Does Medicare cover 90834?
Medicare 2021 90834 Reimbursement Rate: $103.28. Medicare 2020 90834 Reimbursement Rate: $94.55. There has been a 9.2% increase in reimbursement from 2020 to 2021. Billing 90834 vs 90837. This is straightforward enough. Pick the duration of time the session occurred within and use the corresponding code.
What does 90834 stand for?
The Current Procedural Terminology (CPT ®) code 90834 as maintained by American Medical Association, is a medical procedural code under the range - Psychotherapy Services and Procedures. Subscribe to Codify and get the code details in a flash. Request a Demo 14 Day Free Trial Buy Now
What is Procedure Code 90834?
- Licensed Clinical Social Workers (LCSW)
- Licensed Professional Counselors (LPC)
- Licensed Marriage Family Therapist (LMFT)
- Clinical Psychologists (PsyD or PhD)
- Psychiatrists (MD)
How does Medicare calculate reimbursement?
To see payment rates in your area:
- Select the year
- Select Pricing Information
- Choose your HCPCS (CPT code) criteria (single code, range of codes)
- Select Specific Locality or Specific Medicare Administrative Contractor (MAC)
- Enter the CPT code (s) you are looking for
- Under "Modifier" select All Modifiers
- Select your Locality (please note that they are not in alphabetical order)
- Results:
What factors affect insurance reimbursement rate for psychotherapy?
Do insurance companies release contracted rate information?
Does insurance pay for mental health therapists?
Does Medicare cover mental health?
What modifier should be used with 90834?
95The new CPT modifier for “synchronous telemedicine” services is “95” and it indicates “synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system.” As a coding example, when 45 minutes of psychotherapy is delivered via telemedicine, append the CPT code 90834 with ...
How Much Does Medicare pay for 90837?
$132.69What is the difference between the “facility rate” and “nonfacility rate” for telehealth services?CodeService2021 Facility Rate90832Psychotherapy 30-minutes$68.7490837Psychotherapy 60-minutes$132.6996132Neuropsych Test Eval$106.0896158Hlth Bhvr Intrv Indvl$58.971 more row•Dec 10, 2021
How many minutes is a 90834 session?
CPT® code 90834: Psychotherapy, 45 minutes.
Who can Bill 90834 CPT code?
As defined by the CPT, 90834 should be used when you spend an estimated 38–52 minutes on therapy with the client, and 90837 is for all therapy sessions that are at least 53 minutes long.
What is the Medicare approved amount for psychotherapy?
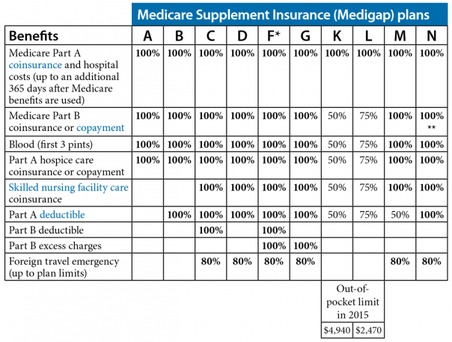
Mental health services, such as individual counseling provided in an outpatient setting will be covered at 80% of the approved charge with Medicare Part B after the annual deductible ($233 for 2022) is met. You pay the other 20%.
How do I calculate Medicare reimbursement for CPT codes?
You can search the MPFS on the federal Medicare website to find out the Medicare reimbursement rate for specific services, treatments or devices. Simply enter the HCPCS code and click “Search fees” to view Medicare's reimbursement rate for the given service or item.
Is 90834 a diagnosis code?
Key facts for utilizing psychotherapy codesPsychotherapy CodesCPT® CodeDescriptor90834Psychotherapy, 45 minutes with patient90837Psychotherapy, 60 minutes with patient90845Psychoanalysis5 more rows
Can you bill two therapy sessions on the same day?
Billing requires the use of multiple CPT codes for the same session, each code having its own charge chosen by the therapist. Thus, multiple lines for the same date of service will be used on the claim form or statement.
How do you bill for a 90 minute psychotherapy session?
Units vs Extended Session CPT Codes To bill an insurance claim for a 90 minute individual therapy session: bill 90837. with add-on code 99354.
Does Medicare pay for cognitive behavioral therapy?
Cognitive Behavioral Therapy (CBT) as psychotherapy via telemental health is covered by Medicare for certain eligible beneficiaries.
What is the CPT code for 50 minute psychotherapy session?
90834Therapists who conduct a traditional 50-minute therapy session should be aware that these should generally be billed as a 90834, as less than 53 minutes are spent in clinical discussion and therapy.
What are the new CPT codes for mental health 2021?
There are many CPT codes currently used by mental health professional that can be reported under the following categories:Health Behavior Assessment and Intervention (CPT codes 96156-96171)Psychotherapy Codes (CPT codes 90832-90863)Psychological and Neuropsychological Testing Codes (CPT codes 96105-96146)
OUTPATIENT PSYCHIATRY & PSYCHOLOGY SERVICES FACT SHEET
Psychotherapy Psychiatric Therapeutic Procedures (CPT Codes 90832-90838, 90845-90853, 90865): A. Codes 90832-90834 represent insight oriented, behavior modifying, supportive,
Billing and Coding Guidelines Psychiatry and Psychology Services
D. CPT Code 90853 should also not be billed more than once per day for the same beneficiary unless he/she has participated in a separate and distinct group therapy session.
Billing and Coding: Psychiatry and Psychology Services
Use this page to view details for the Local Coverage Article for billing and coding: psychiatry and psychology services.
Fee Schedules - General Information | CMS
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
What factors affect insurance reimbursement rate for psychotherapy?
Factors that effect your insurance reimbursement rate for psychotherapy: Location, paying more for under-served locales and less for over-served locations. License, education, and specialization. Specialization. Consumer demand at the time of signing your contract.
Do insurance companies release contracted rate information?
Insurance companies are completely unwilling to release their contracted rate information for reason we’ll discuss shortly and as a result, you don’t know how much you’ll be reimbursed for providing psychotherapy and other mental health services.
Does insurance pay for mental health therapists?
In summary, some private insurance companies reimburse mental health therapists for far more than others. A great way to quickly learn which companies pay the most is to simply ask your colleagues about their experiences with different reimbursement rates for private insurance companies.
Does Medicare cover mental health?
Medicare doesn’t cover all licenses and is far more selective than Medicaid about which providers they will allow into their network. As a result, mental health reimbursement rates for Medicare are higher than Medicaid rates by a substantial margin.
Is Blue Cross Blue Shield the highest reimbursing plan?
To sum things up, the Blue Cross and Blue Shield network across the United States is one of the highest reimbursing and most competitive plans to work with. Inquire about your local BCBS within google by typing in “Blue Cross Blue Shield” + your state’s name.
Does Medicaid pay poorly?
Sadly, Medicaid pays poorly and is overly complex, often requiring license-level modifiers and taxonomy codes. The reason I would recommend working with Medicaid is to establish a very busy practice (perhaps with a billing team on your side) and/or because you want to serve this population of folks in need.
Is Medicaid subcontracted?
Many Medicaid polices are subcontracted out to lower paying organizations. This can skew data downward in comparison to brands that to not facilitate a Medicaid plan in that State. Likewise, EAP sessions have far more hoops, billing nuance, and prior-to-session manual labor (authorizations) involved in billing.
What is CPT code 90837?
• Code 90837: Psychotherapy, 60 minutes with patient and/or family member In general, providers should select the code that most closely matches the actual time spentperforming psychotherapy . CPT® provides flexibility by identifying time ranges that may be associated with each of the three codes:
Is a psychotherapy code dependent on the location?
Psychotherapy codes are no longer dependent on the service location (i.e., office, hospital, residential setting, or other location is not a factor). However, effective January 1, 2014, when E&M services are paid under Medicare’s Partial Hospitalization Program (PHP) and not in the physician office setting, the CPT outpatient visit codes ...
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L33252 Psychiatric Diagnostic Evaluation and Psychotherapy Services.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
How much more does 90837 cost than 90834?
Due to the extended length, 90837 does indeed pay more than 90834. Depending on your credentials, we’ve found that 90837 can pay between $9-20 more on average than a 90834 appointment. This amounts to typically ~13-20% more per session. Medicare has published their 60 minute individual therapy reimbursement rates.
What is CPT code 90837?
CPT Code 90837 is a procedure code that describes a 60 minute individual psychotherapy session performed by a licensed mental health provider. 90837 is considered a routine outpatient CPT Code and is one of the most common CPT codes used in mental health insurance claims coding and billing. We’ll teach you the ins and outs ...
What is the add on code for CPT?
Add-on CPT Code 99354 is defined as a prolonged services code and is defined as an extra 30-74 minutes of therapy. 99354 used to only be allowed by Medical Doctor’s, but has since expanded and is applicable to 90837 and 90487.
How long is 90837?
90837 is defined as a session of 60 minutes, ranging from 53 minutes to longer. The only difference between 90834 (the other commonly used CPT code) and 90837 is the time. 90837 is 60 minutes and 90834 is 45 minutes. Not every therapist does sessions at these exact time intervals.
Does United Healthcare cover 90387?
Still, the vast majority of insurance companies consider 90387 to be routine and will cover it as they would other mental health procedure codes. Thankfully, United Healthcare has reversed course and as of 2019 has started accepting 90837 without prior authorization.
Is a 90837 preauthorization required?
Typically no, authorization is not required. Up until very recently one of the largest insurers, United Healthcare required authorization for 90837. The pre-authorization requirement was not extended onto the other frequently used procedure codes, 90791 or 90834.
What factors affect insurance reimbursement rate for psychotherapy?
Factors that effect your insurance reimbursement rate for psychotherapy: Location, paying more for under-served locales and less for over-served locations. License, education, and specialization. Specialization. Consumer demand at the time of signing your contract.
Do insurance companies release contracted rate information?
Insurance companies are completely unwilling to release their contracted rate information for reason we’ll discuss shortly and as a result, you don’t know how much you’ll be reimbursed for providing psychotherapy and other mental health services.
Does insurance pay for mental health therapists?
In summary, some private insurance companies reimburse mental health therapists for far more than others. A great way to quickly learn which companies pay the most is to simply ask your colleagues about their experiences with different reimbursement rates for private insurance companies.
Does Medicare cover mental health?
Medicare doesn’t cover all licenses and is far more selective than Medicaid about which providers they will allow into their network. As a result, mental health reimbursement rates for Medicare are higher than Medicaid rates by a substantial margin.