What does MSP healthcare mean?
10 meanings of MSPabbreviation related to Medicare: Medicare Medicare Medicare Technology Business Medical Education 1/ 10 Sort Sort Rating A-Z Short first Long first MSP Medicare Abbreviation Suggest to this list Related acronyms and abbreviations Abbr. Meaning Share MSP Medicare Abbreviationpage APA All Acronyms. 2022. MSP.
What does a MSP mean?
Medicare Secondary Payer (MSP) is a term used when Medicare is not responsible for paying first on a healthcare claim. The decision as to who is responsible for paying first on a claim and who pays second is known in the insurance industry as “coordination of benefits.”
What is Medicare Secondary Payer (MSP)?
MSP stands for Medicare Savings Program. Suggest new definition. This definition appears very frequently and is found in the following Acronym Finder categories: Military and Government. Science, medicine, engineering, etc. See other definitions of MSP. Other Resources:
What is the Medicare Savings Program (MSP)?
Feb 10, 2021 · Medicare secondary payer (MSP) billing What you need to know. The MSP provisions apply to situations when Medicare is not the …
What is an MSP plan?
Slide notes. Medicare Secondary Payer (MSP) is a term used when Medicare is not responsible for paying first on a healthcare claim. The decision as to who is responsible for paying first on a claim and who pays second is known in the insurance industry as “coordination of benefits.”Apr 4, 2022
What are the MSP types?
Valid MSP Types for Electronic ClaimsMSP TypeDescription13End-Stage Renal Disease (ESRD): 30-month initial coordination period in which other insurer is primary14No-fault situations: Medicare is secondary if illness/injury results from a no-fault liability.15Workers' compensation (WC) situations41Black Lung benefits3 more rows•Jan 4, 2021
What is MSP type working aged?
Working Aged – Beneficiaries age 65 or older who are insured through their own or their spouse's current employment. The beneficiary must be aged 65 or older. There must be at least 20 or more employees. Disability – This coverage is for beneficiaries who are under age 65 and disabled.Jun 27, 2018
Does MSP mean Medicare is secondary?
What is a MSP? MSP stands for Medicare Secondary Payer and describes when another payer is responsible for paying a beneficiary's claims before Medicare kicks in. The first payer is determined by the patient's coverage. Different conditions determine if Medicare will be the primary, secondary, or tertiary payer.
What insurance does an MSP need?
cyber insuranceAn MSP company needs a full cyber insurance policy. It should cover areas like cyber extortion, network security liability, legal and forensic expense, privacy liability, media liability, damage cost for data or programs, and more.
Is Medicare always the primary payer?
), Medicare pays first. If you have Medicare due to ESRD, COBRA pays first and Medicare pays second during a coordination period that lasts up to 30 months after you're first eligible for Medicare. After the coordination period ends, Medicare pays first.
How do I bill a MSP claim?
MSP claims are submitted using the ANSI ASC X12N 837 format, or by entering the claim directly into the Fiscal Intermediary Standard System (FISS) via Direct Data Entry (DDE). If you need access to FISS in order to enter claims/adjustments via FISS DDE, contact the CGS EDI department at 1.877.Dec 17, 2020
What does working aged mean for Medicare?
To recap, Medicare is the secondary payer under the Working Aged provision when: the beneficiary is. age 65 or older and his/her Medicare entitlement is due to age; the insured person under the GHP is. the beneficiary or the spouse of the beneficiary; the insured person under the GHP has current.Apr 4, 2022
Can providers and other health care professionals may enroll in the Medicare program and also be selected as a provider in a Medicare Advantage MA plan?
A. Beneficiaries must be entitled to Medicare Part A, enrolled in Part B, and live in the plan service area to be eligible to enroll in an MA Plan. Providers and other health care professionals may enroll in the Medicare Program and also be selected as a provider in a Medicare Advantage (MA) Plan.
Is MSP required for Medicare Advantage plans?
The Medicare Advantage program was created under Part C of the Medicare statutes to serve as an alternative delivery vehicle for Medicare benefits, but as far as the MSP regulations and CMS are concerned, Medicare Advantage plans have the same rights and responsibilities for MSP enforcement as traditional Medicare ...Aug 28, 2019
How do you find MSP?
The MSP Questionnaire Form can be found at: www.cms.gov/Medicare/Coordination-of-Benefits-and-Recovery/ProviderServices/Downloads/CMS-Questionnaire.pdf. Please remember that there may be situations where more than one payer is primary to Medicare (e.g., liability insurer and group health plan [GHP]).
What is MSP 14?
14. PP. Beneficiary paid by liability insurer. Used only for conditional claims involving liability insurance payments to the beneficiary where the provider is not expecting any payment from the beneficiary. Report OC 24 with date insurance denied.Feb 12, 2013
MSP stands for Medicare Savings Program
This definition appears very frequently and is found in the following Acronym Finder categories:
Samples in periodicals archive
1, 2012 HOUSE PROVISIONS: * Personal asset limits for Medicare Savings Program and Part D increased.
What is MSP in Medicare?
The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage. Physicians, non-physician practitioners and suppliers are responsible for gathering MSP data to determine whether Medicare is the primary payer by asking Medicare beneficiaries questions concerning their MSP status.
What is MSP billing?
MSP billing. When Medicare is the secondary payer, submit the claim first to the primary insurer. The primary insurer must process the claim in accordance with the coverage provisions of its contract. If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, ...
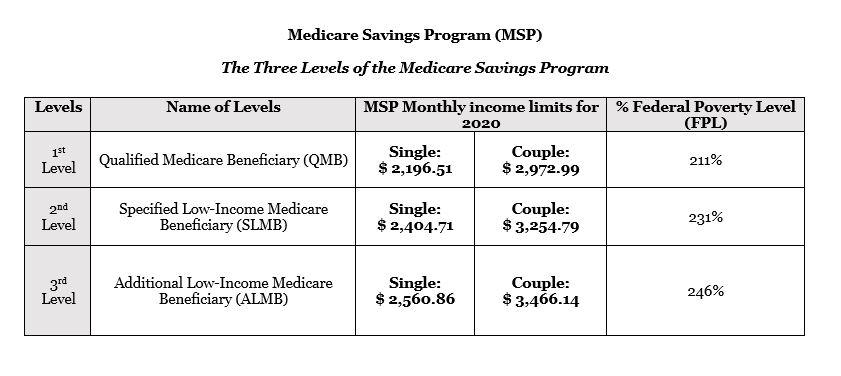
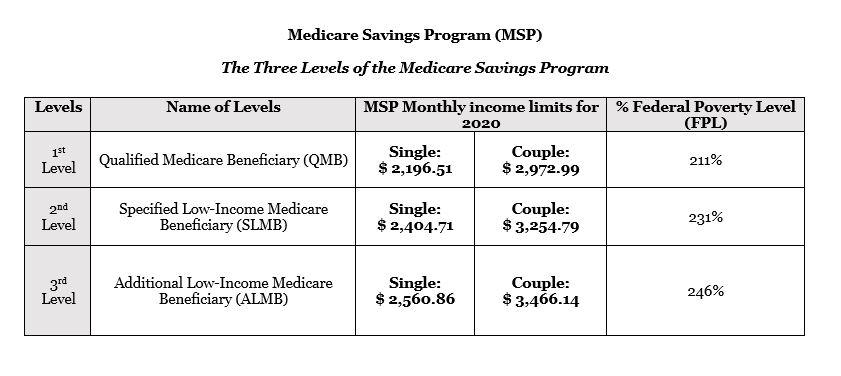
Here is your Connecticut Medicare Savings Program Dictionary
ALMB: (eh-LIM-be ̅) n. 1. “Additional Low-Income Medicare Beneficiary” 2. One of three Medicare Savings Programs that requires proactive enrollment and annual renewal that pays for the Medicare Part B premium for Medicare enrollees not on Medicaid 3. An unmarried Medicare enrollee whose gross monthly income is under $2,641 (Connecticut) 4.
How To Apply For Medicare Savings Program?
If you believe you or someone you love might qualify for the MSP benefit, you can apply at any time. The application process is not that difficult and You can be approved fairly quickly (it is much faster and easier than applying for State benefits for home care or nursing home).