What does PQRS stand for in medical terms?
Physician Quality Reporting System. The Physician Quality Reporting System (PQRS), formerly known as the Physician Quality Reporting Initiative (PQRI), is a health care quality improvement incentive program initiated by the Centers for Medicare and Medicaid Services (CMS) in the United States in 2006.
Is pqrs run by the Medicare administrative contractors?
PQRS is not run by the Medicare Administrative Contractors. The CMS Office of Clinical Standards and Quality administers several quality improvement programs for the agency, including PQRS.
What are PQRS registries?
A number of different vendors have created registries that collect and transmit the data to CMS. PQRS registries must meet criteria set by CMS such as having secure methods for data transmission and providing feedback to registry participants. More information about registry reporting (PDF, 51KB) is available on the CMS website.
Will PQRS reimbursements increase or decrease?
Those providers will lose 1.5% in total reimbursements for CMS patients over the next year, while the 642,000 providers who met PQRS criteria will receive a 0.5% increase in CMS reimbursements. CMS also reported that overall participation grew from 15% in 2007.
What is PQRS Medicare?
The Physician Quality Reporting System (PQRS) was a reporting program of the Centers for Medicare and Medicaid Services (CMS). It gave eligible professionals (EPs) the opportunity to assess the quality of care they were providing to their patients, helping to ensure that patients get the right care at the right time.
What is a PQRS score?
Abstract. Purpose: The performance quality rating scale (PQRS) is an observational measure of performance quality of client-selected, personally meaningful activities. It has been used inconsistently with different scoring systems, and there have been no formal publications on its psychometric properties.
What is PQRS program?
The Physician Quality Reporting Initiative (PQRI) is one of several pay-for-reporting initiatives the Centers for Medicare & Medicaid Services (CMS) is conducting to collect data from health care practitioners about the quality of care furnished to beneficiaries in multiple health care settings.
What is the difference between PQRS and MIPS?
How Is MIPS Different From PQRS? Because MIPS streamlines PQRS, the VM Program and the Medicare EHR Incentive Program, it is more comprehensive and extensive than PQRS alone. MIPS performance is measured by four categories — Quality, Improvement Activities, Promoting Interoperability and Cost.
Why is PQRS important?
Why is PQRS important to you? The program is voluntary, but for those physician practices and individual physicians that do not participate, they will be negatively impacted ECONOMICALLY. They will not be reimbursed at their traditional amounts, and it will impact their ability to keep and hire top physicians.
When did MIPS replace PQRS?
January 1, 2017A new quality program, the Merit-Based Incentive Payment System (MIPS), will replace PQRS on January 1, 2017.
When did PQRS begin?
The Physician Quality Reporting System (PQRS), formerly known as the Physician Quality Reporting Initiative (PQRI), is a health care quality improvement incentive program initiated by the Centers for Medicare and Medicaid Services (CMS) in the United States in 2006.
What is MIPS healthcare?
The Merit-Based Incentive Payment System (MIPS) is the program that will determine Medicare payment adjustments. Using a composite performance score, eligible clinicians (ECs) may receive a payment bonus, a payment penalty or no payment adjustment.
Is Pqrs still a thing?
The Physician Quality Reporting System (PQRS), Medicare's quality reporting program, ended Dec. 31, 2016.
Is MIPS just for Medicare patients?
MIPS reporting of individual measures applies to all patients. Eligibility for a measure is based on CMS documentation (denominator criteria).
What are MIPS requirements?
2022 Low Volume Threshold Participation in MIPS is required if, in both 12-month segments of the MIPS Determination Period if: Excluded individuals or groups must have ≤ $90,000 Part B allowed charges OR ≤ 200 Part B patients OR ≤ 200 covered professional Part B services.
What is PQRS in medical terms?
What is the Physician Quality Reporting System ? Formerly known as the Physician Quality Reporting Initiative (PQRI), the Physician Quality Reporting System (PQRS) was a voluntary reporting program that provided a financial incentive for certain health care professionals, including psychologists, who participated in Medicare to submit data on ...
When did PQRS end?
PQRS ended as a stand-alone program on Dec. 31. 2016; the PQRS quality measures became part of the Merit-based Incentive Payment System (MIPS) in 2017.
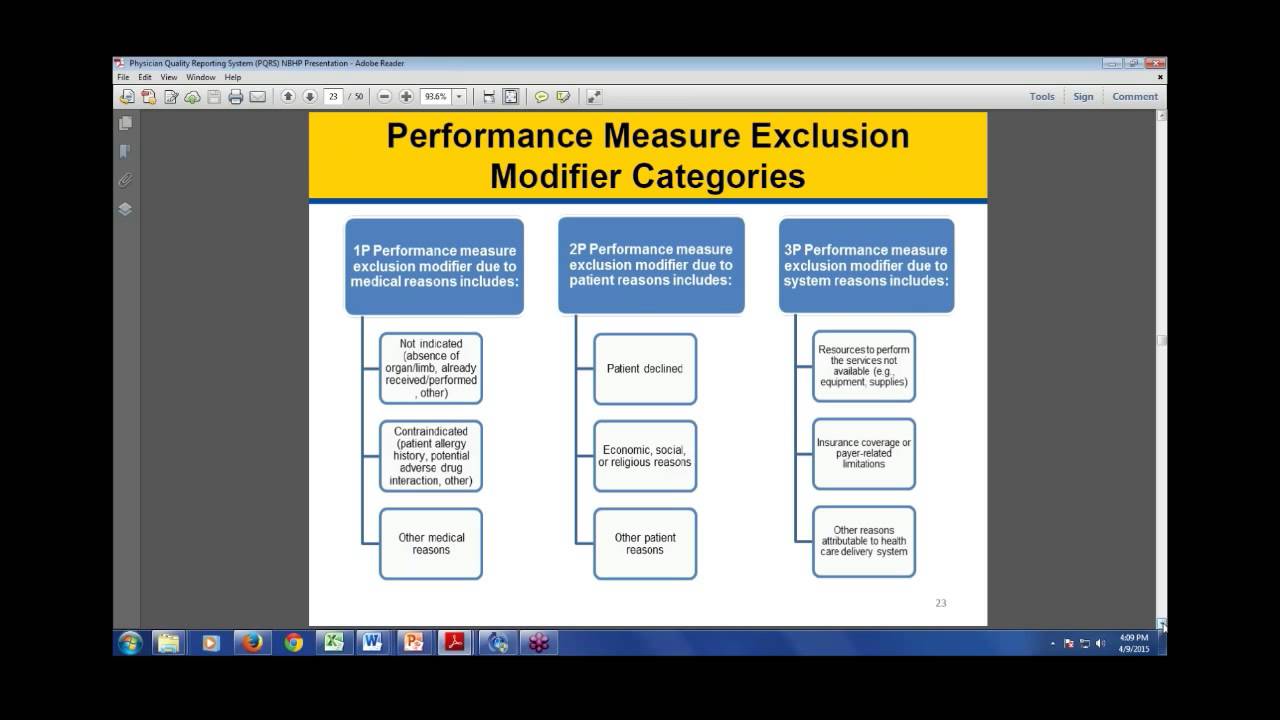
How many measures are required for a psychologist to report?
If a psychologist reports on one to eight measures, or nine measures across fewer than three domains, their claims will automatically be reviewed by CMS under the Measure Validation Process (MAV) so that CMS can determine if additional measures should have been reported.
Is PQRS a Medicare program?
PQRS is not run by the Medica re Administrative Contractors. The CMS Office of Clinical Standards and Quality administers several quality improvement programs for the agency, including PQRS.
Can you report PQRS as an individual?
If the practice has signed up to report under the group reporting option, you cannot choose to separately report PQRS measures as an individual because your National Provider Identification (NPI) number is linked to the TIN used by the group.
What is a PQRS?
Physician Quality Reporting System. The Physician Quality Reporting System (PQRS), formerly known as the Physician Quality Reporting Initiative (PQRI), is a health care quality improvement incentive program initiated by the Centers for Medicare and Medicaid Services (CMS) in the United States in 2006. It is an example of a "pay for performance" ...
When did PQRS become permanent?
It also removed the TRHCA payment cap. The Medicare Improvements for Patients and Providers Act made PQRS permanent in 2008 and increased the incentive payment to 2%. Initially only an incentive program, in 2010 the Affordable Care Act (ACA) introduced penalties for providers who do not submit qualifying PQRS data.
Is PQRS a Medicare incentive?
Because PQRS is a Medicare-based incentive program, only providers who care for patients with Medicare insurance must participate in PQRS. As of 2015, CMS included the following health care practitioners under eligible providers:
Physician Quality Reporting System (PQRS) Overview
The Physician Quality Reporting System (PQRS) has been using incentive payments, and will begin to use payment adjustments in 2015, to encourage eligible health care professionals (EPs) to report on specific quality measures.
Why PQRS
PQRS gives participating EPs the opportunity to assess the quality of care they are providing to their patients, helping to ensure that patients get the right care at the right time. By reporting PQRS quality measures, providers also can quantify how often they are meeting a particular quality metric.
Choosing How to Participate
The program provides an incentive payment to practices with EPs (identified on claims by their individual National Provider Identifier [NPI] and Tax Identification Number [TIN]), or group practices participating in the group practice reporting option (GPRO) who satisfactorily report data on quality measures for covered Physician Fee Schedule (PFS) services furnished to Medicare Part B Fee-for-Service (FFS) beneficiaries (including Railroad Retirement Board and Medicare Secondary Payer)..
Reporting Methods
To participate in the 2014 PQRS program, individual EPs may choose to report quality information through one of the following methods:
Selecting Measures
Quality measures are developed by provider associations, quality groups, and CMS and are used to assign a quantity, based on a standard set by the developers, to the quality of care provided by the EP or group practice.
Incentive Payments
Individual EPs who meet the criteria for satisfactory submission of PQRS quality measures data via one of the reporting mechanisms above for services furnished during the 2014 reporting period will qualify to earn an incentive payment.
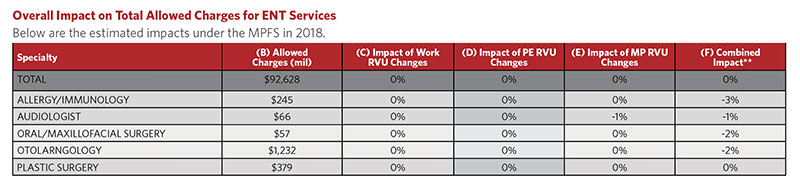
Adjustments
EPs who do not satisfactorily report data on quality measures for covered professional services during the 2014 PQRS program year will be subject to a 2% payment adjustment to their Medicare PFS amount for services provided in 2016.
What is MU in Medicare?
This category replaces the Medicare Electronic Health Record (EHR) Incentive Program for eligible professionals – also known as Meaningful Use (MU). It will account for 25% of your Final Score in 2017. Note: Hospital and Medicaid Meaningful Use are continued.
Do you have to register for a group practice report?
You no longer need to register in advance to report as a group (formerly known as the Group Practice Reporting Option (GPRO), unless you are submitting via the CMS Web-Interface. Under Meaningful Use (MU), there was no option to report as a group, but now providers have that choice.