Mandatory benefits include services including inpatient and outpatient hospital services, physician services, laboratory and x-ray services, and home health services, among others. Optional benefits include services including prescription drugs, case management, physical therapy, and occupational therapy.
Full Answer
What does “your Medicare benefits” mean?
Your Medicare Benefits The information in “Your Medicare Benefits” describes the Medicare Program at the time it was printed. Changes may occur after printing. Visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) to get the most current information. TTY users can call 1-877-486-2048. “Your Medicare Benefits” isn’t a legal document.
What are the Medicare Advantage Benefits?
One of the primary benefits of Medicare as a social program is that the financial risk is distributed across the working population. This means that the nation as a whole assumes financial risk for factors that might raise someone’s premiums substantially.
Why is Medicare considered a social program?
If you are over 18 and under age 65, you may qualify for Medicare benefits if you: Have received Social Security disability benefits (SSDI) for at least 2 years, OR. Have been diagnosed with Lou Gehrig’s Disease, also called Amyotrophic Lateral Sclerosis (ALS), AND. Are starting to get Social Security disability.
Do Medicare Advantage benefit periods differ from Original Medicare Part A?
Medicare benefit periods mostly pertain to Part A, which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you...
What do Medicare benefits mean?
Each month you fill a prescription, your Medicare Prescription Drug Plan mails you an "Explanation of Benefits" (EOB). This notice gives you a summary of your prescription drug claims and costs.
What are the Medicare benefit categories?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Can you use up your Medicare benefits?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
What happens when you run out of Medicare days?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row.
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Does Medicare cover dental?
Dental services Medicare doesn't cover most dental care (including procedures and supplies like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices). Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Do you have to pay back Medicare?
The Nature of the Medicare Medical Lien This means that if you get a settlement, you will have to pay back Medicare before anything else gets taken out. While you can get the lien reduced, paying back Medicare after a settlement is not optional. The only path around a Medicare lien is to negotiate the lien to zero.Dec 9, 2021
Does Medicare pay for ultrasounds?
Medicare can cover all or part of the health care costs of having a baby, including: your doctor or GP fees. ultrasounds and blood tests. midwife and obstetric fees.
What are the disadvantages to a Medicare Advantage Plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
Does Medicare pay 100 percent of hospital bills?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
What is the Medicare Part A benefit period?
In Medicare Part A, which is hospital insurance, a benefit period begins the day you go into a hospital or skilled nursing facility and ends when you have been out for 60 days in a row. If you go back into the hospital after 60 days, then a new benefit period starts, and the deductible happens again.
What is the Medicare 2 midnight rule?
The Two-Midnight rule, adopted in October 2013 by the Centers for Medicare and Medicaid Services, states that more highly reimbursed inpatient payment is appropriate if care is expected to last at least two midnights; otherwise, observation stays should be used.Nov 1, 2021
What is HMO in healthcare?
Lawmakers approved the cooperation between Medicare and health maintenance organizations (HMOs). HMOs act as liaisons between healthcare providers and beneficiaries. People who subscribe to HMO plans usually have to go to a select list of providers that has been approved by the HMO administrators.
How long did it take for Medicare to become law?
However, the path to Medicare wasn’t always smooth sailing. A bill for socialized healthcare was first introduced in 1957, and it took eight years for Medicare to become law. The Johnson administration and lawmakers at the time debated extensively on the concept.
What changes have affected Medicare?
One of the changes that had the biggest impact on Medicare was the decision to include people with certain disabilities as beneficiaries of the program. People with end-stage renal disease (ESRD) or Lou Gehrig’s disease can receive Medicare benefits if they also receive Social Security Disability Insurance.
How much does an employer pay for Medicare?
For people who work for an employer, the employer pays half of the Medicare tax while the worker pays the other half. The Medicare tax rate is 2.9 percent, which means that an employer pays 1.45 percent while the remaining 1.45 percent is deducted from the employee’s wages.
How is Medicare funded?
While Medicare is funded primarily through taxes, there are actually several sources of funding. It’s important to understand the financing behind Medicare because the future of the program largely depends on continued funding from individual taxes and other sources. Social programs only succeed in light of their perceived benefit versus the amount of money it takes to sustain them. These programs fail when they lose financial and moral support. In this section, we’ll give you a basic overview of how Medicare is funded so that you’re familiar with its impact on the economy and the healthcare industry as a whole.
What is the benefit of Medicare?
One of the primary benefits of Medicare as a social program is that the financial risk is distributed across the working population. This means that the nation as a whole assumes financial risk for factors that might raise someone’s premiums substantially.
What is Medicare's coverage for speech therapy?
These forms of care help seniors, particularly those with disabilities, to achieve alternate forms of medical treatments.
How much coinsurance do you pay for inpatient care?
Days 1 through 60. For the first 60 days that you’re an inpatient, you’ll pay $0 coinsurance during this benefit period. Days 61 through 90. During this period, you’ll pay a $371 daily coinsurance cost for your care. Day 91 and up. After 90 days, you’ll start to use your lifetime reserve days.
How long does Medicare benefit last after discharge?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days after being discharged, the benefit period ends. Keep reading to learn more about Medicare benefit periods and how they affect the amount you’ll pay for inpatient care. Share on Pinterest.
What facilities does Medicare Part A cover?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility. hospice. If you have Medicare Advantage (Part C) instead of original Medicare, your benefit periods may differ from those in Medicare Part A.
What is Medicare benefit period?
Medicare benefit periods mostly pertain to Part A , which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you identify your portion of the costs. This amount is based on the length of your stay.
Why is it important to check deductibles each year?
It’s important to check each year to see if the deductible and copayments have changed, so you can know what to expect. According to a 2019 retrospective study. Trusted Source. , benefit periods are meant to reduce excessive or unnecessarily long stays in a hospital or healthcare facility.
How much is Medicare deductible for 2021?
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What are the benefits of Medicare Advantage?
In some cases, you may be able to enroll in a Medicare Advantage plan that covers alternative therapies such as chiropractic care and even acupuncture. In addition, your plan may include other comprehensive benefits such as: 1 Counseling to manage life changes, conflict resolution, and grief in both individual and group sessions that would not otherwise be covered under Original Medicare. 2 Enhanced disease management services for people with serious or chronic medical conditions such as heart disease, diabetes, and Alzheimer’s and related dementias. 3 Bathroom safety devices and safety counseling for individuals at risk for falls. Your plan may also cover a comprehensive in-home safety assessment to help minimize the risk of injury and falls at home. 4 Temporary home meal delivery for up to four weeks following surgery or inpatient hospital stay 5 Personal emergency response system to notify emergency personnel in the event of fall or other medical event. 6 Telemedicine or other remote health services, including a nursing hotline; in some cases, you may also qualify for remote monitoring devices. 7 Transportation assistance to get you to and from covered health care appointments. 8 Wigs for hair loss following chemotherapy for cancer.
Does Medicare cover chiropractic care?
In some cases , you may be able to enroll in a Medicare Advantage plan that covers alternative therapies such as chiropractic care and even acupuncture. In addition, your plan may include other comprehensive benefits such as:
Do you have to pay a deductible on Medicare Advantage?
Keep in mind that there may be annual limits and restrictions on these additional Medicare Advantage benefits, and that you may need to pay a deductible, copayment, or coinsurance amount when you access them. If these benefits are important to you, check your plan documents before you enroll in a Medicare Advantage plan.
Do you lose Medicare Advantage benefits if you switch?
Under federal law, all Medicare Advantage plans must include, at a minimum, all the benefits included in Original Medicare, except for hospice care, which is still covered under Medicare Part A. You do not lose any benefits if you enroll in or switch to a Medicare Advantage plan. However, you may be able to enroll in a plan ...
Is Medicare Advantage available?
There are many different Medicare Advantage benefits available depending on the plan you choose. Because these plans are offered by private companies approved by Medicare, they can offer extra benefits not available under Original Medicare. Find affordable Medicare plans in your area. Find Plans.
Does Medicare cover eye exams?
Original Medicare does not cover routine eye exams or prescription eye glasses except in certain limited situations. However, depending on where you live, you may have Medicare Advantage benefits for routine vision care, prescription eyewear, and contact lenses. Dental care.
Does Medicare Advantage cover prescription drugs?
Most Medicare Advantage plans include Part D prescription drug coverage, but be sure to read your plan documents to understand what medications are covered, if any, and your financial responsibility for covered medications, since this can vary greatly from plan to plan.
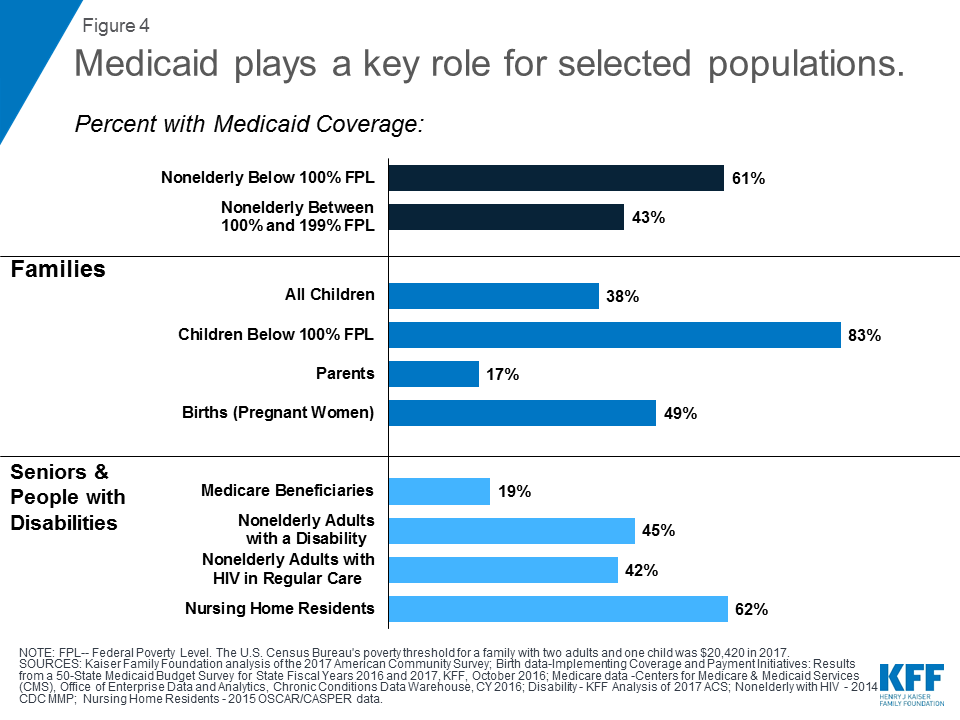
What is the difference between Medicare and Medicaid?
Original Medicare is available to individuals 65 years of age or older and individuals with certain disabilities. Medicaid insurance caters to individuals with low income and provides an affordable, government-funded healthcare option for this demographic. The QMB program has specific income requirements that must be met, ...
What does QMB mean for medicaid?
What Does Medicaid QMB Cover? Medicaid QMB, which stands for Qualified Medicare Beneficiary , is a program designed specifically for individuals that qualify for both Medicare and Medicaid coverage and that are financially unstable.
How many people were in the QMB in 2016?
The amounts of the QMB requirements and the poverty line generally coincide, but it is good to be aware of both. In 2016, there were approximately 7.5 million individuals that are a part of the QMB program. In fact, nearly one out of every eight Medicare recipients was a member of this program.
What is qualified Medicare Beneficiary?
The Qualified Medicare Beneficiary program works to help cover Medicare Part A and Part B premiums, as well as the costs of coinsurance, copayments, and deductibles. All of these costs can add up quickly, especially if you require a variety of different medical services. This program is able to provide full payment of both ...
What is the income limit for 2019?
In 2019, the monthly income limits for individuals is $1,060 and the monthly income limit for a married couple is $1,430. There is also a limit on resources, which is set at $7,730 for individuals and $11,600 for married couples. Additionally, you must also be at or below the annual federal poverty level. The amounts of the QMB requirements and the ...
Do you have to accept Medicare and QMB?
They must accept Medicare and QMB payment for their services and recognize this payment as being the full amount of the cost of service . Improper billing protections prevent individuals using the QMB program from being responsible for any cost-sharing expenses, no matter their origin.
Is Medigap covered by QMB?
It is important to note that if you are currently using a Medigap plan, the premiums associated with it are not covered by the QMB program. In addition, you should also be aware that states can impose laws specific to Medicaid, Medicare, and QMB programs.
What is the income limit for Medicaid expansion?
133% FPL is the income limit used to expand Medicaid to adults in states that opted in to Medicaid expansion under the Affordable Care Act (ACA, or "Obamacare") Medica id expansion allows 5% of income to be ignored, however, so really those under 138% of the poverty level may qualify for Medicaid in expansion states.
What is 150% FPL?
150% FPL is the limit for Medicare Part D's Extra Help partial subsidy, which provides reduced premiums and deductibles and reduced per prescription copayments. 150% FPL (for two people) is also the limit used for the " minimum monthly maintenance needs allowance " for individuals whose spouse is in a Medicaid-paid nursing home.
How much is the SSI limit for nursing homes in 2021?
In 2021, 300% of the SSI limit is $2,382 per month. For more information on eligibility for Medicaid-paid nursing homes, see our section on Medicaid for Nursing Homes. Updated February 11, 2021.
What is the Medicare Savings Program?
This is a Medicare Savings Program that you may be eligible for if you qualify for Medicare because you are 65 or older or are disabled.
What is the FPL in the federal government?
Many federal and state government benefits are tied to the federal poverty level (FPL), or percentages of the FPL. The FPLs, which are also called the federal poverty guidelines, are updated every year.
Can a pregnant woman get medicaid?
Also, in some states, children and pregnant women under 133% FPL qualify for Medicaid, and in other states, parents or even childless adults can qualify for Medicaid with income under this level.
Is SSI tied to poverty?
Note that SSI, which is based on the federal benefit rate, is no longer tied to the poverty level; instead it receives a cost-of-living adjustment each year. For comparison purposes, the federal benefit rate for SSI is about 75% of the FPL for one person.
