
If you are treated in a private hospital, Medicare will pay 75% of the public rate for the treatment, the anaesthesia and all diagnostic work. You and your health insurer are responsible for the rest, including 100% of the cost of all fees like accommodation fees, doctor's fees and theatre fees. Outpatient Clinics
Full Answer
How much does Medicare pay for treatment?
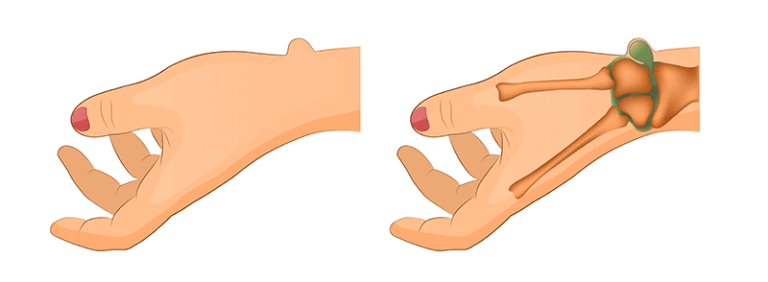
Oct 01, 2019 · This section prohibits Medicare payment for any claim which lacks the necessary information to process the claim. CMS Manual System, Pub. 100-03, Medicare National Coverage ... ASPIRATION AND/OR INJECTION OF GANGLION CYST(S) ANY LOCATION 26341 MANIPULATION, PALMAR FASCIAL CORD (IE, DUPUYTREN'S CORD), POST ENZYME …
Does Medicare pay for surgery in private hospitals?
Medicare coverage for many tests, items, and services depends on where you live. This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live. Your Medicare coverage choices. Learn about the 2 main ways to get your Medicare coverage — Original Medicare or a Medicare Advantage Plan ...
Does Medicare cover nail fungus treatment?
Jan 10, 2014 · 0. Jan 10, 2014. #1. I was wondering if someone has been successful in getting Medicare to pay for a sebaceous cyst excision with pain being the main factor. Often, it is just irritating to the patient, rubbs against clothing, etc. I have only been able to get them paid if infection was involved. Appeals for pain have not been successful.
Does Medicare cover jaw surgery?
Aug 01, 2019 · If you have Original Medicare, jaw surgery will be covered like most other surgical procedures at 80%, leaving the patient to cover the remaining 20% of the cost. If you have purchased a Medigap supplemental insurance, it may help pay for some of …
Does Medicare cover elective surgery?
What Does Medicare Cover? Medicare covers many expenses related to essential surgical procedures, but it does not cover elective surgeries (such as cosmetic surgeries) unless they serve a medical purpose.
How Much Does Medicare pay for surgery?
Typically, you pay 20% of the Medicare-approved amount for your surgery, plus 20% of the cost for your doctor's services.
Does Medicare cover hysteroscopy?
Medicare typically covers medically-necessary hysterectomies. Medicare Advantage plans also cover hysterectomies and include an annual out-of-pocket spending limit, which Original Medicare doesn't offer. Medicare typically does cover hysterectomies that are deemed medically necessary by a doctor.
How do you find out if Medicare will cover a procedure?
If you belong to a Medicare health plan, contact the plan for more information. Call the hospital or facility and ask them to tell you the copayment for the specific surgery or procedure the doctor is planning. It's important to remember that if you need other unexpected services, your costs may be higher.
What surgeries are not covered by Medicare?
Medicare does not cover: medical and hospital services which are not clinically necessary, or surgery solely for cosmetic reasons; ambulance services; and. emergency department administration or facility fees.
What is the maximum out-of-pocket expense with Medicare?
Medicare: Medicare's Private Plans.” In the traditional Medicare program, there's no annual dollar limit on your out-of-pocket expenses.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Does Medicare cover sebaceous cyst removal?
Cryotherapy for acne, or the destruction of milia, is considered cosmetic and is not covered. The removal of skin tags or sebaceous cysts is considered cosmetic unless medical necessity as outlined above exist and is properly documented in the patient's medical record.Jan 7, 2016
How long does it take for Medicare to approve a procedure?
Medicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
What is not covered under Medicare Part A?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
Is Blue Shield part of Medicare?
Blue Shield of California is an HMO and PDP plan with a Medicare contract. Enrollment in Blue Shield of California depends on contract renewal.
Does Medicare pay 100 percent of hospital bills?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
Why do you need jaw surgery?
Jaw surgery may be required to correct facial and structural deformities that impact speech, chewing and even breathing. Beyond that, jaw surgery may be required when teeth become impacted or when facial trauma has caused fractures or breaks.
Does Medicare have a Part A and B plan?
Many Medicare recipients choose to get their Part A and Part B benefits through a Medicare Advantage plan. Medicare Advantage plans are required to provide at least the same Part A and Part B coverage as Original Medicare, but many offer additional benefits, as well. Related articles:
Does Medicare cover jaw surgery?
Because jaw surgery is so vital to oral and overall health, it often requires the skills and advanced equipment of a specialized surgeon. This also means that these procedures can be costly, leaving many patients, especially those on Medicare, to wonder about paying for surgery.
How to find out if a prescription drug covers nail fungus?
To find out if your prescription drug plan covers nail fungus medication, check the plan’s formulary, or list of covered medications. The formulary may change at any time, but the plan will inform you when necessary. Medicare Part D prescription drug plans do not usually cover over-the-counter medications such as over-the-counter nail fungus creams ...
What is Medicare Advantage?
Medicare Advantage must cover everything that Original Medicare covers, with the exception of hospice care which is still covered by Medicare Part A.
What does nail fungus mean?
Nail fungus results in nails that are thickened, discolored, brittle and ragged, and slightly foul smelling. Nail fungus can affect the fingernails, but it’s more common in the toenails. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area.
Does Medicare cover foot care?
In other people, nail fungus could be a mild condition causing no problem beyond the cosmetic. Medicare does not generally cover routine foot care, including removal of corns and calluses or trimming of toe nails.
Can nail fungus come back?
What is nail fungus treatment? According to the Mayo Clinic, nail fungus can be difficult to treat and even after successful treatment nail fungus often comes back.
Can you remove fungus from your nail?
In some cases, your doctor may recommend surgery as nail fungus treatment. Surgery could temporarily remove the nail so antifungal medication can be applied directly under the nail. Surgery also might involve permanent nail removal if the infection is severe.
Does Medicare cover nail fungus?
Medicare covers limited podiatry. Medicare may cover nail fungus treatment if it’s determined to be medically necessary foot care. According to the Mayo Clinic, nail fungus may lead to a serious infection that spreads beyond your feet if you have a suppressed immune system.
What is the coinsurance for dermatology?
A person usually also pays Part B coinsurance, which is 20% of the Medicare-approved amount for dermatological services. If the healthcare professional involved does not agree to Medicare’s rates, the out-of-pocket cost may be higher.
How long does Medicare Part B cover?
Medicare Part B covers one full-body exam within the first 12 months of coverage. A doctor gives this exam to prevent future health problems. Some Advantage plans may cover the costs of preventive screenings and services.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
Does Medicare cover dermatology?
Summary. Medicare may cover medically necessary dermatology services, such as the remo val or treatment of cancerous skin lesions. When Medicare covers dermatology services, Part B usually provides the coverage. In this article, we detail which dermatology services Medicare typically covers and which it excludes.
Does Medicare cover a full body exam?
Medicare covers most costs relating to skin cancer and other skin conditions, such as psoriasis, rosacea, and eczema. Medicare does not cover most preventive full-body exams or cosmetic treatments.
Does Medicare cover mole removal?
However, there can be exceptions, depending on a person’s plan and their skin condition. In addition, Medicare does not usually cover mole removal for cosmetic reasons.
Does Medicare cover skin biopsy?
Skin cancer. If a doctor deems it necessary, Medicare Part B typically covers a skin biopsy to check for cancerous tissue. If a doctor finds cancer, Medicare covers the treatment, though a person is still responsible for deductibles and coinsurance costs. In 2018, researchers. Trusted Source.
How much does Medicare pay for outpatient care?
If the cost is higher than the public rate, you will be responsible for the difference. In an outpatient setting. Medicare will pay 85% of the public rate and you will be responsible for the rest.
What percentage of Medicare costs are covered by private health insurance?
Medicare pays 75% of the Medical Benefits Scheme (MBS) costs and private health insurance pays the remaining 25%. Treatment as a private patient in a private hospital. Private health insurance covers some or all of the costs for accommodation, theatre fees and specialist fees. Advantages of private health cover over Medicare include the choice ...
What are the advantages of private health insurance over Medicare?
Advantages of private health cover over Medicare include the choice of your own treating doctor and eligibility for a shared or private room. Another advantage is shorter waiting times for elective (non-essential) surgery.
How long do you have to live in Australia to qualify for Medicare?
You must have lived or intend to live in Australia for more than 6 months to be eligible. An Australian permanent resident. If you have applied for your PR, or are disputing your PR, you are eligible for Medicare. Reciprocal Health Care Agreement.
Does Medicare cover ambulance rides?
While Medicare covers a lot, there are a few things it won't cover and it's good to know what these are before going into treatment. Here's what Medicare will not cover under most circumstances: Ambulance rides. Overseas medical and hospital costs. Medical treatments that aren't medically necessary, like facelifts.
Does Medicare cover dental care?
Under very few circumstances, Medicare will cover dental treatment. This includes emergency room visits where you're treated for pain, dental work that is necessary to continue with another Medicare-covered surgery and dental work for certain low-income children. Medication.
Does Medicare pay for outpatient services?
Medicare will pay 85% of the public rate and you will be responsible for the rest. Private health insurance usually doesn't cover outpatient services. If you see a GP. Medicare will pay 100% of the cost if the GP bulk bills.
Do you need pelvic exams after age 65?
Gynecologists recommend that women over the age of 65 continue to get pelvic exams. Even after the age of 65, women are still at risk of developing cervical or vaginal cancer. No matter what age, women should get a pelvic exam until their doctor says it’s no longer necessary.
How often does Medicare pay for gynecological exams?
For typical patients, Medicare will cover a pelvic and breast exam every 24 months. However, you may be eligible for an exam every 12 months if:
How much does a gynecological exam cost with Medicare?
Medicare encourages people to embrace preventative care. After all, the more preventative care you receive, the less likely you are to end up needing expensive emergency care.
