudication. This denial code is just intimation that claims has been denied for lack of some information and it always come with other rejection code as given below.
What to do if you receive a co16 from a payer?
When you receive a CO16 from a commercial payer, as stated above, the first place to look would be at any remark code present on the ERA, paper EOB or even the payer’s website. If the reason for the denial is not detailed enough in a remark code, the next step would be to contact the payer to see what information is required.
What does CARC co 16 apply to?
A: CARC CO 16 applies to various scenarios regarding missing or invalid information on the claim. To avoid delay in payment, submit a corrected claim. Claims that are returned as unprocessable cannot be appealed, as an initial determination was not made.
What is denial code Co 16?
The CO16 denial code alerts you that there is information that is missing in order for Medicare to process the claim. Due to the CO (Contractual Obligation) Group Code, the omitted information is the responsibility of the provider and, therefore, the patient cannot be billed for these claims.
How do you handle a co 16 denial?
To resolve this denial, the information will need to be added to the claim and rebilled. For commercial payers, the CO16 can have various meanings. It is primarily used to indicate that some other information is required from the provider before the claim can be processed.
What does denial code CO mean?
Contractual ObligationWhat does the denial code CO mean? CO Meaning: Contractual Obligation (provider is financially liable).
What does co24 mean?
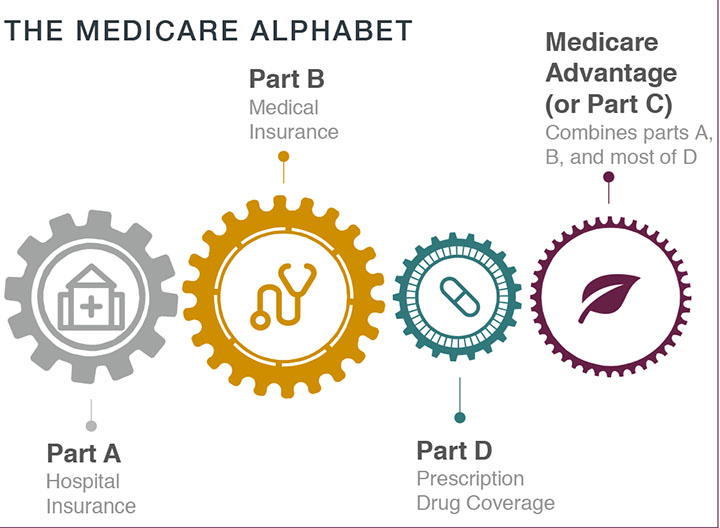
CO 24 – charges are covered under a capitation agreement/managed care plan: This reason code is used when the patient is enrolled in a Medicare Advantage (MA) plan or covered under a capitation agreement. This claim should be submitted to the patient's MA plan.
What is remark code m16?
That's what the denial code means.... your payer has made a recent determination or change with regards to that particular service, claim or adjudication process, and has made notification of that on their website.
What are the top 10 denials in medical billing?
These are the most common healthcare denials your staff should watch out for:#1. Missing Information. You'll trigger a denial if just one required field is accidentally left blank. ... #2. Service Not Covered By Payer. ... #3. Duplicate Claim or Service. ... #4. Service Already Adjudicated. ... #5. Limit For Filing Has Expired.
What are group codes PR and co?
Group codes are codes that will always be shown with a reason code to indicate when a provider may or may not bill a beneficiary for the non-paid balance of the services furnished. PR (Patient Responsibility). CO (Contractual Obligation).
What does co mean in billing?
Contractual ObligationsCO (Contractual Obligations) is the amount between what you billed and the amount allowed by the payer when you are in-network with them. This is the amount that the provider is contractually obligated to adjust off.
What is Medicare denial code Co 22?
In circumstances where there is more than one potential payer, not submitting claims to the proper payer will lead to denial reason code CO-22, indicating this care may be covered by another payer, per COB.
What does covered under capitation mean?
What Is a Capitated Contract? A capitated contract is a healthcare plan that allows payment of a flat fee for each patient it covers. Under a capitated contract, an HMO or managed care organization pays a fixed amount of money for its members to the health care provider.
What does denial code Co 23 mean?
CO 23 Payment adjusted because charges have been paid by another payer.
What does denial code Co 97 mean?
Denial Code CO 97 – Procedure or Service Isn't Paid for Separately. Denial Code CO 97 occurs because the benefit for the service or procedure is included in the allowance or payment for another procedure or service that has already been adjudicated. Basically, the procedure or service is not paid for separately.
Sunday, February 6, 2011
CO - 16 denial and remark code. Claim/service lacks information which is needed for adjudication. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT)
Medicare denial code CO 16, M67, M76, M79, MA120, MA 130, N10
CO - 16 denial and remark code. Claim/service lacks information which is needed for adjudication. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT)
Is N104 payable under CMS?
N104: This claim service is not payable under our claims jurisdiction area. You can identify the correct Medicare contractor to process this claim/service through the CMS website at https://www.cms.gov/Medicare/Medicare-Contracting/Medicare-Administrative-Contractors/Who-are-the-MACs .
Can a Medicare procedure code be changed?
Be aware that code status may change, so a procedure code that was previously valid for Medicare may no longer be valid. • If the procedure code has an “I” status, the procedure code is not valid for Medicare and should not be billed unless documentation is needed for a secondary payer or supplemental plan.
What does a CO16 denial mean?
A CO16 denial does not necessarily mean that information was missing. It could also mean that specific information is invalid. For example, in 2014, after the implementation of the PECOS enrollment requirement, DMEPOS providers began to see CO16 denials when the ordering physician was not enrolled in PECOS. The N264/N575 remark codes are used ...
What does M124 mean on a Medicare claim?
If you encounter the M124 remark code on the explanation of benefits, it means that there is a missing indication of whether the patient owns the equipment that requires the part or supply. This could be received in the case of a new fee-for-service Medicare patient that did not have their base equipment billed through Medicare, and the provider is attempting to bill supplies or accessories. Medicare requires in those instances that the following information is added to box 19 on the CMS-1500 form or the NTE field for electronic claims: HCPCS code of the base equipment, a notation that the beneficiary owns the equipment and the date the patient received the equipment. This information would also be required on repair items where Medicare did not pay for the base equipment.
What is PR42 in Medicare?
PR42 with the amount that is the difference between the allowed amount and the limiting charge for which the beneficiary is liable; if excess payment made by the beneficiary. Common Reasons for Message. Item or service paid Medicare allowed amount. Item or service paid to patient’s deductible and/or coinsurance.
What is Medicare item or service?
Item or service paid Medicare allowed amount. Item or service paid to patient’s deductible and/or coinsurance. Item or services paid with partial unit. Explanation and solutions – It means that the billed which is more than Medicare allowed amount is adjustment. Just write it off. Generally this code comes in paid claim.
Is Medicare claim N104 payable?
N104: This claim service is not payable under our claims jurisdiction area. You can identify the correct Medicare contractor to process this claim/service through the CMS website at https://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/Categorization_of_Tests.html external link.
Is a procedure code valid for Medicare?
Be aware that status codes may change, so a procedure code that was previously valid for Medicare or for PQRS reporting may no longer be valid. • If the procedure code has an “I” status, the procedure code is not valid for Medicare or for PQRS reporting.