
How much does Medicaid pay for health care?
Mar 11, 2022 · That's $12,530 per person. This figure accounted for 19.7% of gross domestic product (GDP) that year. If we look at each program individually, Medicare spending grew 3.5% to $829.5 billion in 2020...
What is the Medicare-Medicaid alignment initiative?
Medicare Medicaid Alignment Initiative (MMAI) plan, and this is when participant confusion and ... Eliminate cost shifting between Medicare and Medicaid. ... enrolled in the Limited Income NET Program, but the 4Rx data are not yet available on Medicare’s system. If this is the case, please contact LINET (contact provided below) and use the ...
How much does Medicare cost the United States?
The Illinois Medicare -Medicaid Alignment Initiative (MMAI) is a demonstration designed to improve ... • Eliminate cost shifting between Medicare and Medicaid. ... • Do not participate in the Illinois Medicaid Breast and Cervical Cancer program; and • Do not have Comprehensive Third Party Insurance.
How is Medicare and Medicaid funded?
Aug 20, 2020 · Being over Medicaid’s income limit (approximately $2,349 / month in 2020 for nursing home Medicaid and home and community based services via a Medicaid waiver) is not automatic cause for Medicaid denial. Approximately half of the states allow Medicaid applicants to create irrevocable (cannot be cancelled or changed) qualified income trusts ...
Is Mmai better than Medicare?
MMAI plans should have more benefits, meaning they cover more services than traditional Medicare/Medicaid. However, they may not cover the same prescriptions that Medicare/Medicaid covered. In order to understand the coverage differences, you may contact any MMAI plan for details.Jun 10, 2021
Who is eligible for Mmai in Illinois?
MMAI plans will be available to Illinois residents who: • Are residents of the Greater Chicago or Central Illinois regions and; • Are at least age 21, entitled to Medicare Part A, and enrolled in Medicare Parts B and D; • Are eligible for full Medicaid benefits; • Are enrolled in the Medicaid Aid to the Aged, Blind, ...
What does Mmai mean in insurance?
The Medicare-Medicaid Alignment Initiative (MMAI) is a statewide program for adults who are enrolled in both Medicare and Medicaid. When you enroll, you will choose a primary care provider (PCP) and health plan to cover all your healthcare.
What is financial alignment initiative?
The Financial Alignment Initiative (FAI) was authorized under Section 3021 of the Patient Protection and Affordable Care Act (P.L. 111-148, as amended) to test ways to improve care for dually eligible beneficiaries and reduce program costs by aligning financing and coordinating care across Medicare and Medicaid.
Is Mmai a Medicare?
Yes. MMAI covers inpatient and outpatient prescription drugs and other medications and equipment covered under Medicare Parts B and D and Medicaid.
Can you have both Medicare and Medicaid in Illinois?
Illinois residents who are eligible for Medicare and Medicaid coverage and benefits can get it all through Humana Gold Plus® Integrated Medicare-Medicaid in Illinois. Through Humana Gold Plus Integrated, your Medicare and Medicaid coverage and benefits are combined into one plan—PLUS you get prescription drug coverage.Jan 1, 2022
What is Humana Gold Plus integrated?
The Humana Gold Plus Integrated plan combines your Medicare and Medicaid services, PLUS it includes coverage for prescription drugs. Some advantages include: You get the coverage of original Medicare PLUS extra benefits like rides to medical appointments, and added vision, hearing, and dental coverage.Jan 1, 2022
What is the income limit for Medicaid in Illinois 2022?
This may include medical care/treatment/supplies, nursing home services, in-home personal care, Medicare premiums, and prescription drugs. Effective April 2022 – March 2023, the medically needy income limit (MNIL) in IL is $1,133 / month for an individual and $1,526 / month for a couple.Mar 25, 2022
What is HealthChoice Illinois?
HealthChoice Illinois is the statewide Medicaid managed care program. Most Medicaid customers are required to choose a primary care provider (PCP) and health plan. We can help you understand your plan choices, find providers and enroll.
What is D SNP?
Dual Eligible Special Needs Plans (D-SNPs) enroll individuals who are entitled to both Medicare (title XVIII) and medical assistance from a state plan under Medicaid (title XIX). States cover some Medicare costs, depending on the state and the individual's eligibility.Dec 1, 2021
What is the goal of Medicare and Medicaid?
Advancing Care for People with Medicaid and Medicare Our goal is to make sure dually eligible individuals have full access to seamless, high quality health care and to make the system as cost-effective as possible.Mar 10, 2022
How do you qualify for Medicaid and Medicare?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).Feb 11, 2022
What is the Medicare-Medicaid Alignment Initiative?
The Medicare-Medicaid Alignment Initiative is one of Illinois' managed care programs. This program is for seniors and persons with disabilities who have full Medicaid and Medicare benefits.
Why is the Medicare-Medicaid Alignment Initiative important for me?
The Medicare-Medicaid Alignment Initiative brings together all of your Medicare, Medicaid, and prescription drug benefits into one health plan. In the Medicare-Medicaid Alignment Initiative, you choose a health plan that is best for you.
Can I enroll in the Medicare-Medicaid Alignment Initiative?
Getting full Medicaid and Medicare benefits (Medicare Parts A and B and Medicaid without a spenddown),
How do I know which health plan is the right plan for me?
To choose the best health plan for you, you should think about your answers to these questions:
How do I enroll in the Medicare-Medicaid Alignment Initiative?
You can enroll in the Medicare-Medicaid Alignment Initiative at any time. To enroll in this program, call Illinois Client Enrollment Services at 1-877-912-8880 (TTY 1-866-565-8576). Call Monday to Friday, 8 a.m. to 7 p.m. The call is free!
What happens after I enroll in the Medicare-Medicaid Alignment Initiative?
Once you enroll in a Medicare-Medicaid Alignment Initiative health plan, you will get a health plan member handbook and a member ID card. Look for them in the mail. You will work with your health plan care coordinator to get the health care services you need. To learn more, call your health plan member services number.
What is medicaid?
Medicaid is a joint federal and state program that: 1 Helps with medical costs for some people with limited income and resources 2 Offers benefits not normally covered by Medicare, like nursing home care and personal care services
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is extra help?
And, you'll automatically qualify for. Extra Help. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying for your.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
Does medicaid pay first?
Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second. Medicaid never pays first for services covered by Medicare. It only pays after Medicare, employer group health plans, and/or Medicare Supplement (Medigap) Insurance have paid.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
What is the agency that administers Medicare?
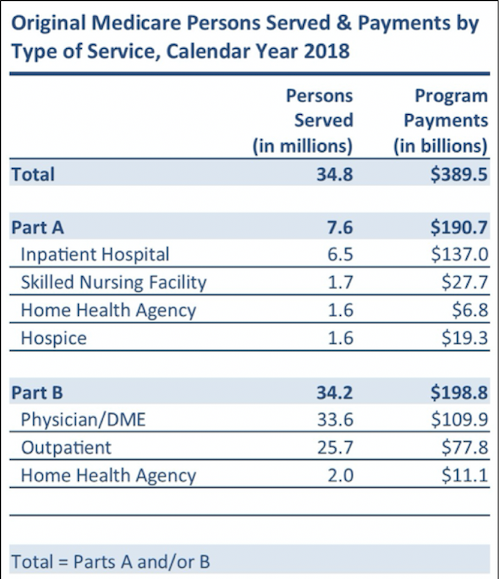
To grasp the magnitude of the government expenditure for Medicare benefits, following are 2018 statistics from the Centers for Medicare & Medicaid Services (CMS), which is the agency that administers Medicare:
Does Medicare pay payroll taxes?
Additionally, Medicare recipients have seen their share of payroll taxes for Medicare deducted from their paychecks throughout their working years.
How long does it take to get medicaid?
The Medicaid application process can take up to 3 months, or even longer, from the beginning of the application process through the receipt of the determination letter indicating approval or denial. Generally, it takes one several weeks to complete the application and gather all of the supportive documentation. If the application is not properly completed, or required documentation is missing, the application process will be delayed even further. In most cases, it takes between 45 and 90 days for the Medicaid agency to review and approve or deny one’s application. Based on law, Medicaid offices have up to 45 days to complete this process (up to 90 days for disability applications). However, despite the law, applications are sometimes delayed even further.
What counties are eligible for Medicare in Illinois?
At the time of this writing, one must reside in one of the following 21 counties: Champaign, Christian, Cook, DeWitt, DuPage, Ford, Kane, Kankakee, Knox, Lake, Logan, Macon, McLean, Menard, Peoria, Piatt, Sangamon, Stark, Tazewell, Vermilion, or Will. Please note that this program will be available statewide beginning July 1, 2021. Additional eligibility criteria are as follows, alternatively one can take a quick, non-binding IL Medicaid eligibility test here.
What is an MCO in Illinois?
A MCO is essentially a private healthcare company. The MCO has a network of care providers and program participants receive services via these providers. Within several counties of Illinois, there are a few managed care plans from which to choose. The Medicare-Medicaid Alignment Initiative is a mandatory Medicaid program for persons who require ...
How to apply for MMAI in Illinois?
To apply for the MMAI, one must apply for IL Medicaid. This can be done via one’s local Department of Human Services’ Family Community Resource Center (FCRC). One can find their local office here. Alternatively, persons can call the Bureau of Customer Inquiry and Assistance at 1-800-843-6154 to locate one’s local office. A needs assessment will be completed as part of the application process to determine if the nursing home level of care need is met.
What is the income limit for 2021?
In 2021, an applicant, regardless of marital status, can have a monthly income up to $1,073. When both spouses are applicants, the monthly income limit for the couple is $1,452.
How much can a spouse keep on Medicaid?
In this case, the applicant spouse can retain up to $2,000 in assets and the non-applicant spouse can keep up to $109,560. This larger allocation of assets to the non-applicant spouse is called a community spouse resource allowance. Some assets are not counted towards Medicaid’s asset limit.
How long does it take for a medicaid application to be approved?
In most cases, it takes between 45 and 90 days for the Medicaid agency to review and approve or deny one’s application. Based on law, Medicaid offices have up to 45 days to complete this process (up to 90 days for disability applications). However, despite the law, applications are sometimes delayed even further.
What is the MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid.
Who is covered by Medicaid?
To participate in Medicaid, Congress requires states to cover specified groups, among them low-income families, qualified pregnant women and children, and people receiving Supplemental Security Income (SSI). The list goes on; states may choose to cover individuals receiving home- and community-based services, as well as children in foster care.
What are the different types of Medicare?
Medicare is divided into four parts: 1 Part A — hospital care 2 Part B — coverage for doctors, medical tests and procedures (requires a monthly premium) 3 Part C, Medicare Advantage — administered by private insurance companies, Part C is an alternative to traditional Medicare coverage, and often includes Parts A, B and D (prescription drugs) 4 Part D — administered by private insurance companies, Part D provides prescription drug coverage (requires a monthly premium); mandatory, unless you have coverage from another source
Why is my medicaid denied?
There are any number of reasons your application for Medicaid might be denied by your state’s Medicaid agency. Your income is too high. You hold disqualifying assets. The state doubts your claim of disability.
How many parts does Medicare have?
Medicare is divided into four parts: Medicaid, by contrast, is a needs-based public-assistance program paid for by taxes collected at the federal and state levels. Within the limits of certain federal mandates, Medicaid programs operate differently from state to state.
When did Obamacare come into effect?
With passage of the Affordable Care Act (a.k.a. ObamaCare) in 2010 accompanied by a fat infusion of funds from Washington, most states have extended Medicaid coverage to able-bodied, working-age, low-income childless adults. The response has been, to put it mildly, enormous.
How many states have medically needy programs?
In the 32 states and the District of Columbia that have adopted medically needy programs, a person can qualify for benefits if, after paying medical expenses, his/her income is reduced to such a low level the participating state declares the person eligible.
