Diagnostic tests like a urinalysis are typically covered under Medicare Part B. In order to qualify for Medicare Part B coverage, a urinalysis must be deemed as medically necessary and ordered by an approved physician.
Full Answer
Does Medicare cover a urinalysis?
Diagnostic tests like a urinalysis are typically covered under Medicare Part B. In order to qualify for Medicare Part B coverage, a urinalysis must be deemed as medically necessary and ordered by an approved physician.
What is the CPT code for Welcome to Medicare exam?
G0402 is the “Welcome to Medicare Exam” which is basically a routine physical which can only be done in the first 12 months the patient becomes eligible for Medicare. G0438 is the code for the first, initial, Annual Wellness Visit. All subsequent AWVs are billed using G0439.
Does Medicare cover DME?
Medicare Part B (Medical Insurance) covers Medically necessary DME if your doctor prescribes it for use in your home. DME that Medicare covers includes, but isn't limited to: Blood sugar meters Blood sugar test strips; Canes Commode chairs; Continuous passive motion devices Continuous Positive Airway Pressure (CPAP) devices; Crutches; Hospital beds
What is the CPT code for routine general exam for diabetes?
Diagnosis Code: Z00.00 (Routine General Exam), E11.9 (Diabetes), I10 (Hypertension), E78.5 (Hyperlipidemia) 2. CPT Code: 99213 (Established Patient Office Visit) – Modifier 25 Diagnosis Code: E11.9 (Diabetes), I10 (Hypertension), E78.5 (Hyperlipidemia)
What is the ICD 10 code for urine drug screening?
ICD-10-CM Codes that Support Medical Necessity For monitoring of patient compliance in a drug treatment program, use diagnosis code Z03. 89 as the primary diagnosis and the specific drug dependence diagnosis as the secondary diagnosis.
Is urine Drug test covered by Medicare?
Medicare also covers clinical laboratory services, including urine drug testing (UDT), under Part B. Physicians use UDT to detect the presence or absence of drugs or to identify specific drugs in urine samples.
How do you code a urine drug screen?
Overview and Clinical Utility: In order to match our testing method that is currently being performed, urine drug screen analysis will be billed using CPT code 80101 for each drug class.
What is the code for a Drug test?
Providers are required to use procedure codes 80305–80307, G0480–G0483, and G0659 when submitting claims for testing for drugs of abuse. Providers should use procedure codes 80305–80307 when submitting claims for presumptive drug tests.
Why does Medicare not pay for urinalysis?
Urine screenings for employment and other non-medical reasons would not be eligible for coverage under Medicare benefits. With Medicare Part B coverage, most medically necessary diagnostic tests do not require copays or coinsurances. Part A benefits cover diagnostic tests for inpatient hospital stays.
Does Medicare pay for CPT code 80305?
The AMA CPT code for drug testing using our 12 panel drug test cups, which is the code used for Medicare B and most other insurers, is 80305.
Can you bill for urine collection?
Physician laboratories may charge for specimen collection only when (a) it is accepted and prevailing practice among physicians in the locality to make a separate charge for drawing or collecting a specimen, and (b) it is the customary practice of the physician performing such a service to bill separately for specimen ...
What is diagnosis code Z51 81?
ICD-10 code Z51. 81 for Encounter for therapeutic drug level monitoring is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is diagnosis code Z03 89?
Z03. 89 No diagnosis This diagnosis description is CHANGED from “No Diagnosis” to “Encounter for observation for other suspected diseases and conditions ruled out.” established. October 1, 2019, with the 2020 edition of ICD-10-CM.
What is the difference between a presumptive and definitive test?
1. Definitive/Quantitative testing is considered medically necessary only in those instances when the results of the initial urine drug testing (Presumptive/Qualitative testing) require information that may result in a change in the evaluation and/or treatment of patients.
What's in a 12 panel Drug test?
Standard 12-panel test: looks for cocaine, marijuana, PCP, amphetamines, opiates, benzodiazepines, barbiturates, methadone, propoxyphene, Quaaludes, Ecstasy/MDA, & Oxycodone/Percoset.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
The billing and coding information in this article is dependent on the coverage indications, limitations and/or medical necessity described in the related LCD L34645 Drug Testing.
ICD-10-CM Codes that Support Medical Necessity
For monitoring of patient compliance in a drug treatment program, use diagnosis code Z03.89 as the primary diagnosis and the specific drug dependence diagnosis as the secondary diagnosis.
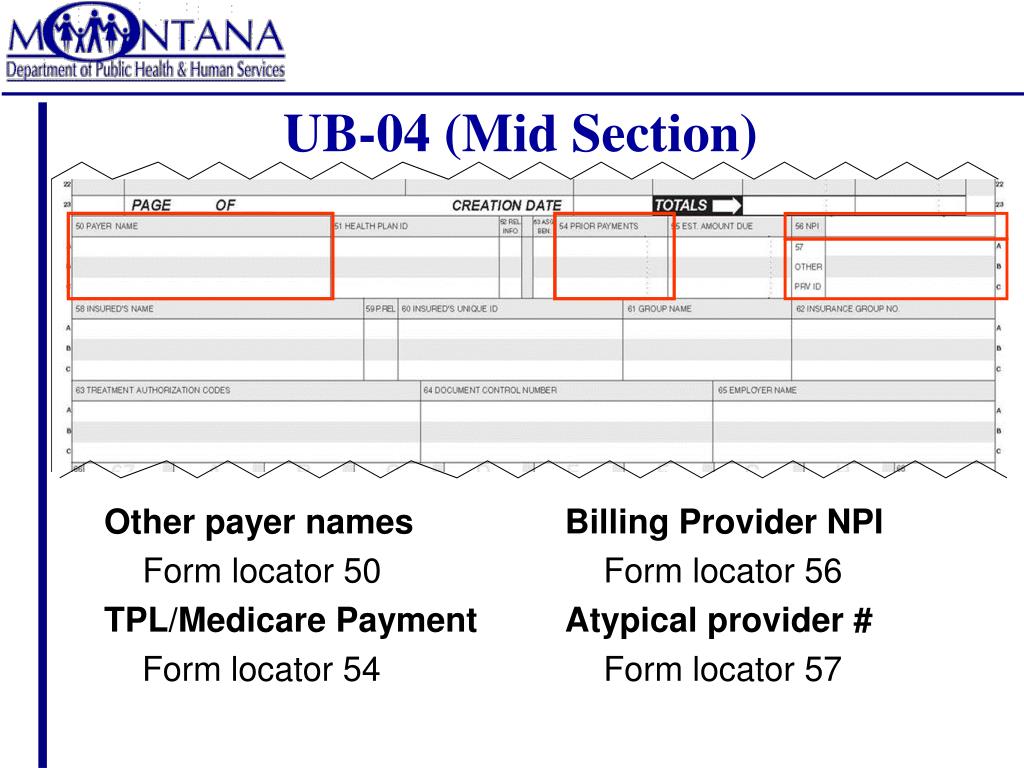
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
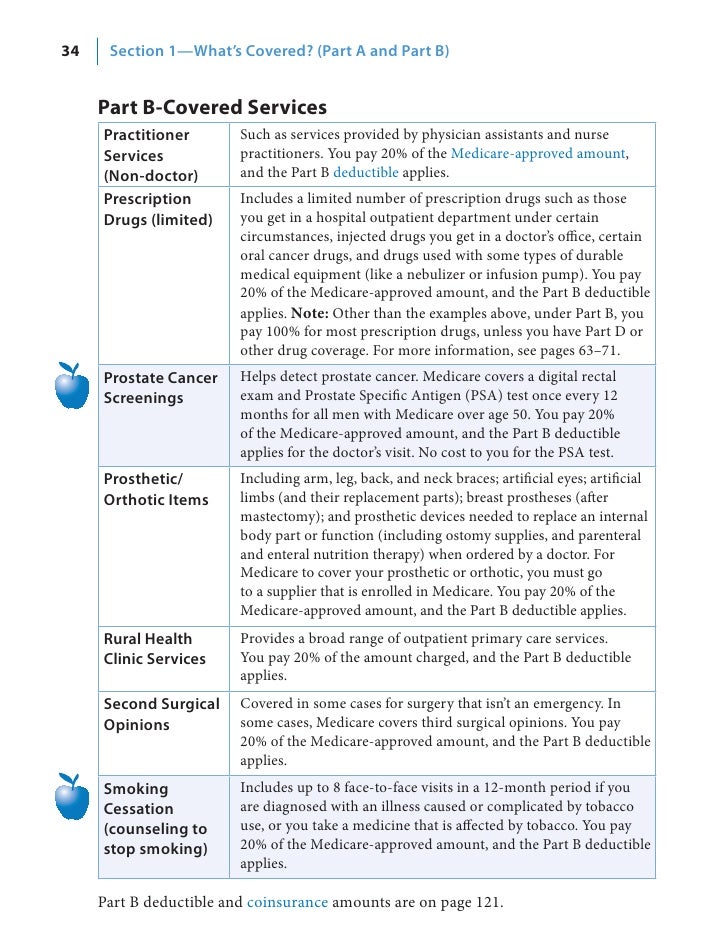
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. you pay 20% of the. Medicare-Approved Amount.
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
What is the HCPCS code for a wellness visit?
This exam is billed using HCPCS code G0402. An Annual Wellness Visit code of G0438 should not be used — and will be denied — because the patient is eligible for the Welcome to Medicare visit during the first year of enrollment. For more information on the Welcome to Medicare visit go-to CMS.
Is 99397 covered by Medicare?
Preventative Medicine codes 99387 and 99397, better known to offices as Complete Physical Exams or Well Checks for 65 and older, still remain a non-covered, routine service from Medicare. The Well Woman Exam codes G0101 and Q0091 are covered services.