generic denial code. generic reason statement. n522. this is a duplicate claim billed by the same provider. 18. gba01. this is a duplicate service previously submitted by the same provider. refer to iom, pub 100-04, medicare claims processing manual chapter 1 section 120-120.3. n522. this is a duplicate claim billed by different provider. 18 . gba02
What is a N522 claim?
Dec 03, 2020 · Description. Reason Code: 18. Exact duplicate claim/service. Remark Code: N522. Duplicate of a claim processed, or to be processed, as a crossover claim.
What is a Medicare denial code?
Medicare denial code and Description ... claim adjustment reason, and remittance advice remark codes to communicate clearly why an amount is not covered by Medicare and who is financially responsible for that amount. Valid Group Codes for use on Medicare remittance advice: ... N163 Medical record does not support code billed per the code ...
What is the difference between N9 adjustment and denial?
Dec 01, 2021 · Electronic Remit Advice (ERA) and Standard Paper Remit (SPR) After Medicare processes a claim, either an ERA or an SPR is sent with final claim adjudication and payment information. One ERA or SPR usually includes adjudication decisions about multiple claims. Itemized information is reported within that ERA or SPR for each claim and/or line to ...
What is the difference between 5555 and 56 claim denial?
Remittance Advice Remark Codes (RARCs) are used to provide additional explanation for an adjustment already described by a Claim Adjustment Reason Code (CARC) or to convey information about remittance processing. ... Medicare Part B does not pay for items or services provided by this type of practitioner for beneficiaries in a Medicare Part A ...

What are remittance advice Remark codes?
What are the denial codes?
- 1 – Denial Code CO 11 – Diagnosis Inconsistent with Procedure. ...
- 2 – Denial Code CO 27 – Expenses Incurred After the Patient's Coverage was Terminated. ...
- 3 – Denial Code CO 22 – Coordination of Benefits. ...
- 4 – Denial Code CO 29 – The Time Limit for Filing Already Expired. ...
- 5 – Denial Code CO 167 – Diagnosis is Not Covered.
What is remark code M51?
What does co A1 mean?
How do Medicare denials work?
- Examine the Explanation of Benefits (EOB) from the carrier, which should include the reason for a claims denial. ...
- Have a standardized letter handy asking the insurance carrier to reconsider your claim. ...
- Consider invoking your right to an appeal an adverse claims decision.
How do denials work?
What does denial code PR 16 mean?
What is denial code N479?
What does denial code M86 mean?
What is denial code CO 204?
What is denial code P12?
What is a Medicare denial code?
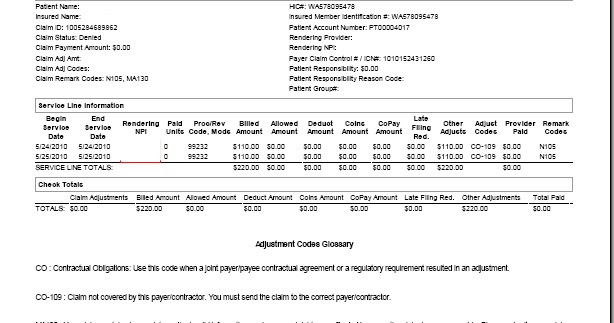
Medicare denial code - Full list - Description. Medicare denial code and Description. A group code is a code identifying the general category of payment adjustment. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service.
What is a group code in Medicare?
Medicare denial code and Description. A group code is a code identifying the general category of payment adjustment. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service. MACs do not have discretion to omit appropriate codes and messages.