
What items are covered by Medicare?
What Medicare health plans cover Preventive & screening services What's not covered by Part A & Part B Medicare Part A coverage–hospital care Inpatient hospital care Skilled nursing facility …
Is there a deductible for Medicare Part A?
Jan 06, 2022 · One of the most basic coverages provided under Medicare Part A is inpatient care in a hospital or rehabilitation facility. It also provides coverages related to inpatient mental health care, if this type of treatment is needed. A few of the inpatient expenses covered by Medicare Part A include: General nursing staff Medications used while in care
How long will Medicare pay for a hospital stay?
Jan 30, 2022 · Medicare Part A covers the majority of medically necessary inpatient care. Within the first 60 days of your Part A deductible when you incur an authorized facility charge, Medicare Part A pays 100% of the deductible for covered hospital stays, hospices, or short stays at skilled nursing facilities.
How much does Medicare pay for hospital stays?
May 06, 2021 · Here’s a look at the health-care costs that Original Medicare (Part A and Part B) may cover. If you’re an inpatient in the hospital: Part A (hospital insurance) typically covers health-care costs such as your care and medical services. You’ll usually need to pay a deductible ($1,484 per benefit period* in 2021).
Does Medicare cover hospital expenses?
What is typically not covered by Medicare?
Does Medicare pay for food?
Does Medicare cover eye exams?
Medicare doesn't cover eye exams (sometimes called “eye refractions”) for eyeglasses or contact lenses. You pay 100% for eye exams for eyeglasses or contact lenses.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
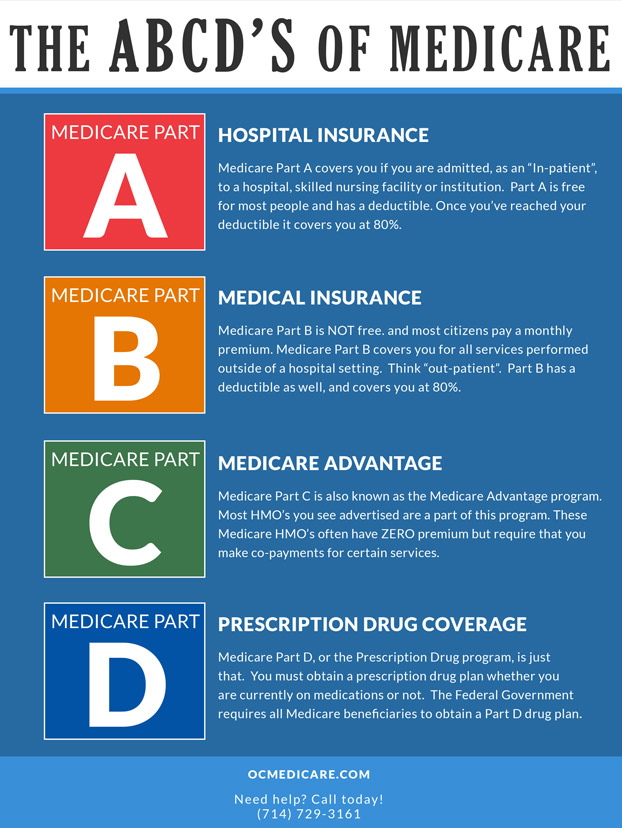
Medicare Part A Coverage
Medicare.gov explains that Medicare Part A is often referred to as “Hospital Insurance.” Rightfully so, as this is the part of Medicare that covers expenses related to hospital, nursing facility care, hospice, and home health care.
Medicare Part B Coverage
Part B is the “Medical Insurance” piece of Medicare and covers most preventative services fully. It also provides at least partial coverage for medically necessary services and supplies needed to diagnose and/or treat existing conditions. Part B also pays a set amount toward other expenses, such as:
Medicare Part C Coverage
As an alternative to purchasing Part A and Part B, some participants receive Medicare benefits through Part C, which is commonly known as Medicare Advantage. Instead of the federal government providing healthcare coverage, Medicare Advantage’s benefits are offered through private insurance companies that have been pre-approved by Medicare.
Medicare Part D Coverage
Part D refers to the prescription drug coverage portion of Medicare and each plan has its own set of covered drugs. Additionally, each drug is placed in a designated tier within that plan, which ultimately determines the copayment and/or coinsurance cost of the drug.
Medicare Supplement (Medigap) Coverage
Medicare Supplement policies, also known as Medigap, are designed to help cover expenses not covered under Original Medicare Parts A and B.
What Medicare Does Not Cover
Medicare as a whole covers a wide variety of physical and mental health services—whether in whole or in part—but there are some expenses it will not pay toward. Among them are:
Which Part Of Medicare Helps With Inpatient Hospitalization?
Part A may be required to provide hospitalization care or skilled nursing treatment at a skilled nursing facility, hospice care, or home health care for a number of reasons.
What Is Medicare Part A And Part B Mean?
It covers treatment in hospitals as well as patients’ stays in hospitals. The purpose of Part B is to provide outpatient or medical coverage. Obtain Medicare Part C benefits on a sliding scale (click below for more info). It provides prescriptions for prescription drugs.
Which Part Of Medicare Covers Hospital Stays Up To 60 Days?
A patient that stays at a public hospital for 90 days is eligible to receive 60 years of inpatient hospitalization coverage if eligible for Inpatient Hospital Care. In general, Medicare will not renew the lifetime reserve days if you use them.
Does Medicare Part A Cover 100 Hospitalization?
Medicare Part A covers the majority of medically necessary inpatient care. Within the first 60 days of your Part A deductible when you incur an authorized facility charge, Medicare Part A pays 100% of the deductible for covered hospital stays, hospices, or short stays at skilled nursing facilities.
What Is Medicare Part C Used For?
An appointment with an eye doctor as part of your Medicare Part C outpatient coverage. It is always necessary to transport emergency patients by ambulance. Wheelchairs and equipment for the home oxygen system are made of durable materials. Care for the elderly in the emergency room.
What Is Medicare Part B Known As?
Original Medicare Part B, also called medical insurance, covers services and supplies for medical conditions that you must treat medically. See “Medicare and You” for a breakdown of preventive services covered under Part B.
Does Medicare Part B Cover Inpatient Services?
As part of longstanding Medicare policy, the United States pays a relatively limited number of ancillary services on admission to a hospital as inpatient services for Part B payments unless a Part A claim submitted by a hospital for an Outpatient Acute Treatment is denied.
What does Medicare cover?
Medicare coverage: what costs does Original Medicare cover? Here’s a look at the health-care costs that Original Medicare (Part A and Part B) may cover. If you’re an inpatient in the hospital: Part A (hospital insurance) typically covers health-care costs such as your care and medical services. You’ll usually need to pay a deductible ($1,484 per ...
Does Medicare have a maximum spending limit?
Be aware that Original Medicare has no annual out-of-pocket maximum spending limit. If you meet your Medicare Part A and/or Part B deductibles, you still generally pay a coinsurance or copayment amount – and there’s no limit to what you might pay in a year.
Does Medicare cover prescription drugs?
Medicare Part A and Part B don’ t cover health-care costs associated with prescription drugs except in specific situations. Part A may cover prescription drugs used to treat you when you’re an inpatient in a hospital. Part B may cover medications administered to you in an outpatient setting, such as a clinic.
Does Medicare Supplement cover Part A and Part B?
If you’re concerned about how much Original Medicare (Part A and Part B) doesn’ t typically cover, you might want to learn about Medicare Supplement (Medigap) insurance. This type of insurance works alongside your Original Medicare coverage. Medicare Supplement insurance plans typically help pay for your Medicare Part A and Part B out-of-pocket ...
What type of insurance is used for Medicare Part A and B?
This type of insurance works alongside your Original Medicare coverage. Medicare Supplement insurance plans typically help pay for your Medicare Part A and Part B out-of-pocket costs, such as deductibles, coinsurance, and copayments.
How much does Medicare Supplement pay for hospital visits?
(Under Medicare Supplement Plan N, you might have to pay a copayment up to $20 for some office visits, and up to $50 for emergency room visits if they don’t result in hospital admission.)
Does Medicare Advantage work?
To answer that question, here’s a quick rundown on how the Medicare Advantage (Medicare Part C) program works. When you have a Medicare Advantage plan, you still have Medicare – but you get your Medicare Part A and Part B benefits through the plan, instead of directly from the government.
What is Medicare Part A?
Medicare Part A is also called "hospital insurance," and it covers most of the cost of care when you are at a hospital or skilled nursing facility as an inpatient. Medicare Part A also covers hospice services. For most people over 65, Medicare Part A is free. The following list gives you an idea of what Medicare Part A pays for, ...
Does Medicare cover hospice?
Medicare Part A also covers hospice services. For most people over 65, Medicare Part A is free. The following list gives you an idea of what Medicare Part A pays for, and does not pay for, during your stay in a participating hospital. However, even when Part A covers a cost, there are significant financial limitations on the length of coverage, ...
Does Medicare cover a semiprivate room?
When you are admitted to a hospital or skilled nursing facility, Medicare Part A hospital insurance will cover the following for a certain amount of time: • a semiprivate room (two to four beds per room), or a private room if medically necessary. • all meals, including special, medically required diets.
How many days can you use Medicare lifetime reserve?
If you are in the hospital more than 90 days during one spell of illness, you can use up to 60 additional "lifetime reserve" days of coverage. During those days, you are responsible for a daily coinsurance payment of $704 per day in 2020. Medicare pays the rest of covered costs.
How many reserve days do you have to use for Medicare?
You do not have to use your reserve days in one spell of illness; you can split them up and use them over several benefit periods. But you have a total of only 60 reserve days in your lifetime. (Note: If you have a Medicare Advantage Plan, called Medicare Part C, you may not have to pay ...
Does Medicare cover skilled nursing?
Skilled Nursing Facilities and Home Health Care. Under some circumstances, Medicare will cover some of the cost of inpatient treatment in a skilled nursing facility or visits from a home health care agency. Your stay in a skilled nursing home facility or home health care is covered by Medicare Part A only if you have spent three consecutive days, ...
Does Medicare cover home health care?
Under some circumstances, Medicare will cover some of the cost of in patient treatment in a skilled nursing facility or visits from a home health care agency. Your stay in a skilled nursing home facility or home health care is covered by Medicare Part A only if you have spent three consecutive days, not counting the day of discharge, in the hospital.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What is medically necessary?
Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What is preventive care?
Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best. You pay nothing for most preventive services if you get the services from a health care provider who accepts. assignment.
Does Medicare cover hospital stays?
Medicare Part A can help provide coverage for hospital stays. You’ll still be responsible for deductibles and coinsurance. A stay at the hospital can make for one hefty bill. Without insurance, a single night there could cost thousands of dollars. Having insurance can help reduce that cost.
Does Medicare Part A cover inpatient care?
If you’re eligible for Medicare, Medicare Part A can provide some coverage for inpatient care and significantly reduce costs for extended hospital stays. But in order to receive the full scope of benefits, you may need to pay a portion of the bill. Keep reading to learn more about Medicare Part A, hospital costs, and more.
What is Medicare Part A?
Medicare Part A, the first part of original Medicare, is hospital insurance. It typically covers inpatient surgeries, bloodwork and diagnostics, and hospital stays. If admitted into a hospital, Medicare Part A will help pay for:
How much does Medicare Part A cost in 2020?
In 2020, the Medicare Part A deductible is $1,408 per benefit period.
What is the Medicare deductible for 2020?
Even with insurance, you’ll still have to pay a portion of the hospital bill, along with premiums, deductibles, and other costs that are adjusted every year. In 2020, the Medicare Part A deductible is $1,408 per benefit period.
How much is Medicare Part A deductible for rehabilitation?
In 2020, the Medicare Part A deductible is $1,408 per benefit period.
How long does Medicare Part A deductible last?
Unlike some deductibles, the Medicare Part A deductible applies to each benefit period. This means it applies to the length of time you’ve been admitted into the hospital through 60 consecutive days after you’ve been out of the hospital.
Does Medicare cover observation?
Medicare typically does cover observation in a hospital if it is deemed medically necessary by a doctor, but it’s very important that you understand how observation status may affect your out-of-pocket Medicare costs. Medicare Advantage (Part C) plans may also cover observation in a hospital if it’s ordered by your doctor.
Does Medicare Advantage have an out-of-pocket spending limit?
Original Medicare does not include an out-of-pocket spending limit.
Does Medicare pay for outpatient lab tests?
If you receive observation services in a hospital, Medicare Part B (medical insurance) will typically pay for your doctor services and hospital outpatient services (such as lab tests and IV medication) received at the hospital. There are some important things you should know about what hospital observation status means for your Medicare coverage: ...
Does Medicare cover hospital costs?
Because your doctor hasn’t formally admitted you as an inpatient, Medicare Part A will not cover your hospital costs. Part B will typically cover the costs of your doctor services (such as certain tests like an EKG or ECG). If you were to be formally admitted for inpatient care, Part A typically covers your hospital costs ...
Does Medicare Part A cover inpatient care?
If you were to be formally admitted for inpatient care, Part A typically covers your hospital costs and your inpatient services at a hospital . If you are initially kept in the hospital for observation care but then are admitted for inpatient care, you will switch from outpatient to inpatient status. Medicare Part A will cover your hospital costs, ...
Does Medicare cover SNF?
If you were to need extended care from a skilled nursing facility (SNF) after receiving hospital observation, Medicare Part A might not cover these costs. In order for Medicare Part A to cover your skilled nursing facility costs, you must have a qualified inpatient hospital stay of at least three days before being admitted to ...
How much does Medicare pay for hospital observation?
You typically must pay a 20 percent coinsurance for your Part B-covered care after you meet the Part B deductible (which is $185 for the year in 2019).
