All Medicare Supplement plans typically cover:
- Your Medicare Part A hospital coinsurance, plus an additional full year of benefits after your Medicare benefits are exhausted
- Some or all of your Medicare Part B coinsurance
- Some or all of your Part A hospice coinsurance
- Some or all of your first three pints of blood
Full Answer
What is the best and cheapest Medicare supplement insurance?
The Medicare Supplement Plan N is best for the following people:
- People looking for complete coverage at a modest monthly rate
- Those who don’t mind paying a minor fee at the time of service
- People who are not subject to Part B excess charges
How much does a Medicare supplement insurance plan cost?
Medicare Supplement Insurance Cost Factors
- Plan Coverage. One big factor in the cost of a Medicare Supplement Insurance plan is the level of coverage provided.
- Carrier. Medicare Supplement Insurance is sold by private insurance companies that set their own plan prices.
- Location. ...
- Enrollment Time. ...
- Pricing Structure. ...
- Discounts. ...
- Gender. ...
How to pick the best Medicare supplement plan?
- Do your important physicians participate in any Medicare Advantage plans or do they only accept Original Medicare?
- What insurance is accepted by your preferred hospitals?
- Do you travel out of the area frequently? ...
- What is your risk tolerance? ...
- How about peace of mind? ...
What is the best Medicare supplement?
Medicare.gov, describes a five star plan as "excellent" saying that the rating system "help you compare plans based on quality and performance." The ratings for plans are completed each year and can very as new plans become available. Those who select a ...

What does Medicare Supplement plan a cover?
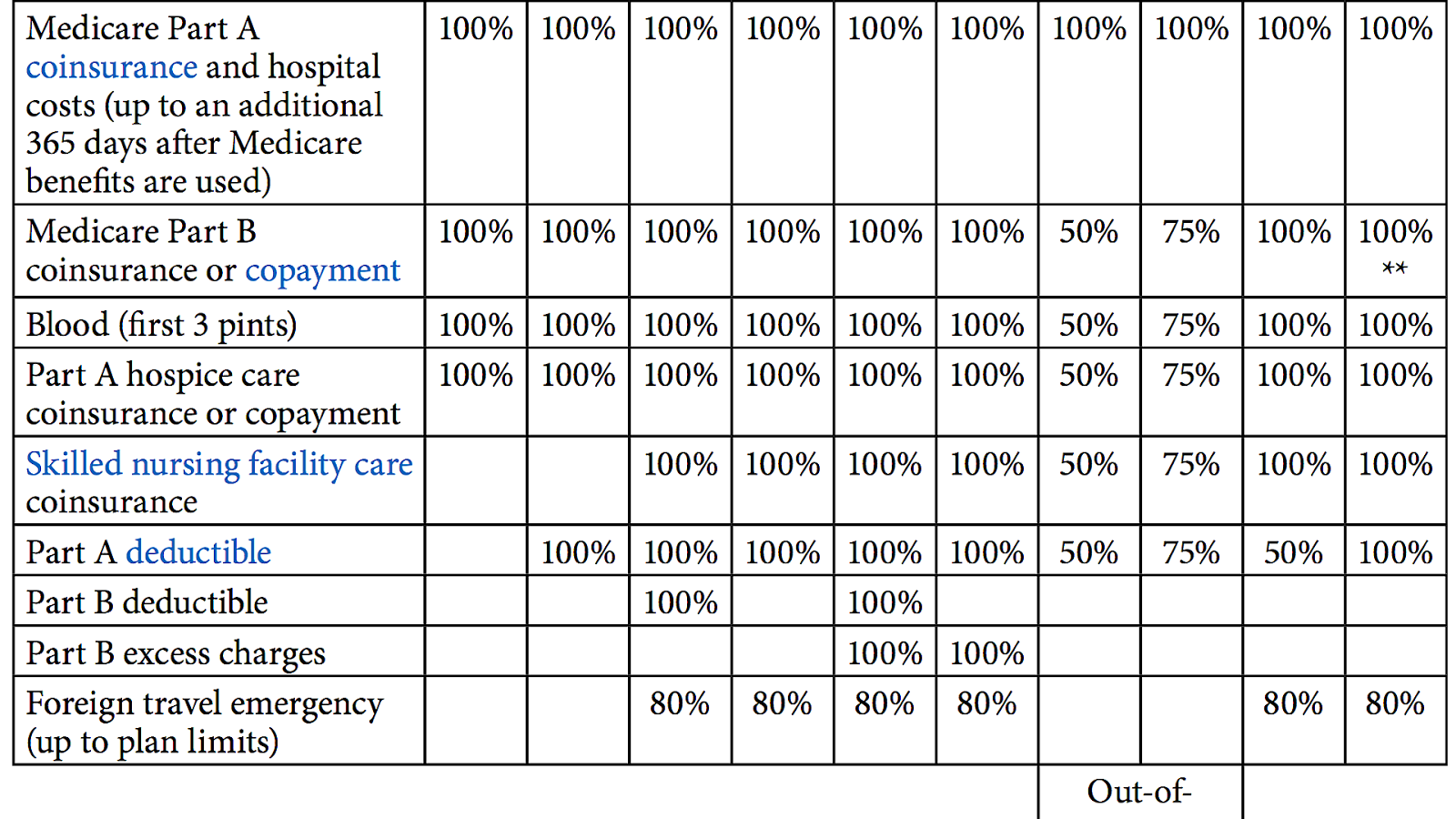
Medicare Supplement insurance Plan A covers 100% of four things: Medicare Part A coinsurance payments for inpatient hospital care up to an additional 365 days after Medicare benefits are used up. Medicare Part B copayment or coinsurance expenses. The first 3 pints of blood used in a medical procedure.
Is there a Medicare Supplement that covers everything?
Medicare Supplement insurance Plan F offers more coverage than any other Medicare Supplement insurance plan. It usually covers everything that Plan G covers as well as: The Medicare Part B deductible at 100% (the Part B deductible is $203 in 2021).
What is the difference between Medicare and a supplemental plan?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Copayments. Coinsurance.
Does Medicare Supplement have benefits?
These are also called Part C plans. Medicare Supplement insurance policies, also called Medigap, help pay the out-of-pocket expenses not covered by Original Medicare (Part A and B). It is not part of the government's Medicare program, but provides coverage in addition to it.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
What will Medicare not pay for?
Generally, Original Medicare does not cover dental work and routine vision or hearing care. Original Medicare won't pay for routine dental care, visits, cleanings, fillings dentures or most tooth extractions. The same holds true for routine vision checks. Eyeglasses and contact lenses aren't generally covered.
What are the advantages and disadvantages of Medicare Supplement plans?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
What does plan G pay for?
Medicare Supplement Plan G covers your percentage of any medical benefit that Original Medicare covers, except for the outpatient deductible. So, it helps to pay for inpatient hospital costs, such as the first three pints of blood, skilled nursing facility care, and hospice care.
Do Medicare Supplement plans cover deductible?
Most Medicare Supplement insurance plans cover the Part A deductible at least 50%. All Medicare Supplement plans also cover your Part A coinsurance and hospital costs 100% for an additional 365 days after your Medicare benefits are used up.
Which of the following is not covered under Part A in Medigap insurance?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
Do Medicare Supplement plans have an out-of-pocket maximum?
Medicare Supplement insurance Plans K and L have out-of-pocket limits that may change from year to year. In 2022, the out-of-pocket limit for Plan K is $6,620 and the limit for Plan L is $3,310. Both plans require you to meet the Part B deductible.
What is coinsurance in Medicare?
Your coinsurance. Hospital costs after you run out of Medicare-covered days. Skilled nursing facility costs after you run out of Medicare-covered days. Here's how it works: You pay a monthly premium for your Medicare supplement plan. These plans are also called Medigap.
What is Medicare Advantage?
Medicare Advantage plans help with your Medicare costs, too. They also offer additional health coverage that Medicare supplement plans don't. The table below breaks down the differences between Medicare supplement plans and Medicare Advantage plans. It might be a good place to start if you're wondering which type of plan is right for you.
What is a Medigap plan?
These plans are also called Medigap. In return, the plan pays most of your out-of-pocket expenses. So when you go to the doctor, for example, you don't have to pay the 20 percent coinsurance required by Medicare. Your Medigap plan pays it for you.
Does Medicare coordinate with Part D?
You coordinate between Medicare, your Medigap plan and your Part D prescription drug plan, if you have one. One company coordinates all your care. Helps pay for costs you have with Original Medicare. Many plans include extra benefits Original Medicare doesn't offer like dental, vision and prescription coverage.
Does Medicare Supplement Plan work?
Medicare supplement plans don't work like most health insurance plans. They don't actually cover any health benefits. Instead, these plans cover the costs you're responsible for with Original Medicare. Hospital costs after you run out of Medicare-covered days.
Is Medicare Supplement a good plan?
A Medicare supplement plan might be a good choice for you if you already have prescription coverage through an employer or military benefits. You can read more about how supplement and Medigap plans work in our help section.
COVERAGE FROM ORIGINAL MEDICARE
Original Medicare, unlike Medicare Supplement insurance, offers basic coverage. It will help cover doctor’s visits, diagnostic testing, at-home physical therapy, and part-time skilled nursing care.
WHAT IS MEDICARE SUPPLEMENT INSURANCE?
Medicare Supplement insurance, which is also called Medigap, is a private insurance that you can purchase in addition to your regular Original Medicare coverage. It covers the copayments, coinsurance, and deductibles that Original Medicare may not, and it may pay for medical expenses you incurred if you traveled outside of the United States.
PURCHASING A MEDICARE SUPPLEMENT INSURANCE PLAN
When you want to purchase a Medicare Supplement insurance plan, you need to do it during open enrollment, which is six months from the first day of the month of your 65th birthday. You also need to make sure you signed up for Medicare Part B within those same six months.
What is Medicare Supplement Insurance?
Medicare Supplement insurance is meant to limit unpleasant surprises from healthcare costs. Your health at age 65 may be no indicator of what’s to come just a few years later. You could get sick and face medical bills that devastate years of planning and preparation. Combine this with the fixed income that so many seniors find themselves on, ...
How much does Medicare Supplement cover?
Choosing Medicare Supplement insurance can help. It can cover up to 100% of out-of-pocket costs, depending on the plan. One out of every three Original Medicare beneficiaries — over 13 million seniors — have chosen to do so. 1.
How long is the open enrollment period for Medicare?
The Medigap Open Enrollment Period covers six months. It starts the month you are 65 or older and are enrolled in Medicare Part B. In this period, no insurer offering supplemental insurance in your state can deny you coverage or raise the premium because of medical conditions.
How many separate insurance plans are there?
Premiums for the same policy can vary between insurance companies. But, only the quoted price and the reputation of the insurer will vary. There are ten separate plans, labeled A through N. Two plans, C and F, are no longer offered to newly eligible beneficiaries.
What is Part B deductible?
After that, you pay daily coinsurance amounts, depending on the length of your stay. Part B also has an annual deductible. Once you reach it, Part B covers 80% of eligible doctor-related, testing and medical-equipment expenses. You are responsible for the balance (or coinsurance).
Does Medicare Supplement cover all costs?
Original Medicare does not cover all costs. Medicare Supplement insurance, or Medigap, can cover what Medicare does not. Private insurance companies – vetted by the federal government – offer it to help manage out-of-pocket expenses. These policies do not add coverage.
Can you renew a Medigap policy?
You can renew your Medigap policy as long as you pay the premium. The insurer cannot use your health problems to cancel your policy or raise your premium.
What is Medicare Supplement?
Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance. For many people, Medicare Supplement, also known as Medigap, insurance helps them economically by paying some of the out-of-pocket costs associated with Original Medicare.
How many people does Medicare Supplement cover?
Keep in mind that, just like Medicare, Medicare Supplement plans are individual insurance policies. They only cover one person per plan. If you want coverage for your spouse, you must purchase a separate plan.
What percentage of Medicare supplement is paid?
After this is paid, your supplement policy pays your portion of the remaining cost. This is generally 20 percent. Some policies pay your deductibles The deductible is a set amount which you must pay before Medicare begins covering your health care costs.
How long does Medicare cover travel?
Each plan varies in what it covers, but all plans pay for Medicare Part A (hospital insurance) coinsurances for up to 365 days beyond the coverage that Medicare offers. Some of the plans cover a percentage of the cost for emergency health care while traveling abroad.
How old do you have to be to qualify for medicare?
To be eligible for Medicare, you must be at least 65 years old, a citizen of the United States or permanent legal resident for at least five consecutive years. Also, you, or your spouse, must have worked and paid federal taxes for at least ten years (or 40 quarters).
Does Medicare cover long term care?
Most plans do not cover long-term care, vision, dental, hearing care, or private nursing care. All Medicare Supplement insurance coverage comes with a monthly premium which you pay directly to your provider. How much you pay depends on which plan you have.
Does Medicare Supplement pay for coinsurance?
Most supplement plans pay for Medicare copayments, coinsurance, and deductibles. But the coverage may vary according to the plan you choose. Medicare Supplement plans work together with Original Medicare. First, Medicare pays for a percentage, usually 80 percent, of the Medicare-approved cost of your health care service.
What is supplemental insurance?
Supplemental insurance is any policy that you have in addition to your main health insurance coverage.
Cost of supplemental insurance
Supplemental policies are less expensive than regular insurance because they provide supplemental coverage, not comprehensive coverage.
Why should you buy supplemental plans?
Supplemental policies serve a dual purpose of limiting how much you pay for health care while also helping to protect your finances.
Types of supplemental insurance
Below are descriptions of some of the most popular supplemental plans and what to consider when shopping for coverage.
Frequently asked questions
Supplemental insurance is an add-on to your regular insurance that provides an extra level of coverage, helping you to meet out-of-pocket costs and other expenses not covered by your regular insurance.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
Medigap and Assisted Living
Medigap plans exist to help Medicare beneficiaries pay for services that Original Medicare leaves uncovered. Vision, dental and some prescription drugs are typically included in most Medicare supplemental policies.
Paying for Assisted Living
Medicare and Medigap are not the only resources available for seniors who need help with the cost of residential care. Seniors with limited income and assets often choose Medicaid as their Medicare supplement.
