
Medicare Part A is also called "hospital insurance," and it covers most of the cost of care when you are at a hospital or skilled nursing facility as an inpatient. Medicare Part A also covers hospice services. For most people over 65, Medicare Part A is free.
Full Answer
Do all hospitals accept Medicare coverage?
While not all hospitals accept Medicare assignments, the majority of inpatient hospitals do. Veterans hospitals and active duty hospitals don’t take Medicare for example, due to military personnel and veterans receiving their own medical benefits.
Does Medicare Part B cover inpatient hospital services?
Under longstanding Medicare policy, Medicare only pays for a limited number of ancillary medical and other health services as inpatient services under Part B when a Part A claim submitted by a hospital for payment of an inpatient admission is denied as not reasonable and necessary.
What does inpatient versus outpatient mean for Medicare?
When the doctor orders observation or tests to help with the diagnosis, you remain outpatient until inpatient admission. Outpatient is when you get care without admission or have for a stay of fewer than 24 hours, even if overnight. Health services you get at a facility can be outpatient care.
How much does Medicare cover for hospital stays?
Once the deductible is paid fully, Medicare will cover the remainder of hospital care costs for up to 60 days after being admitted. If you need to stay longer than 60 days within the same benefit period, you’ll be required to pay a daily coinsurance.
Does Medicare Part A cover hospitalizations?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Does Medicare Part A cover 100 of hospital stay?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
What does Medicare Part A services include?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What part of Medicare pays for inpatient procedures?
Medicare Part AMedicare Part A covers expenses related to inpatient hospital stays and surgeries. Typically, you'll receive an all-inclusive package of services when you're admitted to the hospital and pay the Part A deductible of $1,556 for a stay of up to 60 days. You'll also owe 20% of the doctor's charges.
What is not covered by Medicare Part A?
A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care. A television or telephone in your room, and personal items like razors or slipper socks, unless the hospital or skilled nursing facility provides these to all patients at no additional charge.
What is deductible for Medicare Part A?
Part A Deductible: The deductible is an amount paid before Medicare begins to pay its share. The Part A deductible for an inpatient hospital stay is $1,556 in 2022. The Part A deductible is not an annual deductible; it applies for each benefit period.
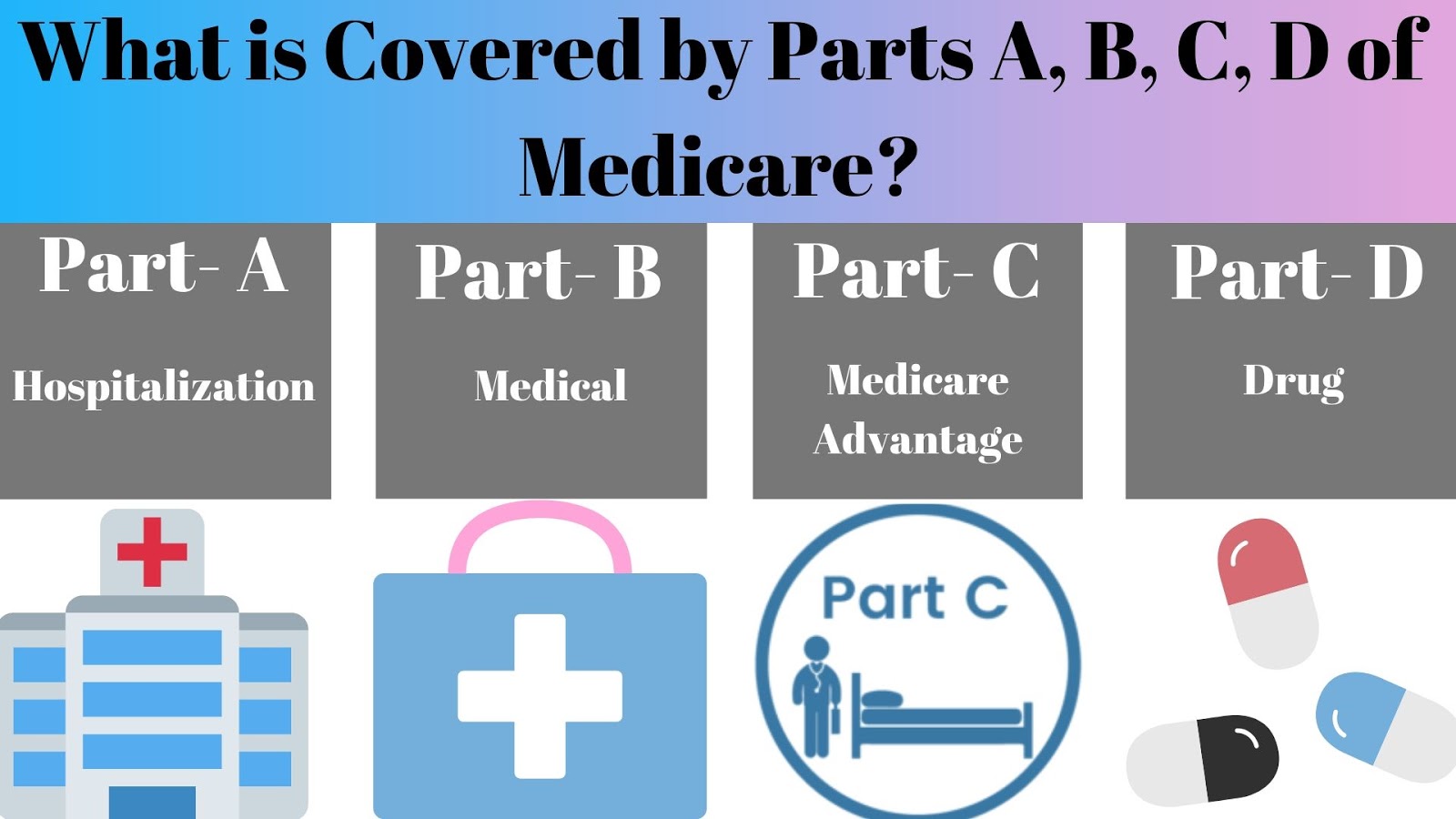
What is the difference between Medicare Part A and B?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers.
What is Medicare Part A and B mean?
Part A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
Which of the following is covered by Medicare Part A quizlet?
Medicare Part A provides coverage for inpatient hospital stays. Inpatient stays are those in which an individual must receive care or treatment in a hospital. Covered inpatient expenses include: semi-private room, meals, hospital services and supplies, drugs received during inpatient care, and general nursing services.
What procedures are on the inpatient only list?
Examples of Inpatient Only surgeries include: Coronary artery bypass grafting (CABG) Gastric bypass surgery for obesity. Heart valve repair or valve replacement.
What are inpatient only procedures?
“Inpatient-only” service is furnished, but the patient dies before inpatient admission or transfer to another hospital. The hospital reports the “inpatient only” service with modifier “CA” (Procedure payable only in the inpatient setting when performed emergently on an outpatient who expires prior to admission).
What is the maximum out-of-pocket expense with Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
What is Medicare Part A?
Medicare Part A coverage includes inpatient hospital stays you need to treat your health condition. The plan provides coverage for general nursing care, semi-private rooms, drugs received as an inpatient, and supplementary hospital supplies and services that are medically required for your care. The facilities where you can receive coverage include:
What is SNF Part A?
Part A provides coverage for inpatient stays in an SNF following a qualifying 3-day inpatient hospital stay. Before you can qualify for SNF coverage, your health condition must require daily skilled care that only an SNF can provide. Coverage for SNF stays include:
Does Medicare cover hospice?
Medicare provides hospice coverage for terminally ill Medicare beneficiaries. This service can be received either in an inpatient hospital facility or at home. Before you can qualify for hospice care, your doctor must prove that you are terminally ill and you only have six months or less to live. Also, you must agree to accept palliative care and relinquish restorative treatment. Finally, you must agree to accept hospice service instead of Medicare-approved care for your condition. Hospice services covered by Medicare Part A include:
Does Medicare cover mental health?
Medicare covers inpatient mental healthcare services, which include the care you receive in either a general or psychiatric hospital. If you receive doctor services while you are in a hospital, Medicare Part A will cover you. Similar to services received from the general hospital that Medicare Part A covers, mental health coverage includes a semi-private room, general nursing care, and meals.
What is Medicare Part A?
Medicare Part A – Hospital Insurance. Medicare Part A, often referred to as hospital insurance, is Medicare coverage for hospital care , skilled nursing facility care, hospice care, and home health services. It is usually available premium-free if you or your spouse paid Medicare taxes for a certain amount of time while you worked, ...
How long does Medicare cover nursing?
Original Medicare measures your coverage for hospital or skilled nursing care in terms of a benefit period. Beginning the day you are admitted into a hospital or skilled nursing facility, the benefit period will end when you go 60 consecutive days without care in a hospital or skilled nursing facility. A deductible applies for each benefit period.
How long does Medicare deductible last?
A deductible applies for each benefit period. Your benefit period with Medicare does not end until 60 days after discharge from the hospital or the skilled nursing facility. Therefore, if you are readmitted within those 60 days, you are considered to be in the same benefit period.
What is a skilled nursing facility?
A skilled nursing facility provides medically necessary nursing and/or rehabilitation services. To receive Medicare coverage for care in a skilled nursing facility: A physician must certify that you require daily skilled care that can only be provided as an inpatient in a skilled nursing facility. You must have been an inpatient in a hospital ...
How many days can a skilled nursing facility be covered by Medicare?
The facility must be Medicare-approved to provide skilled nursing care. Coverage is limited to a maximum of 100 days per benefit period, with coinsurance requirements of $164.50 per day in 2017 for Days 21 through 100. Coverage includes: A semiprivate room.
How much does Medicare pay for Grandpa's stay?
Grandpa is admitted to the hospital September 1, 2017. After he pays the deductible of $1,316, Medicare will pay for the cost of his stay for 60 days. If he stays in the hospital beyond 60 days, he will be responsible for paying $329 per day, with Medicare paying the balance.
What is home health care?
Home health care is care provided to you at home, typically by a visiting nurse or home health care aide. Medicare Part A covers medically necessary home health care offered by a provider certified by Medicare to provide home health care. Medicare pays the lower of:
What is Medicare Part A?
Medicare Part A is also called "hospital insurance," and it covers most of the cost of care when you are at a hospital or skilled nursing facility as an inpatient. Medicare Part A also covers hospice services. For most people over 65, Medicare Part A is free. The following list gives you an idea of what Medicare Part A pays for, ...
How much does Medicare pay for hospital bills?
Medicare Part A pays only certain amounts of a hospital bill for any one spell of illness. (And for each spell of illness, you must pay a deductible before Medicare will pay anything. In 2020, the hospital insurance deductible is $1,408.)
How many days can you use Medicare lifetime reserve?
If you are in the hospital more than 90 days during one spell of illness, you can use up to 60 additional "lifetime reserve" days of coverage. During those days, you are responsible for a daily coinsurance payment of $704 per day in 2020. Medicare pays the rest of covered costs.
How long does a skilled nursing home stay in the hospital?
Your skilled nursing stay or home health care must begin within 30 days of being discharged.
How long does Medicare cover psychiatric hospitals?
Psychiatric Hospitals. Medicare Part A hospital insurance covers a total of 190 days in a lifetime for inpatient care in a specialty psychiatric hospital (meaning one that accepts patients only for mental health care, not just a general hospital). If you are already an inpatient in a specialty psychiatric hospital when your Medicare coverage goes ...
How many reserve days do you have to use for Medicare?
You do not have to use your reserve days in one spell of illness; you can split them up and use them over several benefit periods. But you have a total of only 60 reserve days in your lifetime. (Note: If you have a Medicare Advantage Plan, called Medicare Part C, you may not have to pay ...
Does Medicare cover skilled nursing?
Skilled Nursing Facilities and Home Health Care. Under some circumstances, Medicare will cover some of the cost of inpatient treatment in a skilled nursing facility or visits from a home health care agency. Your stay in a skilled nursing home facility or home health care is covered by Medicare Part A only if you have spent three consecutive days, ...
What is Medicare Part A?
Medicare Part A generally covers inpatient medical services. This includes stays in a hospital or nursing facility. It also pays for some home care and hospice. Find a Medicare Plan that Fits Your Needs Get a Free Medicare Plan Review. Get Started.
How much does Medicare pay for hospital stays?
Hospital stays. The amount covered depends on how long you're in the hospital. In 2019, for the first 60 days, you pay a deductible of $1,364 for each benefit period and Medicare pays the rest. After that, the longer you stay, the more you pay. You pay $341 per day for days 61 through 90.
What happens if you don't pay Medicare taxes?
But if neither you nor your spouse worked and paid Medicare taxes for 10 years, you will have to pay an additional monthly fee depending on how long you worked. If you enroll late, you will be penalized by paying a higher monthly amount. Medicare Part A pays some of the charges for: Hospital stays.
How much does Medicare pay for skilled nursing?
Medicare pays in full for the first 20 days. From the 21st to 100th day, you pay a co-pay of $170.50 per day in 2019. After that, you pay all the costs of your stay in a skilled nursing facility. Home health care.
How long does skilled nursing care last?
Medicare will cover the cost of skilled nursing care for a maximum of 100 days. Medicare pays in full for the first 20 days.
How long do you have to sign up for Medicare Part B?
If your employer coverage ends, you have 8 months to sign up for Part B to avoid paying a higher premium . If you have a disability, Lou Gehrig's disease (ALS), or kidney failure, you may get Medicare even when you're younger than 65.
What is hospice care?
Hospice care. This covers some care for people who are terminally ill. Medicare Part A covers most drug costs, as well as medical and support services. Hospice care is usually given at home or in the facility where you live.
How much does Medicare cover inpatients?
Does Medicare Part A Cover 100 Percent? For a qualifying inpatient stay, Medicare Part A covers 100 percent of hospital-specific costs for the first 60 days of the stay — after you pay the deductible for that benefit period.
What is Medicare Part A?
Medicare Part A#N#Medicare Part A, also called "hospital insurance ," covers the care you receive while admitted to the hospital, skilled nursing facility, or other inpatient services. Medicare Part A is part of Original Medicare.#N#provides coverage to U.S. citizens age 65 and older for inpatient stays in hospitals and similar medical facilities.
How long does it take to pay coinsurance for Medicare?
After 60 days , you must pay coinsurance that Part A doesn’t cover. For hospital expenses covered by Part B, you have to pay 20 percent coinsurance after meeting your annual deductible. Part A and B are collectively known as Original Medicare and work hand-in-hand to help cover hospital stays.
How long does Medicare Part A and Part B last?
Your IEP begins three months before the month you turn 65. The IEP is open for a total of seven months and allows you to enroll in Medicare Part A and Part B.
Why is Medicare Part A called Medicare Part A?
Medicare Part A is commonly referred to as “hospital insurance” because its primary function is to help older adults manage the cost of hospital bills.
Do you have to pay Medicare premiums at 65?
If you, like most people, don’t have to pay a monthly premium for Part A, there is no downside to enrolling when you become eligible at age 65. You don’t have to pay a premium if you have paid Medicare taxes for at least 10 years.
Is short term care covered by Medicare?
Short-term care in a skilled nursing facility or nursing home may also be covered by Medicare Part A if it’s a doctor-approved treatment for a medical condition stemming from an inpatient hospital stay.
How long does an inpatient stay in the hospital?
Inpatient after your admission. Your inpatient hospital stay and all related outpatient services provided during the 3 days before your admission date. Your doctor services. You come to the ED with chest pain, and the hospital keeps you for 2 nights.
How does hospital status affect Medicare?
Inpatient or outpatient hospital status affects your costs. Your hospital status—whether you're an inpatient or an outpatient—affects how much you pay for hospital services (like X-rays, drugs, and lab tests ). Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility ...
What is an ED in hospital?
You're in the Emergency Department (ED) (also known as the Emergency Room or "ER") and then you're formally admitted to the hospital with a doctor's order. Outpatient until you’re formally admitted as an inpatient based on your doctor’s order. Inpatient after your admission.
When is an inpatient admission appropriate?
An inpatient admission is generally appropriate when you’re expected to need 2 or more midnights of medically necessary hospital care. But, your doctor must order such admission and the hospital must formally admit you in order for you to become an inpatient.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. , coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
Is an outpatient an inpatient?
You're an outpatient if you're getting emergency department services, observation services, outpatient surgery, lab tests, or X-rays, or any other hospital services, and the doctor hasn't written an order to admit you to a hospital as an inpatient. In these cases, you're an outpatient even if you spend the night in the hospital.
Does Medicare cover skilled nursing?
Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility (SNF) following your hospital stay. You're an inpatient starting when you're formally admitted to the hospital with a doctor's order. The day before you're discharged is your last inpatient day. You're an outpatient if you're getting ...
