2018 defined standard Medicare Part D prescription drug plan coverage parameters
- Initial Deductible: will be increased by $5 to $405 in 2018.
- Initial Coverage Limit (ICL): will increase from $3,700 in 2017 to $3,750 in 2018.
- Out-of-Pocket Threshold (or TrOOP): will increase from $4,950 in 2017 to $5,000 in 2018.
What are Medicare Part D prescription drug quantity limits?
Your Medicare Part D plan formulary will show any Quantity Limits for your medications and you can also see the Quantity Limits for all formulary medications by using our Drug Finder ( www.Q1Rx.com ). For example: "Q:6/28Days" meaning the quantity limit is a quantity of 6 pills per 28 days or "Q:90/365Days" meaning the Medicare Part D plan limits this drug to 90 pills for the entire year.
What is the Medicare Part D initial coverage limit (ICL)?
The Initial Coverage Limit (ICL) is a fixed dollar amount ( $4,430 in 2022) that acts as the "boundary" between the second part of your Medicare Part D plan or the Initial Coverage Phase (where you and your drug plan share the cost of your drug purchases) and the third part of your plan, the Coverage Gap (where you receive a 75% Donut Hole discount on all formulary drugs).
What companies offer Medicare Part D?
Top 10 Supplemental Medicare Insurance Companies in 2022
- Mutual of Omaha – Best Overall
- Aetna – High-Quality Nationwide Options
- Cigna – Superior Customer Care
- United American – Best Enrollment Experience
- GPM – Superior Coverage Options
- UnitedHealthcare – Wide Variety of Plan Options
- Manhattan Life – Best Website Experience
- Bankers Fidelity – Best Senior Expertise
- Blue Cross Blue Shield – Best Mobile App
What are the best Medicare Part D plans?
They include:
- Switching to generics or other lower-cost drugs;
- Choosing a plan (Part D) that offers additional coverage in the gap (donut hole);
- Pharmaceutical Assistance Programs;
- State Pharmaceutical Assistance Programs;
- Applying for Extra Help; and
- Exploring national and community-based charitable programs.
What is the max out-of-pocket for Medicare Part D?
As expected, a $2,000 cap on out-of-pocket spending would generate larger savings than a $3,100 cap. Average out-of-pocket spending was $3,216 among the 1.2 million Part D enrollees with out-of-pocket spending above $2,000 in 2019.
What does Medicare Part D specifically cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan's list of covered drugs is called a “formulary,” and each plan has its own formulary.
What is not covered under Medicare Part D?
Drugs not covered under Medicare Part D Weight loss or weight gain drugs. Drugs for cosmetic purposes or hair growth. Fertility drugs. Drugs for sexual or erectile dysfunction.
What is quantity limits for Part D?
A quantity limit is a restriction used by Part D plans and Medicare Advantage Plans. It limits coverage of a drug to a certain amount over a certain period of time, such as 30 pills per month.
What are the 4 phases of Part D coverage?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
Is it worth getting Medicare Part D?
Most people will need Medicare Part D prescription drug coverage. Even if you're fortunate enough to be in good health now, you may need significant prescription drugs in the future. A relatively small Part D payment entitles you to outsized benefits once you need them, just like with a car or home insurance.
Do Part D plans have to cover all drugs?
Part D plans are required to cover all drugs in six so-called “protected” classes: immunosuppressants, antidepressants, antipsychotics, anticonvulsants, antiretrovirals, and antineoplastics.
Are OTC drugs covered by Part D?
This allows you to purchase select, eligible health and wellness items like allergy pills, cold and flu products, first aid supplies, vitamins and more. This is important because Original Medicare and Medicare Part D do not pay for OTC drugs.
What is best Part D drug plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
What are quantity limits?
A quantity limit is the highest amount of a prescription drug that can be given to you by your pharmacy in a period of time (for example, 30 tablets per month). Some drugs have quantity limits to help encourage appropriate usage, ensure effectiveness and reduce costs.
What is a quantity limit exception?
Information about this Request for Quantity Limit Exception Use this form to request coverage of a quantity in excess of plan quantity limits. Quantity limits are in place on certain classes of agents based on manufacturer's safety and dosing guidelines.
What is the opioid quantity limitation at retail and home delivery pharmacies for Medicare Part D patients?
Seven-day supply limit for opioid naïve patients This alert limits initial opioid fills for Part D patients who haven't filled an opioid prescription recently (like within the past 60 days) to a supply of 7 days or less. This alert shouldn't affect patients who already take opioids.
What is Medicare Part B and Part D?
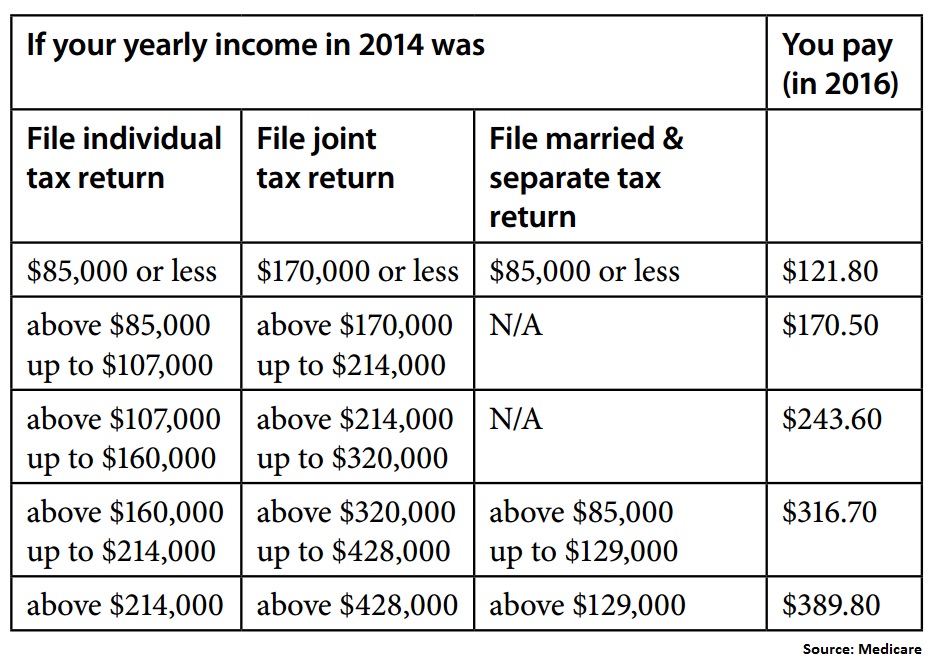
Medicare Part B (medical insurance) and Part D have income limits that can affect how much you pay for your monthly Part B and/or Part D premium. Higher income earners pay an additional amount, called an IRMAA, or the Income-Related Monthly Adjusted Amount.
What is the Medicare Advantage spending limit?
Medicare Advantage (Medicare Part C) plans, however, do feature an annual out-of-pocket spending limit for covered Medicare expenses. While each Medicare Advantage plan carrier is free to set their own out-of-pocket spending limit, by law it must be no greater than $7,550 in 2021. Some plans may set lower maximum out-of-pocket (MOOP) limits.
What is the Medicare donut hole?
Medicare Part D prescription drug plans feature a temporary coverage gap, or “ donut hole .”. During the Part D donut hole, your drug plan limits how much it will pay for your prescription drug costs. Once you and your plan combine to spend $4,130 on covered drugs in 2021, you will enter the donut hole. Once you enter the donut hole in 2021, you ...
How much is Medicare Part A deductible in 2021?
You are responsible for paying your Part A deductible, however. In 2021, the Medicare Part A deductible is $1,484 per benefit period. During days 61-90, you must pay a $371 per day coinsurance cost (in 2021) after you meet your Part A deductible.
What happens if you spend $6,550 out of pocket in 2021?
After you spend $6,550 out-of-pocket on covered drugs in 2021, you leave the donut hole coverage gap and enter the catastrophic coverage stage. Once you reach this stage, you only pay a small coinsurance or copayment for your covered drugs for the rest of the year.
What Medicare plans limit the number of providers you can visit?
Some private Medicare plans such as Medicare Advantage plans and Part D plans may feature provider or pharmacy networks that limit the providers you can visit for covered services.
What is Medicare Advantage Plan?
When you enroll in a Medicare Advantage plan, it replaces your Original Medicare coverage and offers the same benefits that you get from Medicare Part A and Part B.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
Why does Medicare change its drug list?
Your plan may change its drug list during the year because drug therapies change, new drugs are released, or new medical information becomes available.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
What are the tiers of Medicare?
Here's an example of a Medicare drug plan's tiers (your plan’s tiers may be different): Tier 1—lowest. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug.
How long does Medicaid pay for stay?
Or, a copy of a state document showing Medicaid paid for your stay for at least a month. A print-out from your state’s Medicaid system showing you lived in the institution for at least a month. A document from your state that shows you have Medicaid and are getting home- and community-based services.
What are some examples of documents you can send to Medicare?
Examples of documents you can send your plan include: A purple notice from Medicare that says you automatically qualify for Extra Help. A yellow or green automatic enrollment notice from Medicare. An Extra Help "Notice of Award" from Social Security. An orange notice from Medicare that says your copayment amount will change next year.
How much does a prescription cost for 2021?
Make sure you pay no more than the LIS drug coverage cost limit. In 2021, prescription costs are no more than $3.70 for each generic/$9.20 for each brand-name covered drug for those enrolled in the program. Contact Medicare so we can get confirmation that you qualify, if it's available.
What is an orange notice from Medicare?
An orange notice from Medicare that says your copayment amount will change next year. If you have. Supplemental Security Income (Ssi) A monthly benefit paid by Social Security to people with limited income and resources who are disabled, blind, or age 65 or older.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) cover inpatient hospital and outpatient health care services that are deemed medically necessary. " Medically necessary " can be defined as “services and supplies that are needed to prevent, diagnose, or treat illness, injury, disease, health conditions, ...
How long can you stay in a hospital with Medicare?
Medicare Part A covers hospital stays for any single illness or injury up to a benefit period of 90 days. If you need to stay in the hospital more than 90 days, you have the option of using your lifetime reserve days, of which the Medicare lifetime limit is 60 days.
How much does Medicare pay for therapy?
Starting in 2019, Medicare no longer limits how much it will pay for medically necessary therapy services. You will typically pay 20% of the Medicare-approved amount for your therapy services, once you have met your Part B deductible for the year.
How long does Medicare cover psychiatric care?
Medicare only covers 190 days of inpatient care in a psychiatric hospital throughout your lifetime. If you require more than the Medicare-approved stay length at a psychiatric hospital, there’s no lifetime limit for mental health treatment you receive as an inpatient at a general hospital.
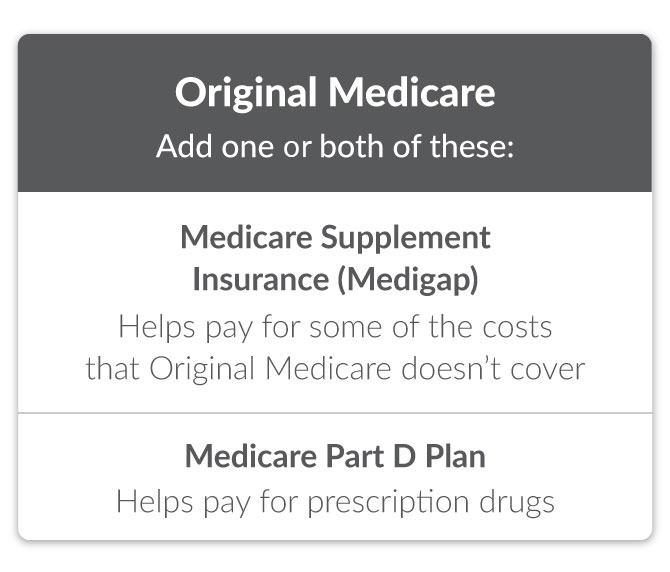
What is a Medigap policy?
Medicare Supplement Insurance (Medigap) policies are private health care plans designed to supplement your Original Medicare benefits and help pay for some of the out-of-pocket costs that Original Medicare doesn’t cover.
What are the services that are beyond the annual limit?
Extended hospitalization. Psychiatric hospital stays. Skilled nursing facility care. Therapy services. If you require any of these services beyond the annual limits, and don't qualify for an exception, you may be responsible for the full cost of those services for the rest of the year.
Does Medicare cover 100% of hospital costs?
Did you know there are some Original Medicare coverage limits? Medicare covers many of your hospital and medical care costs, but it doesn't cover 100% of them.
How long can you have opioids on Medicare?
First prescription fills for opioids. You may be limited to a 7-day supply or less if you haven’t recently taken opioids. Use of opioids and benzodiazepines at the same time.
Does Medicare cover acupuncture?
Talk with your doctor about other options that Medicare covers to treat your pain, like non-opioid medications and devices, physical therapy, acupuncture for lower back pain, individual and group therapy, behavioral health integration services, and more.
Does Medicare cover opioid pain?
There also may be other pain treatment options available that Medicare doesn’t cover. Tell your doctor if you have a history of depression, substance abuse, childhood trauma or other health and/or personal issues that could make opioid use more dangerous for you. Never take more opioids than prescribed.
Does Medicare cover benzodiazepines?
Some Medicare drug plans have a drug management program in place to help you use these opioids and benzodiazepines safely. If your opioid use could be unsafe (for example, due to getting opioid prescriptions from multiple doctors or pharmacies), or if you had a recent overdose from opioids, your plan will contact the doctors who prescribed them for you to make sure they’re medically necessary and you’re using them appropriately.
Does Medicare cover prescription drugs?
In most cases, the prescription drugs you get in a Hospital outpatient setting, like an emergency department or during observation services , aren't covered by Medicare Part B (Medical Insurance). These are sometimes called "self-administered drugs" that you would normally take on your own. Your Medicare drug plan may cover these drugs under certain circumstances.
Does Medicare require prior authorization?
Your Medicare drug plan may require prior authorization for certain drugs. . In most cases, you must first try a certain, less expensive drug on the plan’s. A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
Does Medicare send out safety alerts?
For certain drugs, Medicare drug plans might perform additional safety checks, and will send your pharmacy an alert for review before your prescription is filled. Safety alerts may cover situations like:
How much does Medicare Part D cost?
The average premium for Medicare Part D is around $40 a month. The premiums do vary by location and plan. Medications that fall on the higher tiers attract higher coinsurance costs and co-payments compared to those on the lower tiers.
How much is the deductible for Part D in 2021?
The initial deductible for Part D is $445 in 2021. In 2022, the initial deductible will be $480.
What is the Medicare donut hole?
The coverage gap is known as the donut hole. It begins once you reach your Medicare Part D costs plan’s initial coverage limit and ends when you spend a total of $6,550. Part D enrollees will receive a 75% discount on the total cost of their brand-name drugs purchased while in the donut hole. The 75% discount paid by the brand-name drug ...
What is Medicare Part D 2021?
Medicare Part D costs include the initial deductible, initial coverage limit, out-of-pocket threshold, and the coverage gap, also known as the donut hole.
How much discount do you get for a brand name drug?
The 75% discount paid by the brand-name drug manufacturer will apply to get out of the donut hole. For example: if you reach the donut hole and purchase a brand-name medication with a retail cost of $100, you will pay $25 for the medication, and receive $95 credit toward meeting your total out-of-pocket spending limit.
What are not covered prescriptions?
Not Covered Prescriptions: Drugs for cosmetic purposes. Medicines for anorexia, weight gain, or weight loss. Drugs meant to relieve colds and coughs. Medications for erectile dysfunction. Individual outpatient drugs. Over-the-counter medications. Minerals or vitamin drugs except those noted in the formulary.
What is the out of pocket limit for 2022?
In 2022, the out-of-pocket threshold is $7,050.
What is the Medicare Part D premium for 2021?
Part D plans have their own separate premiums. The national base beneficiary premium amount for Medicare Part D in 2021 is $33.06, but costs vary. Your Part D Premium will depend on the plan you choose.
What is Medicare Part B?
Medicare Part B. This is medical insurance and covers visits to doctors and specialists, as well as ambulance rides, vaccines, medical supplies, and other necessities.
What about Medicare Advantage plans?
The price for Medicare Advantage (Part C) plans greatly varies. Depending on your location, you may have dozens of options, all with different premium amounts. Because Part C plans don’t have a standard plan amount, there are no set income brackets for higher prices.
What about Medicaid?
If you qualify for Medicaid, your costs will be covered. You won’t be responsible for premiums or other plan costs.
How much is Medicare Part B 2021?
For Part B coverage, you’ll pay a premium each year. Most people will pay the standard premium amount. In 2021, the standard premium is $148.50. However, if you make more than the preset income limits, you’ll pay more for your premium.
How many types of Medicare savings programs are there?
Medicare savings programs. There are four types of Medicare savings programs, which are discussed in more detail in the following sections. As of November 9, 2020, Medicare has not announced the new income and resource thresholds to qualify for the following Medicare savings programs.
What age does QDWI pay Medicare?
The QDWI program helps pay the Medicare Part A premium for certain individuals under age 65 who don’t qualify for premium-free Part A.