If Medicare covers your genetic testing, there are some out-of-pocket costs you should expect to pay, which may include: Part B deductible Part B coinsurance or copayment Medicare Part B deductible and genetic tests For all beneficiaries, the Medicare Part B deductible is $233 per year in 2022.
Full Answer
Does Medicare cover genetic testing?
The health care professional performing the genetic test can explain any limitations known for a specific test and its common uses. In order for Medicare to cover genetic testing, certain requirements must be met.
Does Medicare cover multigene panel testing?
Medicare coverage of multigene panel testing is available in all Medicare regions, although eligibility for this testing varies by Medicare Administrative Contractor (MAC). First Coast Service Options and Novitas Solutions MACs have more narrow testing policies.
What is the CPT code for pharmacogenetic testing?
CPT Codes* Required Clinical Information Pharmacogenetic Testing 0173U 0175U 81479 Medical notes documenting all of the following:
Does Medicare cover every test?
Medicare coverage for many tests, items and services depends on where you live. This list only includes tests, items and services that are covered no matter where you live. If your test, item or service isn’t listed, talk to your doctor or other health care provider.
Does Medicare pay for pharmacogenetic testing?
Pharmacogenomics and Other Genetic Tests Medicare covers these tests when they are necessary for the diagnosis or treatment of certain kinds of leukemia and rare blood cancers. Cytogenetic studies may also be covered when they are used to diagnose or treat genetic disorders in a fetus or failure of sexual development.
How much does a pharmacogenetic test cost?
Treatment response rates, mortality rates, direct and indirect medical costs, and utility inputs were derived from the reference study and published scientific literature. The cost of the pharmacogenetic test was $2,000. A 3% discount rate was used to discount costs and effects.
Is pharmacogenetic testing covered by insurance?
The coverage of pharmacogenetic tests varied widely among companies. Overall, evidence-driven and medically recommended pharmacogenetic tests are not consistently available or covered by private health insurance companies, potentially impacting patients' health outcomes.
Is genome sequencing covered by Medicare?
Medicare has limited coverage of genetic testing for an inherited genetic mutation. Medicare covers genetic testing for people with a cancer diagnosis who meet certain criteria; you must have a cancer diagnosis to qualify for coverage of genetic testing for an inherited mutation under Medicare.
How accurate is pharmacogenetic testing?
Only 36% of the labels reviewed provided convincing evidence for the clinical validity of the pharmacogenetic test, that is, an established association between the pharmacogenetic variant and drug response; and only 15% provided convincing evidence of clinical utility, that is, one or more controlled studies ...
How much does genetic testing for antidepressants cost?
There are now genetic tests that claim to tell you how you'll respond to depression drugs. The tests can cost up to $2,000, and scientists are now questioning whether they're worth it.
Does UnitedHealthcare cover pharmacogenetic testing?
UnitedHealthcare's policy specifies that the use of pharmacogenetic multi-gene panels to guide therapy decisions is proven and medically necessary for antidepressants and antipsychotics medication when the following criteria are met: The individual has a diagnosis of major depressive disorder or anxiety; and.
Who should get pharmacogenetic testing?
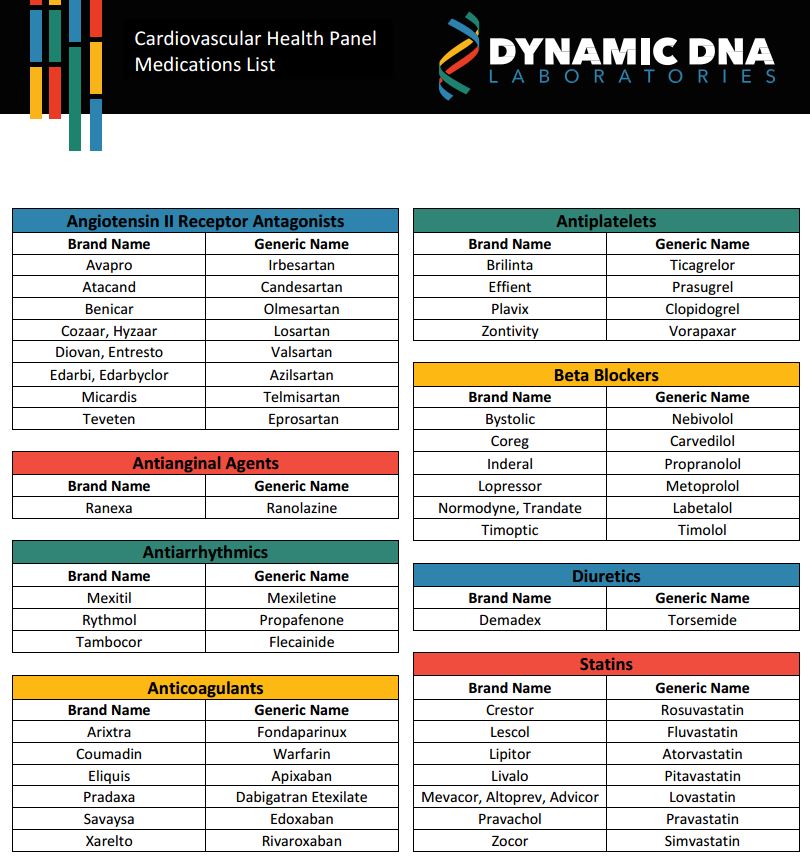
Q: When is Pharmacogenetic testing indicated?Over 65 years of age.Experiencing unwanted side effects from medication(s)Feels their medications aren't working.Currently taking or considering any of the medications on this list.
Does UnitedHealthcare cover GeneSight test?
Health insurance giant UnitedHealthcare has agreed to cover Myriad Genetics' GeneSight depression test, giving a boost to the diagnostic company's efforts to grow its sales.
Does Medicare cover biomarker testing?
Medicare covers a blood-based biomarker test (if available) once every 3 years.
Does Medicare pay for Mthfr testing?
There is broad consensus in the medical literature that MTHFR genotyping has no clinical utility in any clinical scenario. This testing is considered investigational and is NOT a Medicare benefit.
Is 81479 covered by Medicare?
Such testing is considered screening and is excluded by Medicare statute.
How often does Medicare cover colorectal cancer screening?
The only screening test Medicare will cover (once every three years) is to determine if a beneficiary has colorectal cancer. That test is appropriate when a beneficiary has no symptoms of colorectal cancer and only an average risk of developing it. [1] .
Should Medicare beneficiaries seek advice?
Beneficiaries should always seek the advice and orders of their treating physician on Medicare-coverage related issues. ...
Does Medicare cover genetic testing?
Medicare typically covers genetic tests only when a beneficiary has signs or symptoms that can be further clarified by diagnostic testing. Medicare also covers some genetic tests that assess an individual’s ability to metabolize certain drugs. The only screening test Medicare will cover (once every three years) is to determine if a beneficiary has colorectal cancer. That test is appropriate when a beneficiary has no symptoms of colorectal cancer and only an average risk of developing it. [1] Federal Regulation 42 CFR § 410.32 (a) requires genetic tests to be ordered by a physician who is treating the beneficiary.
How often does Medicare cover colorectal cancer screening?
Medicare Part B may also cover a screening test for colorectal cancer once every 3 years. If your genetic test is not covered by Medicare, you may be responsible for 100 percent of the cost.
What is Medicare Advantage?
Medicare Advantage plans are sold by private insurance companies and are an alternative to Original Medicare. Medicare Advantage plans cover the same benefits that are covered by Original Medicare.
How much is Medicare Part B deductible?
Medicare Part B deductible and genetic tests. For all beneficiaries, the Medicare Part B deductible is $198 per year in 2020.
Does Medicare cover genetic testing?
Medicare may cover genetic testing when it is ordered by a doctor, but only for specific types of cancer, and only if you meet certain criteria. Medicare Advantage (Part C) plans may also cover medically necessary genetic tests in very limited circumstances for certain types of cancer.
Does Medicare cover prescription drugs?
Many Medicare Advantage plans cover prescription drugs and offer annual out-of-pocket spending limits for Part A and Part B services, both of which are not offered by Original Medicare (Part A and Part B).
Does Medicare Advantage cover prescriptions?
Many Medicare Advantage plans may offer prescription drug coverage. Some plans may also offer coverage for routine dental, hearing and vision care, as well as some other benefits. A licensed insurance agent can help you compare available Medicare Advantage plans in your area. Call to speak with an agent today to learn if you’re eligible ...
What is the number to call for genetic testing?
FORCE's toll-free helpline: 866-288-RISK, ext. 704, can connect you with a volunteer board-certified genetic counselor who can answer general questions about genetic testing and hereditary cancer and help you find a genetic counselor near you.
What is a multigene panel?
A multigene panel is a type of genetic test that looks for inherited mutations in more than one gene at the same time. It might include testing for BRCA1 and BRCA2 mutations in addition to mutations in other genes such as ATM, PALB2, CHEK2, etc. Medicare covers panel testing when:
What is Medicare Rights Center?
Medicare Rights Center is a national nonprofit that works to ensure access to affordable health care for older adults and people with disabilities under the Medicare program. Patient Advocate Foundation provides case managers who help identify financial assistance programs and resources for those facing challenges.
Does Medicare cover genetic testing?
Medicare has limited coverage of genetic testing for an inherited genetic mutation. Medicare covers genetic testing for people with a cancer diagnosis who meet certain criteria; you must have a cancer diagnosis to qualify for coverage of genetic testing for an inherited mutation under Medicare. For people with a cancer diagnosis, Medicare policies ...
Does Medicaid cover genetic testing for Lynch syndrome?
The majority of states cover testing for a Lynch syndrome mutation (MLH1, MSH2, MSH6, PMS2, or EPCAM) for qualifying individuals, including people with a known genetic mutation in the family, or specific personal and/or family history of cancer. As of 2020, the following Medicaid programs did not cover genetic counseling or testing ...
Does Medicaid cover Lynch syndrome?
As of 2020, the following Medicaid programs did not cover genetic counseling or testing for Lynch syndrome: Alabama, Delaware, North Carolina, Nevada, Rhode Island and South Carolina. There is limited or questionable coverage in New Hampshire, South Dakota, Tennessee and Utah. Multigene panel testing —a type of genetic test ...
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) DL39063 Pharmacogenomics Testing. Please refer to the LCD for reasonable and necessary requirements.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted. The following ICD-10-CM code supports medical necessity and provides coverage for CPT code: 81220.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.