What are modifiers? For Medicare purposes, modifiers are two-digit codes that may consist of alpha and/or numeric characters, which may be appended to procedure codes and/or HCPCS codes, to provide additional information needed to process a claim. This includes both HCPCS Level 1 (CPT) and HCPCS Level II codes.
Which modifier goes first 25 or 95?
You put the modifier that affects payment the most first. Since AI is informational only and the 25 determine if the visit level should be paid ... put the 25 first then the AI You must log in or register to reply here.
What is Kx modifier with Medicare?
KX Modifier Thresholds (formerly known as Therapy Cap Process) Under Medicare Part B, the annual limitations on per beneficiary incurred expenses for outpatient therapy services are commonly referred to as “therapy caps” now known as KX modifier thresholds. The KX modifier thresholds are determined on a calendar year basis, which means that all beneficiaries begin a new threshold amount each year.
What is a Gy modifier for Medicare?
- Are proper and needed for the diagnosis or treatment of the patient’s medical condition
- Are furnished for the diagnosis, direct care, and treatment of the patient’s medical condition
- Meet the standards of good medical practice
- Are not mainly for the convenience of the patient, provider, or supplier Examples of services that are covered include:
When to use Medicare ABN claim modifiers?
You may also use the ABN as a voluntary notice to alert patients of their financial liability prior to providing care that Medicare never covers. An ABN is not required to bill a patient for an item or service that is not a Medicare benefit and is never covered. Medicare prohibits routine issuing of ABNs.
Which modifier is used for Medicare patients?
The GA modifier must be used when physicians, practitioners, or suppliers want to indicate that they expect that Medicare will deny a service as not reasonable and necessary and they do have on file an ABN signed by the beneficiary.
What does patient modifier mean?
Sep 6. A medical coding modifier is two characters (letters or numbers)appended to a CPT or HCPCS level II code. The modifier provides additional information about the medical procedure, service, or supply involved without changing the meaning of the code.
What does modifier mean?
Non-physician Assisting at SurgeryModifier AS – Non-physician Assisting at Surgery Medicare has established the -AS modifier to report Physician Assistant (PA), Nurse Practitioner (NP), or Clinical Nurse Specialist (CNS) services for assistant-at-surgery, non-team member.
What are payment modifiers?
Modifier: Two digit numeric or alpha-number descriptor that is used by providers to indicate that a service or procedure has been altered by a specific circumstance, but the procedure code and definition is unchanged. 4.
What does modifier mean in medical billing?
A medical coding modifier is two characters (letters or numbers) appended to a CPT® or HCPCS Level II code. The modifier provides additional information about the medical procedure, service, or supply involved without changing the meaning of the code.
How do you know when to use a modifier?
Modifiers should be added to CPT codes when they are required to more accurately describe a procedure performed or service rendered.
What are healthcare modifiers?
What are Modifiers? According to the AMA and the CMS, a modifier provides the means to report or indicate that a service or procedure has been performed and altered by some specific circumstance but not changed in definition.
What is an example of a modifier?
A modifier is a word, phrase, or clause that modifies—that is, gives information about—another word in the same sentence. For example, in the following sentence, the word "burger" is modified by the word "vegetarian": Example: I'm going to the Saturn Café for a vegetarian burger.
What are Medicaid modifiers?
According to the American Medical Association (AMA) and the Centers for Medicare and Medicaid Services (CMS), a modifier provides the means to report or indicate that a service or procedure that has been performed has been altered by some specific circumstance but not changed in its definition or code.
Why do we use modifiers in medical billing?
Modifiers are added to the Healthcare Common Procedure Coding System (HCPCS) or Current Procedural Terminology (CPT®) codes to provide additional information necessary for processing a claim, such as identifying why a doctor or other qualified healthcare professional provided a specific service and procedure.
Do modifiers affect payment?
How does a modifier affect payment? In some cases, addition of a modifier may directly affect payment. Placement of a modifier after a CPT or HCPCS code does not insure reimbursement. Medical documentation may be requested to support the use of the assigned modifier.
How many modifiers are there in medical billing?
59- Distinct Procedural Services. 99- Multiple modifiers.
Why do medical coders use modifiers?
Medical coders use modifiers to tell the story of a particular encounter. For instance, a coder may use a modifier to indicate a service did not occur exactly as described by a CPT ® or HCPCS Level II code descriptor, but the circumstance did not change the code that applies. A modifier also may provide details not included in the code descriptor, ...
Why is it important to use modifiers?
Proper use of modifiers is important both for accurate coding and because some modifiers affect reimbursement for the provider. Omitting modifiers or using the wrong modifiers may cause claim denials that lead to rework, payment delays, and potential reimbursement loss.
What is NCCI PTP modifier?
An NCCI PTP-associated modifier is a modifier that Medicare and Medicaid accept to bypass an NCCI PTP edit under appropriate clinical circumstances. Bypassing or overriding an edit is also called unbundling.
What is a pricing modifier?
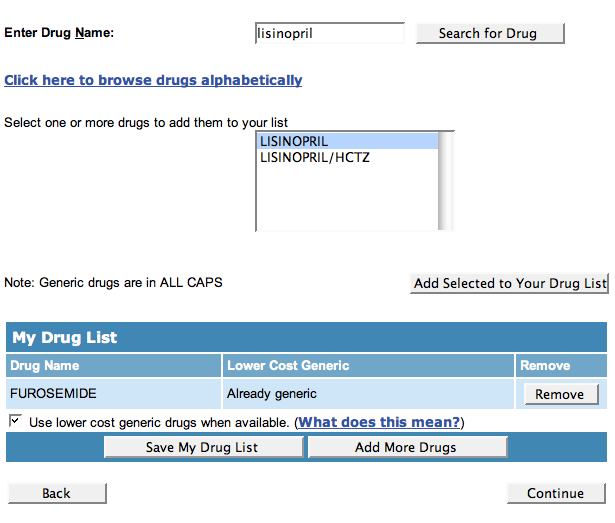
A pricing modifier is a medical coding modifier that causes a pricing change for the code reported. The Multi-Carrier System (MCS) that Medicare uses for claims processing requires pricing modifiers to be in the first modifier position, before any informational modifiers. On the CMS 1500 claim form, the appropriate field is 24D (shown below). You enter the pricing modifier directly to the right of the procedure code on the claim. Most providers use the electronic equivalent of this form to bill Medicare for professional (pro-fee) services.
What is a modifier 59?
Modifier 59 Distinct procedural service is a medical coding modifier that indicates documentation supports reporting non-E/M services or procedures together that you normally wouldn’t report on the same date. Appending modifier 59 signifies the code represents a procedure or service independent from other codes reported and deserves separate payment.
What is informational modifier?
An informational modifier is a medical coding modifier not classified as a payment modifier. Another name for informational modifiers is statistical modifiers. These modifiers belong after pricing modifiers on the claim.
Why is modifier 59 difficult to master?
Like modifier 25, modifier 59 is difficult to master because it requires determining whether the code is truly distinct and separately reportable from other codes. The CPT ® definition of modifier 59 advises that the modifier may be appropriate for a code when documentation shows at least one of the following:
What is a modifier code?
Modifiers are two-digit codes that are appended to a service as a means to indicate that the service/procedure is affected or altered by a specific circumstance and to add specificity, but not changed in its definition.
What modifiers are used in CPT?
HCPCS modifiers may also be used with CPT codes and/or in combination with CPT modifiers. CPT modifiers may also be used with HCPCS codes and/or in combination with HCPCS modifiers. For example, -TC and –76 can be appended to a radiology procedure to indicate the technical component of the services was repeated.
What is an E/M modifier?
(E/M) service you are indicating that the patient’s condition requires a significant, separately identifiable E/M service above and beyond the other service provided, or beyond the usual pre-operative and postoperative care associated with the procedure that was performed. Services appended with a –24 modifier must be sufficiently documented in the patient’s medical record that the visit was unrelated to the post-operative care of the procedure.
Does the 51 modifier affect payment?
It is not necessary to append the –51 modifier to “add on” or to exempt codes. Applicable code edits will be applied to services submitted. The -51 modifier itself does not affect payment. Multiple surgical payment is based on whether the surgical procedure may be subject to a multiple surgery.
Modifier 53
As noted earlier, the qualifying discontinued service codes for modifier 53 are very specific. CPT® Appendix A states, “Under certain circumstances, the physician may elect to terminate a surgical or diagnostic procedure.
Appropriate use
This modifier is often used with both diagnostic and surgical CPT codes.
Are You Ready to Get Billing?
Want to have an error-free billing and coding expert at your work? You are at the right place, what you need now is a partner who can finish out the rest of the work and make the technology and implementation just as simple. That’s what the best medical billing company like Medisys Data Solutions Inc can do.
What is Medicare Access and CHIP Authorization Act?
The Medicare Access and CHIP Authorization Act of 2015 ( MACRA) requires the Centers for Medicare & Medicaid Services (CMS) to implement patient relationship categories and codes to attribute patients and episodes to one or more clinicians for purposes of cost measurement. Clinicians are not required to include the applicable patient relationship ...
Is HCPCS Level II voluntary?
Are your clinicians reporting patient relationship codes on their Medicare Part B claims? The HCPCS Level II modifiers are voluntary this year, making it a good time to get in practice.
