MACs send claim adjudication and payment information to providers, suppliers, and billers using an Electronic Remittance Advice (ERA) or a Standard Paper Remittance (SPR) along with payments. These RAs give explanations and guidance as to whether Medicare made a payment on a claim and if the payment differs from what the provider submitted. The ERA or SPR conveys itemized information for each claim and/or service line enabling the provider to associate the adjudication decisions with those submitted claims/lines. The ERA or SPR, reports the reason and the value of each adjustment. Adjustments can happen at the claim, service line, or provider level.
Full Answer
What is an RA remark code?
Each RA remark code identifies a specific message as shown in RA remark code list Qualified Medicare Beneficiary (QMB) Program - View QMB program information and related remit advice remark codes. Reason Code Guidance - View common claim submission error codes, a description of issue and potential solutions
What is the difference between the original claim and adjusted claim?
For claim adjustments where payment was made to the provider on the original and the adjusted claim, this amount will be the lower paid amount of the original claim or the adjusted claim. The Medicare ID on the original claim will display with the Financial Control Number (FCN).
What does the allowed amount mean on a Medicare claim?
The allowed amount represents the Medicare reimbursement rate for the specific service billed. This field displays the amount of any deductible applied to the claim. The patient is responsible for this amount.
How do I know what type of claim or adjustment I received?
The first two digits of the Internal Control Number that appear on your payment listing will show the type of claim or claim adjustment. The next two digits of the ICN will show the two-digit year the claim was received, or the adjustment was initiated.
What information can be found on the RA from Medicare?
The RA provides not only payment information, but also information about adjustments, denials, missing information, refunds, and offsets.
What is a claim RA?
WHAT IS AN RA? The Remittance Advice (RA) contains information about your claim payments that Medicare Administrative Contractors (MACs) send, along with the payments, to providers, physicians, and suppliers. The RA, which may either be in the form of an Electronic Remittance Advice (ERA) or a Standard Paper.
What does MOA mean on an EOB?
MOA. Medicare Outpatient Adjudication (MOA) remark codes are used to convey appeal information and other claim-specific information that does not involve a financial adjustment.
How do you read a remittance report?
1:1228:46How to Read the Remittance Advice - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe basics of a remittance advice is to include the a35 transaction is to communicate the claimMoreThe basics of a remittance advice is to include the a35 transaction is to communicate the claim submitters. The reasons why build services are paid or denied. Both the current paper remit.
What is the difference between an RA and an EOB?
Difference of Recipient Both types of statements provide an explanation of benefits, but the remittance advice is provided directly to the health-care provider, whereas the explanation of benefits statement is sent to insured patient, according to Louisiana Department of Health.
What does forwarding balance mean on EOB?
"Forwarding balance" means that a negative value represents a balance moving forward to a future payment advice. A positive value represents a balance being applied from a previous Remittance Advice (RA). A reference number (the original ICN and the patient's Medicare ID number) is applied for tracking purposes.
How do you explain Explanation of Benefits?
An EOB is a statement from your health insurance plan describing what costs it will cover for medical care or products you've received. The EOB is generated when your provider submits a claim for the services you received. The insurance company sends you EOBs to help make clear: The cost of the care you received.
What do you do with Explanation of Benefits?
What should you do with an EOB? You should always save your Explanation of Benefits forms until you get the final bill from your doctor or health care provider. Compare the amount you owe on the EOB to the amount on the bill. If they match, that's the amount you'll need to pay.
What information is found on the Explanation of Benefits EOB?
After you visit your provider, you may receive an Explanations of Benefits (EOB) from your insurer. This is an overview of the total charges for your visit and how much you and your health plan will have to pay. An EOB is NOT A BILL and helps to make sure that only you and your family are using your coverage.
Is a claim that is automatically forwarded from Medicare to a secondary insurer after Medicare has paid its portion of a service in the EHR?
A claim that is automatically forwarded from Medicare to a secondary insurer after Medicare has paid its portion of a service when using an EHR is known as: crossover.
What is a claim payment remittance advice and check?
An electronic remittance advice, or ERA, is an explanation from a health plan to a provider about a claim payment. An ERA explains how a health plan has adjusted claim charges based on factors like: Contract agreements. Secondary payers. Benefit coverage.
Why did I get a remittance advice check?
Remittance advice is used by a customer to inform the supplier about a payment status. It contains important information such as the payment amount and what invoice numbers the payment is tendered. If an invoice is paid by check, it's common to attach a paper remittance advice to the check.
What is a RA in insurance?
Providers use the RA to post payments and to review claim adjustments. The RA also contains detailed and specific claim decision information. An adjustment may be made for any number of reasons. These reasons are identified on the RA through standardized code sets which include Group Codes, Claim Adjustment Reason Codes, and RA Remark Codes.
How does ERA help with Medicare?
Using the ERA saves time and increases productivity by providing electronic payment adjustment information that is portable, reusable, retrievable , and storable. The ERA can be exchanged between partners with much greater ease than a paper remittance. Advantages to using the ERA include:•Faster communication and payment notification•Faster account reconciliation through electronic posting•Less paper generated•Lower operating costs•More detailed information•Access to data in a variety of formats through free, Medicare-supported software
What is the ERA for Medicare?
A provider may receive an RA from Medicare transmitted in an electronic format, called the Electronic Remittance Advice (ERA), or in a paper format, called the Standard Paper Remittance Advice (SPR).
What is a remittance advice?
WhAt Is An RA? A Remittance Advice (RA) is a notice of payments and adjustments sent to providers, billers, and suppliers. After a claim has been received and processed, a Medicare contractor produces the RA, which may serve as a companion to a claim payment (s) or as an explanation when there is no payment.
What is a Medicare specific remark code?
Medicare-Specific Remark Codes - Convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a claim adjustment reason code. Each RA remark code identifies a specific message as shown in RA remark code list
What is a reason code?
Reason Codes - Explain why a claim was not paid or how claim was paid and provides reason for any claim financial adjustments, such as denials, reductions or increases in payment
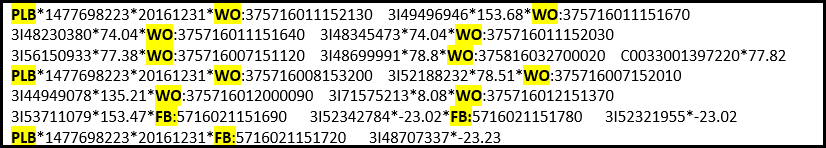
What is a FB on a Medicare claim?
The "Payment Summary" page of the remittance advice (RA)/electronic remittance advice (ERA) may include a list of forward balances (FB) at the claim level. A FB occurs when a payment is recouped on a current or on a future RA/ERA, but the reimbursement amount is not enough to recover the recouped amount. The FB amount is the balance of what still needs to be recouped. For example, if the amount of $5000.00 needs to be recouped, but the total reimbursement made was only $3000.00, the remaining amount of $2000.00 will display as a FB on the "Payment Summary" page. The FB amount will then be recouped on future RAs/ERAs until it reaches a zero balance. The FB shown on the "Payment Summary" page identifies the document control number (DCN) and the Medicare ID number of the claim which created the FB.
How many columns are there in the payment summary page?
Note that the "Payment Summary" page will display three sets of columns. The following is an example of just one column.
What is an ERA in Medicare?
After the Fiscal Intermediary Standard System (FISS) completes processing your Medicare claim, either an RA (also known as a Standard Paper Remittance (SPR)), or an ERA (also known as an Electronic Remittance Notice (ERN)) is provided with final claim adjudication and payment information. It is recommended that providers accept ERA transmissions in lieu of mailed SPRs. The ERA contains all information found on the SPRs, as well as additional information not available on an SPR.
How much does it cost to get a duplicate RA?
There is a charge of $15.00 for each duplicate remittance advice (electronic or paper) requested. Requests will be completed within 45 business days of receipt and mailed to the remittance advice address on the Fiscal Intermediary Standard System (FISS) provider file.
What is an ERA on a SPR?
The ERA contains all information found on the SPRs, as well as additional information not available on an SPR. All ERAs are sent in the X12 835 transaction. The free software, PCPrint, is available for providers to read and print the ERA.
What Is An RA?
- A Remittance Advice (RA) is a notice of payments and adjustments sent to providers, billers, and suppliers. After a claim has been received and processed, a Medicare contractor produces the RA, which may serve as a companion to a claim payment(s) or as an explanation when there is no payment. The RA explains the reimbursement decisions including th...
What Are The Uses For The RA?
- Providers use the RA to post payments and to review claim adjustments. The RA also contains detailed and specific claim decision information. An adjustment may be made for any number of reasons. These reasons are identified on the RA through standardized code sets which include Group Codes, Claim Adjustment Reason Codes, and RA Remark Codes.
What Are The Different Types of RAS?
- A provider may receive an RA from Medicare transmitted in an electronic format, called the Electronic Remittance Advice (ERA), or in a paper format, called the Standard Paper Remittance Advice (SPR). Although the information featured on the ERA and SPR is similar, the two formats are arranged differently, and the ERA offers some data and administrative efficiencies not availa…
The Importance of The Era
- The ERA must be produced in the current Health Insurance Portability and Accountability Act of 1996 (HIPAA)-compliant Accredited Standards Committee (ASC) X12N 835 004010A1 format. The Secretary of the Department of Health & Human Services (DHHS) adopted ASC X12N 835 version 004010 as the standard for ERA in August 2000. In February 2003, an addendum was ad…
Why Receive The Era?
- Using the ERA saves time and increases productivity by providing electronic payment adjustment information that is portable, reusable, retrievable, and storable. The ERA can be exchanged between partners with much greater ease than a paper remittance. Advantages to using the ERA include:•Faster communication and payment notification•Faster account reconciliation through …