
While this is a popular program in the US, sometimes Medicare is denied attributing the denial to- “Denial Code CO 22 – The care may be covered by another payer per coordination of benefits, and hence the denial” and “Denial Code CO 24 – The charges are covered under a capitation agreement or managed care plan”
What does OA 4 mean on a Medicare Code?
This new reason code enables Medicare to communicate the message that coinsurance or deductible cannot be collected from the patient. OA 4 The procedure code is inconsistent with the modifier used or a required modifier is missing.
What is the OA code for denied?
OA 155 This claim is denied because the patient refused the service/procedure. OA 192 Non standard adjustment code from paper remittance advice. OA 199 Revenue code and Procedure code do not match. OA 209 Per regulatory or other agreement.
What is a Medicare denial code?
Medicare denial codes are standard messages used to provide or describe information to a medical patient or provider by insurances about why a claim was denied. This is the standard format followed by all insurances for relieving the burden on the medical provider.
What does MCR-835 denial code list OA mean?
MCR - 835 Denial Code List OA : Other adjustments OA Group Reason code applies when other Group reason code cant be applied. Its mostly like that payment is not considered due to coverage problem and some other party is responsible for that claim like the below reason. Benefits were not considered by the other payer because patient is not covered.
What is denial Reason code 24?
“Denial Code CO 24 – The charges are covered under a capitation agreement or managed care plan”
What does denial code OA mean?
Other AdjustmentsOA (Other Adjustments): It is used when no other group code applies to the adjustment. PI (Payer Initiated Reductions): It is used by payers when it is believed the adjustment is not the responsibility of the patient, but there is no supporting contract between the provider and payer.
What does OA mean on Medicare EOB?
Other AdjustmentsOA (Other Adjustments) is used when CO (Contractual Obligation) nor PR (Patient Responsibility apply. This can be used when the claim is paid in full and there is no contractual obligation or patient responsibility on the claim.
What does OA stand for in medical billing?
Physician assistantsPAs: Physician assistants PAs work in primary and specialty care under the direction and supervision of a licensed physician.
What is adjustment OA 23?
OA-23: Indicates the impact of prior payers(s) adjudication, including payments and/or adjustments. No action required since the amount listed as OA-23 is the allowed amount by the primary payer. OA-109: Claim not covered by this payer/contractor. You must send the claim to the correct payer/contractor.
What does code OA 18 mean?
Q: We are receiving a denial with claim adjustment reason code (CARC) OA18. What steps can we take to avoid this denial code? A: You will receive this reason code when more than one claim has been submitted for the same item or service(s) provided to the same beneficiary on the same date(s) of service.
What does OA A1 mean?
OA A1 Claim/Service denied. At least one Remark Code must be provided (may be comprised of either the Remittance Advice Remark Code or NCPDP Reject Reason Code.)
What does denial code OA 133 mean?
Reason Code 133: Failure to follow prior payer's coverage rules. ( Use Group Code OA). This change effective 7/1/2013: Failure to follow prior payer's coverage rules. ( Use only with Group Code OA)
What is OA 45 Adjustment code?
45. Charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement. Usage: This adjustment amount cannot equal the total service or claim charge amount; and must not duplicate provider adjustment amounts (payments and contractual reductions) that have resulted from prior payer(s) adjudication. (
What is the difference between a PA C and an MD?
Duties that MDs and PAs Can Perform Another major difference between an MD and a PA is that doctors can legally practice independently while a PA always requires supervision. Both can do the following: Diagnose and treat patients. Perform medical procedures in the office.
Are Physician Assistants doctors?
Physician assistants are medical professionals who work under the delegated authority of a medical practitioner. Physician assistants are generalist trained, augmenting the services traditionally provided by a doctor.
What does PA mean in healthcare?
physician assistantA physician assistant (PA) is a licensed medical professional who holds an advanced degree and is able to provide direct patient care. They work with patients of all ages in virtually all specialty and primary care areas, diagnosing and treating common illnesses and working with minor procedures.
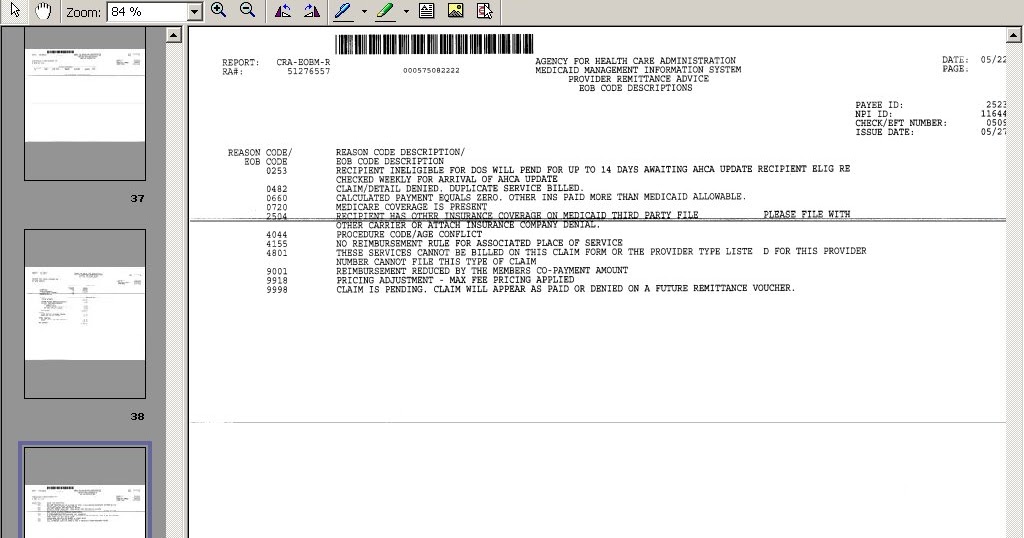
What is a Medicare denial code?
Medicare denial code - Full list - Description. Medicare denial code and Description. A group code is a code identifying the general category of payment adjustment. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service.
What is a CO code?
CO or contractual obligations is the group code that is used whenever the contractual agreement existing between the payee and payer or the regulatory requirement has resulted in a proper adjustment.
What is Medicare group code?
Medicare Group Codes. A group code is a code identifying the general category of payment adjustment. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service. MACs do not have discretion to omit appropriate codes and messages.
What is a group code in CARC?
Group codes are codes that will always be shown with a reason code to indicate when a provider may or may not bill a beneficiary for the non-paid balance of the services furnished. Payment Adjustment Category Description. • PR (Patient Responsibility).
What is ASC X12 835?
A particular ASC X12 835 reason or remark code might be mapped to one or more shared system codes, or vice versa, making it difficult for a MAC to determine each of the internal codes that may be impacted by remark or reason code modification, retirement, or addition.
What is reason and remark code?
In most cases, reason and remark codes reported in remittance advice transactions are mapped to alternate codes used by a shared system. These shared system codes may exceed the number of the reason and remark codes approved for reporting in a remittance advice transaction.
Do you need separate reason codes in the NSF?
Separate reason code entries must be used in the NSF for the CR group entry and any other groups that apply to the readjudicated claim. At least one reason code is always used with a group code in the NSF .
Can deactivated code be used in derivative business messages?
The Shared System Maintainers shall make sure that a deactivated code (either reason or remark) is not allowed to be used in any original business message, but is allowed and processed when reported in derivative business messages.
What is Medicare Advantage?
Medicare Advantage (MA): • If a Medicare beneficiary enrolls into a Medicare Advantage plan, that health plan will then replace the beneficiary’s traditional Medicare plan. • Medicare claims must be submitted to the MA plan. • If a claim is submitted to Medicare it will be returned as an unprocessable claim, and the remittance advice (RA) ...
Does Medicare limit out of network providers?
Medicare does, however, limit the amount providers can bill patients for services. For more information, please refer to Medicare & You 2018 external pdf file. When a patient enrolled in a MA plan uses out-of-network providers, their out of pocket expenses for covered services may be higher.
What is CO 24 Denial Code?
If any patient is already covered under the Medicare advantage plan but in spite of that the claims are submitted to the insurance, then the claims which have been denied can be stated by the CO 24 denial code.
How can the CO 24 Denial Code be resolved?
The steps are listed below that you must follow to resolve the CO24 denial code.
How can one get rid of the CO24 Denial Code?
Wondering how to get rid of the co24 denial code? Well, then here is a list of the things which you could take care of.
When did CMS standardize reason codes?
In 2015 CMS began to standardize the reason codes and statements for certain services. As a result, providers experience more continuity and claim denials are easier to understand.
What does CMS review?
CMS contractors medically review some claims (and prior authorizations) to ensure that payment is billed (or authorization requested) only for services that meet all Medicare rules.