Medicare Part B pays for 80 percent of the cost of your CPAP mask and other related supplies, as well as for the rental cost of the machine. That leaves you to pay 20 percent of your CPAP rentals and purchases.
Full Answer
Does Medicare pay for CPAP machines and supplies?
CPAP machines, oxygen, oxygen tubing, diabetic testing supplies and much more. DME products must be reusable. When covered by Medicare Part B your deductible applies, then Medicare pays 80% and you or your secondary insurance would pay 20%. If you have a ...
How to find Medicare approved CPAP suppliers?
- Medicare requires all new CPAP therapy patients to use their newly acquired CPAP machine for at least 4 hours a night.
- This is called the "compliance period."
- Failure to pass the compliance period will result in Medicare not paying for your new machine.
How often will Medicare pay for a CPAP machine?
To qualify for CPAP coverage, you must meet the following requirements:
- Complete a sleep test in a laboratory setting or by using an approved at-home test
- Be diagnosed with obstructive sleep apnea based on sleep test results
- Have a prescription for a CPAP machine from your doctor
- Get the CPAP machine from a participating Medicare supplier
Will Medicare pay for CPAP?
Medicare will pay 80 percent of the cost of CPAP machines and certain supplies. Some accessories such as tubing or face masks might not be fully covered. You’d still be responsible for 20 percent of any remaining costs that are not covered by Medicare. Additionally, if the services are not Medicare-approved, you may need to pay more out of pocket.

Does Medicare pay for supplies for CPAP?
Medicare typically pays 80 percent of approved costs for CPAP machines and BiPAP machines. Certain supplies, such as tubing and masks, are also partially covered. You may need to undergo a doctor-supervised sleep study to qualify for a CPAP machine covered by Medicare.
How Long Will Medicare pay for CPAP supplies?
for 13 monthsfor the machine rental and purchase of related supplies (like masks and tubing). Medicare pays the supplier to rent a CPAP machine for 13 months if you've been using it without interruption. After Medicare makes rental payments for 13 continuous months, you'll own the machine.
Does Medicare cover CPAP machine parts?
Medicare will cover a part of the cost of a CPAP machine if you've been diagnosed with obstructive sleep apnea. Coverage for CPAP machines falls under the Medicare Part B coverage of durable medical equipment.
How much do CPAP supplies cost out of pocket?
How Much Does a CPAP Machine Cost?Machine TypeCost RangeCPAP (Continuous Positive Airway Pressure)$250 to $1,000BiPAP (Bilevel Positive Airway Pressure)$1,000 to $6,000Auto CPAP or APAP (Automatic Positive Airway Pressure)$450 to $1,800Mar 11, 2022
How often can you get CPAP supplies under Medicare?
CPAP Mask - 1 every 3 months. CPAP Tubing - 1 every 3 months. CPAP Headgear - 1 every 6 months.
How often can you get a new CPAP machine under Medicare?
Your CPAP machine should be replaced after approximately 5 years of use. The good news is, Medicare and most other insurers typically provide coverage for a new CPAP machine around the same time frame.
Does ResMed accept Medicare?
Do you accept either Medicare or Medicaid? Medicare and Medicaid will pay for medical equipment and supplies only if a supplier has a Medicare or Medicaid supplier number. Expedite, LLC, the operator of the ResMed Shop, does not have a Medicare or Medicaid supplier number.
How many hours per night should I use my CPAP machine?
If you're wondering, “how many hours per night should CPAP be used?” the answer is, for the entire night while you sleep, ideally 7+ hours. CPAP compliance measures how many hours and nights you use your therapy and if you use it often enough for effective treatment.
Will Medicare replace my recalled CPAP machine?
If the equipment is more than 5 years old, Medicare will help pay for a replacement. Important: Register your recalled equipment with Philips so they know you need a replacement, and can provide information on the next steps for a permanent corrective solution.
Do I own my CPAP machine?
After the rental period is over, you own the device. However, these insurance companies are often requiring proof that you are using the equipment and meeting their usage requirements (at least 4 hours per night for 70% of nights) in order to continue payment.
How much do CPAP supplies cost per month?
CPAP Mask - $40 to $200 every 3 months. Headgear - $30 to $50 every 6 months. Tubing - $10 to $35 ($40 to $60 for heated hoses) every 3 months.
How much does ResMed CPAP cost?
The ResMed AirSense 10 AutoSet CPAP machine comes with a 2-year warranty and costs $969.
Does Medicare Cover CPAP and Other Pap Therapy For Sleep Apnea?
Yes. Medicare covers a 3-month trial of for CPAP therapy (learn more about CPAP here) if you’ve been diagnosed wtih obstructive sleep apnea (learn...
How Does Medicare Define CPAP Compliance Or Adherence?
Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (that’s 21 nights) during a consecutive 30 day period...
What Is The Rental Term For Pap Therapy?
If the 3-month trial is successful (see above) Medicare will continue to cover the PAP device on a rental basis for up to 13 months in total up to...
Will Medicare Cover CPAP If I had A Machine Before I Got Medicare?
Yes, Medicare may cover rental or a replacement CPAP machine and/or CPAP supplies if you meet certain requirements.
When Does Medicare Cover Bi-Level Or Bipap?
Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive...
What Is Required in The Initial Face-To-Face Clinical Evaluation?
Written entries of the evaluation may include:History 1. Signs and symptoms of sleep disordered breathing including snoring, daytime sleepiness, ob...
What Information Does Medicare Require on The Prescription For CPAP and Supplies?
1. Beneficiary/patient’s name 2. Treating physician’s name 3. Date of order 4. Detailed description of items (type of device and supplies, pressure...
How Often Does Medicare Cover Replacement Pap Supplies?
Here’s an outline of the Medicare supply replacement schedule. For more detail (including how to tell when your equipment needs to be replaced, che...
How Much Will Medicare Pay For A CPAP Or Other Pap Machine?
Medicare will pay 80% of the Medicare-approved amount for a PAP device after you’ve met your Part B deductible (learn about this and other insuranc...
CPAP therapy comes with continuing expenses
CPAP therapy requires periodic purchase of replacement supplies, including masks, filters, headgear, the water reservoir in the humidifier and the tubing that connects the CPAP machine with your face mask. Medicare covers these supplies on varying schedules; a competent supplier will help you optimize the timing of these purchases.
What you pay for CPAP
Because CPAP is covered as durable medical equipment, the Medicare Part B deductible applies; it’s $233 in 2022. Then you pay 20% of the Medicare-approved amount for the CPAP machine rental and ongoing supply purchases.
How long does it take to use CPAP for Medicare?
How does Medicare define CPAP compliance or adherence? Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (that’s 21 nights) during a consecutive 30 day period any time in the first three months of initial usage.
How much does Medicare pay for a PAP?
Medicare will pay 80% of the Medicare-approved amount for a PAP device after you’ve met your Part B deductible (learn about this and other insurance terms here ). If you have a secondary insurance, they may pick up the remaining 20% (read our post about how much sleep studies cost here ).
How long does a bi level CPAP trial last?
If the patient switches to a bi-level device within the 3-month trial, the length of the trial is not changed as long as there are at least 30 days remaining. If less than 30 days remain of the trial period, re-evaluation must occur before the 120th day (following the same criteria as CPAP adherence).
When does Medicare continue to cover PAP?
If you are successful with the 3-month trial of PAP, Medicare may continue coverage if the following criteria are met: Clinical re-evaluation between the 31st and 91st day after starting therapy, to include: Treating physician documents that the patient is benefiting from therapy; and.
Does Medicare cover bi level respiratory assist?
Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive sleep apnea if the patient meets the criteria for PAP therapy (outlined above) and:
Does Medicare require proof of usage?
Many other insurance companies are now following Medicare’s lead and requiring proof of usage before continuing to pay for the machine. Learn more about that here. If adherence to therapy is not documented within the first three months, the patient fails the trial period.
Does Medicare cover CPAP?
Yes. Medicare covers a 3-month trial of for CPAP therapy (learn more about CPAP here) if you’ve been diagnosed wtih obstructive sleep apnea (learn more about OSA here) and meet one of the following criteria: AHI or RDI > 15 events per hour with a minimum of 30 events or. AHI or RDI > 5 to14 events per hour with a minimum ...
Medicare Coverage for CPAP Machines
Caitlin McCormack Wrights has over a decade of experience writing hundreds of articles on all things finance. She specializes in insurance, mortgages, and investing and relishes making dull subject matter gripping and everyday topics amazing. Caitlin has a bachelor's from Duke and a master's from Princeton.
When Will Medicare Cover CPAP Machines?
Medicare Part B covers the use of CPAP machines by adult patients with obstructive sleep apnea. Medicare initially will cover the cost of the CPAP for up to three months if your sleep apnea diagnosis is documented by a sleep study.
How To Get Medicare To Cover a CPAP Machine
Medicare will cover a CPAP machine if you meet two conditions. You must first be diagnosed with obstructive sleep apnea, and you must submit your primary doctor’s order or prescription to the right supplier to receive coverage. Here are the steps you’ll need to take to make that happen.
How Much Does a CPAP Machine Cost With Medicare?
Medicare typically covers the most basic level of equipment, and it may not pay for upgrades. In the case where Medicare doesn’t cover upgrades or extra features, you’ll need to sign an Advance Beneficiary Notice (ABN) before you get the equipment.
The Bottom Line
The rules of how DMEs are covered, including CPAP machines, are generally the same whether you have Original Medicare or a Medicare Advantage Plan. However, the amount you pay with Original Medicare and a Medicare Advantage Plan may often differ. Compare Medicare and Medicare Advantage to learn more.
How often can I get a new CPAP machine while on Medicare?
Once you’ve continuously used your CPAP machine for the approved 13-month rental, you will own it. However, CPAP supplies may lose effectiveness with use, and Medicare covers their replacement. Guidelines suggest replacing a CPAP mask every three months and a non-disposable filter every six months. 4
How do I get CPAP supplies covered by Medicare?
Medicare will only help cover CPAP supplies and accessories if you get them from a Medicare-approved contract supplier after completing the necessary medical steps.
Get A Second Clinical Evaluation
If Medicare covers your CPAP machine for the three-month trial period, you must undergo a second clinical evaluation to establish medical necessity for continued coverage. During the face-to-face evaluation, your doctor must document that your symptoms of sleep apnea have improved and that youve adhered to consistent CPAP therapy.
Does Medicare Pay For Cpap Machines And Supplies
Many or all of the products featured here are from our partners who compensate us. This may influence which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here’s how we make money.
How Do You Treat Sleep Apnea
Mild cases of sleep apnea are often managed through simple lifestyle changes such as quitting smoking, losing weight or treating nasal allergies. For individuals who have a moderate or severe case of sleep apnea, treatment may be more complex, and can include supplemental oxygen, oral appliances or airway-pressure devices, including CPAP machines.
What Are Medicare Guidelines For Cpap
You have a three-month trial period covered by Medicare. After three months, your doctor will check how the treatment is working for you. Medicare may cover CPAP therapy long-term if your doctor verifies in your medical record that:
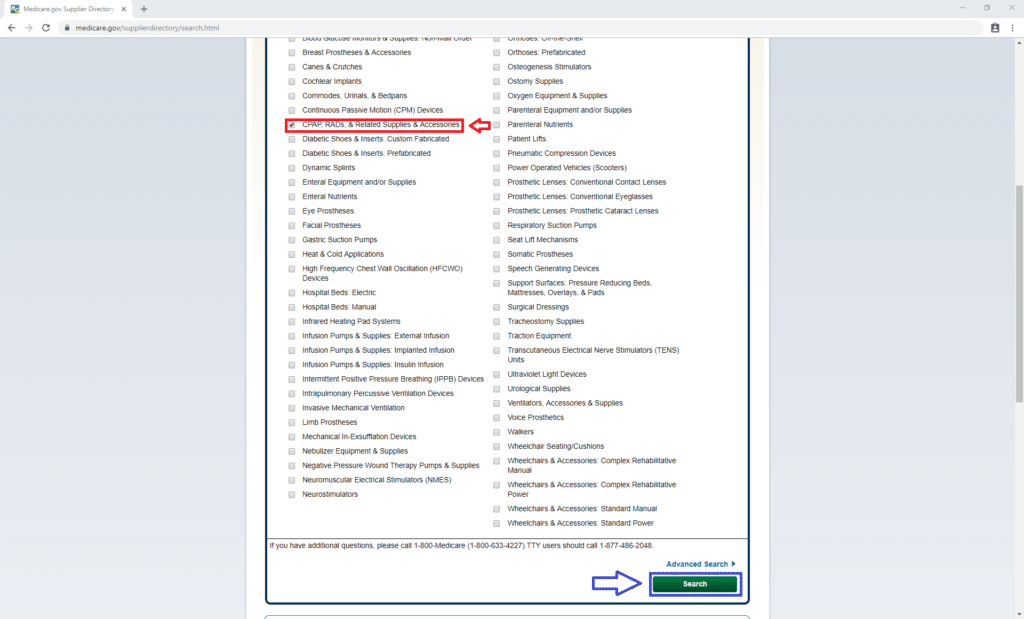
Option : Use Medicares Website
If you have a Medicarehealthcare plan, you can also find in-network durable medical equipment providers by using Medicares Supplier Directory. After you click the link, enter your zipcode and select the corresponding product category. For CPAP machines and related supplies, select .
When Should I Contact My Private Insurance
Once you think you have sleep apnea, check with your insurance company to find out what type of coverage you get for CPAP.
Insurance And Cpap Machines
The terms of your CPAP machine, insurance coverage depends on your provider. Some providers reimburse you for the cost of purchasing the machine outright, while others require a rent-to-own plan under which you must use the machine for a set amount of time before it becomes your property.
How often does Medicare pay for CPAP?
nondisposable filters: 2 times per year. chinstrap: 2 times per year.
How long can you rent a CPAP machine?
CPAP rental for 13 months if you’ve been using it consistently (after 13 months , you’ll own the CPAP machine) masks or nose pieces you wear when using the machine. tubing to connect the mask or nose piece to the machine. This Medicare coverage applies only if your doctor and supplier participate in the Medicare program.
What is Medicare Part B?
Medicare Part B is the section that pays for durable medical equipment (DME), such as CPAP machines. To have your CPAP machine covered, you need to make sure that your clinician and device supplier participate in the Medicare program.
How long does a CPAP machine last?
Your CPAP machine is paid for after 13 months and you’ll own it, but it should last several years . You may have it replaced with your medical benefit after this time.
Does Medicare cover CPAP machines?
Medicare will cover a part of the cost of a CPAP machine if you’ve been diagnosed with obstructive sleep apnea. Coverage for CPAP machines falls under the Medicare Part B coverage of durable medical equipment. You’ll still pay a portion of the cost for your CPAP machine, unless you have a Medigap plan to cover those costs.
Do you pay for a CPAP machine?
You’ll still pay a portion of the cost for your CPAP machine, unless you have a Medigap plan to cover those costs. A continuous positive airway pressure (CPAP) machine is a medical device that gives you extra oxygen with a bit of force.
How much does Medicare cover for a CPAP machine?
After you pay the $185 yearly Part B deductible (for 2019), Medicare will cover 80% of the Medicare-approved rental costs of the CPAP machine for 3 months, ...
How long is a CPAP trial?
If you have been formally diagnosed with sleep apnea, you are likely eligible for a 3-month trial of CPAP therapy. If the therapy is successful, your doctor can extend the treatment and Medicare will cover it.
What is the best treatment for sleep apnea?
A continuous positive airway pressure (CPAP) machine is the most common treatment for moderate to severe sleep apnea. The machine is equipped with a mask that blows air into your throat while you are sleeping to keep your airway ...
Does Medicare Supplement have a 20% deductible?
Depending on the Medicare Supplement insurance plan you choose, you could get full coverage for both the Part B deductible and the 20% Part B coinsurance cost. You can use the comparison chart below to see the benefits that are offered by each type of standardized Medigap plan sold in most states.
Can you take a prescription for a CPAP machine?
After you are approved for therapy, your doctor will give you a medical prescription for the CPAP machine. You can take this to any medical equipment supplier that accepts Medicare payments. If they accept Medicare, the supplier will bill Medicare directly for your Medicare-covered CPAP supplies.
Does Medicare cover CPAP?
Medicare does cover CPAP machine therapy if you are diagnosed with sleep apnea. You may be eligible for sleep apnea treatment options if you are enrolled in Medicare Part B and have been diagnosed with obstructive sleep apnea. If you have been formally diagnosed with sleep apnea, you are likely eligible for a 3-month trial of CPAP therapy.
How long does Medicare pay for a CPAP machine?
The Part B deductible applies. Medicare helps pay to rent your CPAP machine for a total of 13 months, but only if you continue to use it without interruption. After 13 months of rental, you own the CPAP machine.
How to qualify for CPAP?
To qualify for CPAP coverage, you must meet the following requirements: Complete a sleep test in a laboratory setting or by using an approved at-home test. Be diagnosed with obstructive sleep apnea based on sleep test results. Have a prescription for a CPAP machine from your doctor. Get the CPAP machine from a participating Medicare supplier.
How long does it take for CPAP to work?
Since CPAP treatment doesn’t work for everyone, Medicare first covers the machine for a three-month trial period. After three months , your doctor will check how the treatment is working for you.
How often do you need to replace CPAP?
Depending on the item, you may need replacements every two weeks to every six months. Talk with your doctor or supplier about scheduling replacement supplies.
What does Medicare Part B cover?
In addition to CPAP machines, Medicare Part B’s durable medical equipment benefit also covers CPAP supplies, such as face masks, tubing and filters . Medicare Part B pays 80 percent of the Medicare-approved amount, while you pay 20 percent as coinsurance.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. you pay 20% of the. Medicare-Approved Amount.
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.