Who pays first – Medicare or group health?
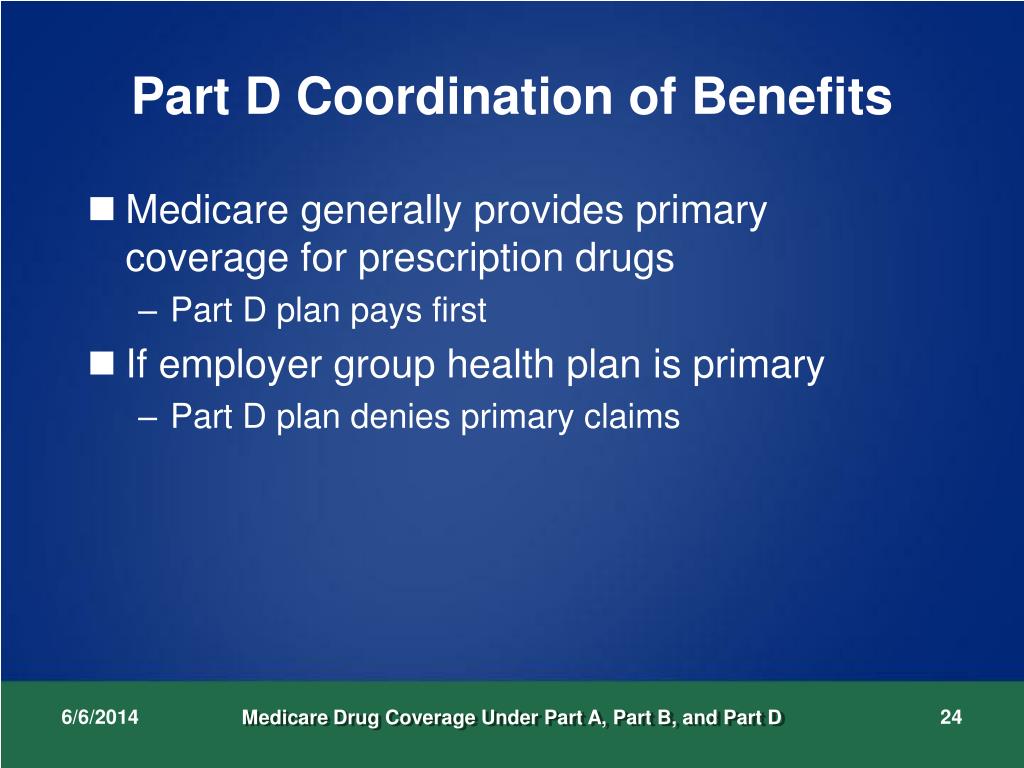
After the coordination period, Medicare pays first and the group health plan (or retiree coverage) pays second. If you originally got Medicare due to your age or a disability other than ESRD, and your group health plan was your primary payer, then it still pays first when you become eligible because of ESRD.
How does Medicare work with my health insurance?
If Medicare is primary, it means that Medicare will pay any health expenses first. Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs.
Do employers have to pay for Medicare?
You must be the one to pay Medicare. However, employers can pay Medicare premiums for active employees if the company’s payment plan is integrated with the group’s health plan. For example, the linked group plan must provide minimum value by paying for at least 60 percent of the actuarial value of services received.
Do you have to pay for Medicare if you have group health?
You'll have to pay any costs Medicare or the group health plan doesn't cover. Employers with 20 or more employees must offer current employees 65 and older the same health benefits, under the same conditions, that they offer employees under 65.
Who is Medicare funded by?
Funding for Medicare, which totaled $888 billion in 2021, comes primarily from general revenues, payroll tax revenues, and premiums paid by beneficiaries (Figure 1). Other sources include taxes on Social Security benefits, payments from states, and interest.
Is Medicare financed by corporations?
The Medicare program is primarily funded through a combination of payroll taxes, general revenues and premiums paid by beneficiaries. Other sources of revenues include taxes on Social Security benefits, payments from states and interest on payments and investments.
Is Medicare paid for by taxpayers?
Funding for Medicare is done through payroll taxes and premiums paid by recipients. Medicaid is funded by the federal government and each state.
How is Medicare Part A primarily funded?
How is Medicare Part A funded? Medicare Part A (hospital insurance) is paid through the HI Trust Fund. The fund primarily comprises revenue from the Medicare tax.
How is Medicare funded in America?
Medicare is primarily funded through the Federal Insurance Contributions Act (FICA). Taxes from FICA contribute to two trust funds that cover Medicare expenditures. The Medicare Hospital Insurance (HI) trust fund covers Medicare Part A costs.
Is Medicare funded by private insurance companies?
Medicare is funded through a mix of general revenue and the Medicare levy. The Medicare levy is currently set at 1.5% of taxable income with an additional surcharge of 1% for high-income earners without private health insurance cover.
How is Medicare funded by paid taxes quizlet?
How is Medicare funded? Partially funded by federal government through tax dollars. -The rest is funded by premiums, deductibles and coninsurance payments.
Who pays for Medicaid?
The Medicaid program is jointly funded by the federal government and states. The federal government pays states for a specified percentage of program expenditures, called the Federal Medical Assistance Percentage (FMAP).
Is Medicare paid for by the government?
Medicare is an insurance program. Medical bills are paid from trust funds which those covered have paid into. It serves people over 65 primarily, whatever their income; and serves younger disabled people and dialysis patients.
Is CMS a federal agency?
The federal agency that runs the Medicare, Medicaid, and Children's Health Insurance Programs, and the federally facilitated Marketplace. For more information, visit cms.gov.
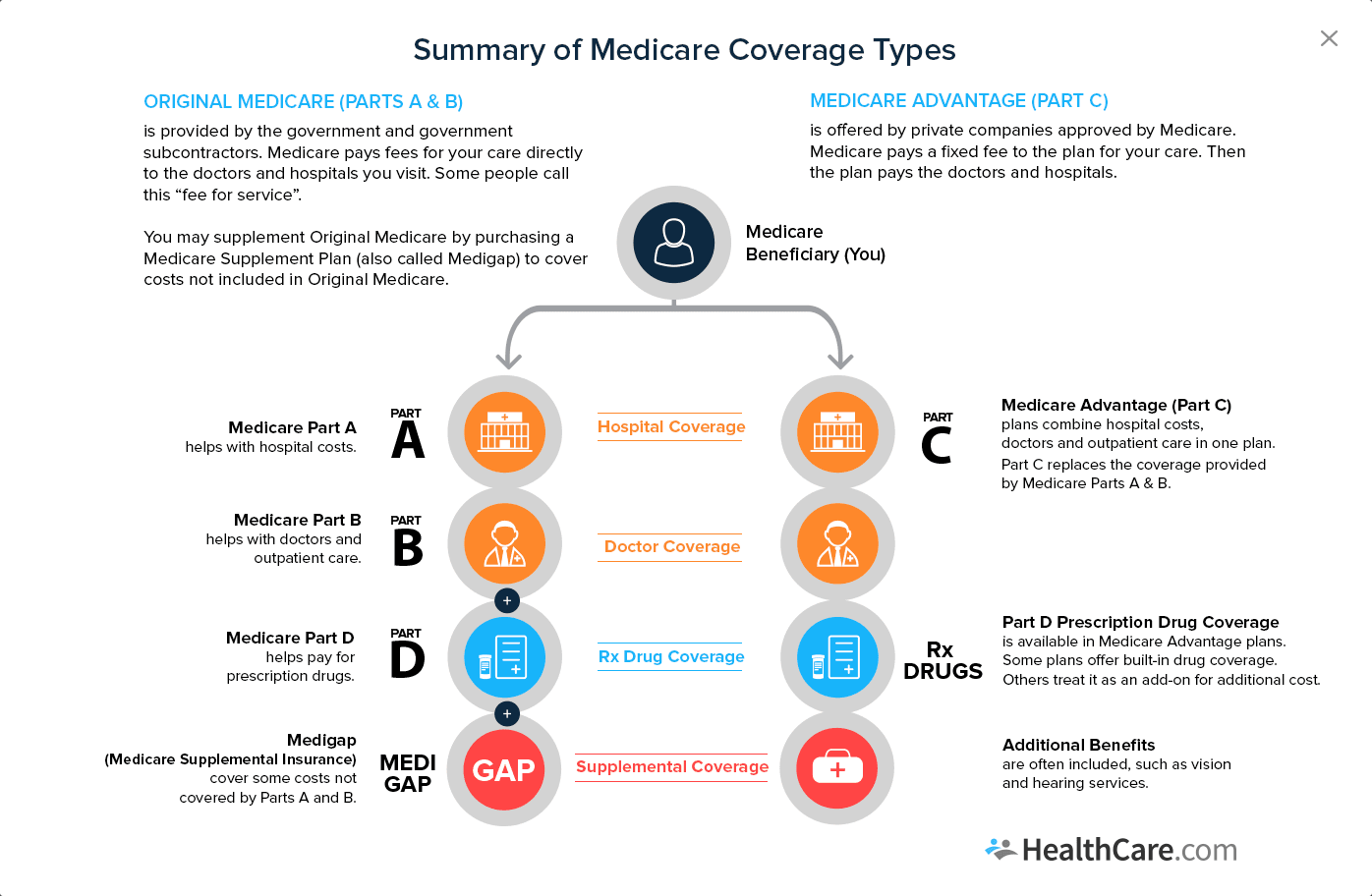
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What are the responsibilities of an employer under MSP?
As an employer, you must: Ensure that your plans identify those individuals to whom the MSP requirement applies; Ensure that your plans provide for proper primary payments whereby law Medicare is the secondary payer; and.
What is the purpose of MSP?
The MSP provisions have protected Medicare Trust Funds by ensuring that Medicare does not pay for items and services that certain health insurance or coverage is primarily responsible for paying. The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage.
What age does GHP pay?
Individual is age 65 or older, is covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, ...
What is Medicare Secondary Payer?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer. This booklet gives an overview of the MSP provisions and explains your responsibilities in detail.
Why does Medicare make a conditional payment?
Medicare may make pending case conditional payments to avoid imposing a financial hardship on you and the patient while awaiting a contested case decision.
What is a COB in health insurance?
Coordination of Benefits (COB) allows plans to determine their payment responsibilities. The BCRC collects, manages, and uploads information to the Common Working File (CWF) about patients’ other health insurance coverage. Providers, physicians, and other suppliers must collect accurate MSP patient information to ensure that claims are filed properly.
What happens if you don't file a claim with the primary payer?
File proper and timely claims with the primary payer. Not filing proper and timely claims with the primary payer may result in claim denial. Policies vary depending on the payer; check with the payer to learn its specific policies.
Can Medicare make a payment?
Medicare can’t make payment when payment “has been made or can reasonably be expected to be made” under liability insurance (including self-insurance), no-fault insurance, or a WC law or plan of the United States, called a primary plan.
Can Medicare deny a claim?
Medicare may mistakenly pay a claim as primary if it meets all billing requirements, including coverage and medical necessity guidelines . However, if the patient’s CWF MSP record shows another insurer should pay primary to Medicare, we deny the claim.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
Can CMS issue more than one demand letter?
For ORM, there may be multiple recoveries to account for the period of ORM, which means that CMS may issue more than one demand letter. When Medicare is notified of a settlement, judgment, award, or other payment, including ORM, the recovery contractor will perform a search of Medicare paid claims history.
How does Medicare reimbursement work?
A Medicare premium reimbursement is a fantastic way for active employees to get refunds of their premiums. Often, premiums may cost less than group insurance at your workplace. If you prefer Medicare to your group coverage, you may be eligible to get premium reimbursements.
What does MEC mean for Medicare?
This type of arrangement can help reimburse employees for their Medicare premiums. If an employee holds minimum essential coverage (MEC), they can get assistance in paying for virtually all Medicare costs, including Medigap premiums.
What is ICHRA insurance?
Individual Coverage Health Reimbursement Arrangement (ICHRA) To be eligible for an Individual Coverage Health Reimbursement Arrangement, you’ll need Part A and Part B, or Part C. You can use the ICHRA to reimburse premiums for Medicare and Medigap as well as other costs. Employers have more choice in which medical costs are eligible ...
What is a health reimbursement arrangement?
A Health Reimbursement Arrangement is a system covered by Section 105. This arrangement allows your employer to reimburse you for your premiums. Some HRAs at employers that provide group coverage require that your employer’s payment plan ties in with the group health plan. Contact a human resources representative at your organization ...
What is Section 105?
Although there are several different plan options, the most popular Section 105 program is a Health Reimbursement Arrangement plan.
Can my employer pay my Medicare premiums in 2021?
Updated on July 13, 2021. While your employer can’t pay your Medicare premiums in the true sense, you’ll be glad to know that they may reimburse you for your premium costs! To compensate you, your employer will need to create a Section 105 Medical Reimbursement Plan. We’re here to help you understand your options for reimbursement ...
Is a Section 105 reimbursement taxable?
Some Section 105 plans may only permit refunds on healthcare costs and premiums. This compensation isn’t taxable. If the Section 105 plan reimburses with cash for any remaining benefits, both the money and reimbursements are taxable.answer.
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
What is a small group health plan?
Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage a small group health plan. If your employer’s insurance covers more than 20 employees, Medicare will pay secondary and call your work-related coverage a Group Health Plan (GHP).
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Does Cobra pay for primary?
The only exception to this rule is if you have End-Stage Renal Disease and COBRA will pay primary. Your COBRA coverage typically ends once you enroll in Medicare. However, you could potentially get an extension of the COBRA if Medicare doesn’t cover everything the COBRA plan does like dental or vision insurance.
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The BCRC takes actions to identify the health benefits available to a Medicare beneficiary and coordinates the payment process to prevent mistaken payment ...
Who is responsible for pursuing recovery from a liability insurer?
The CRC is responsible for pursuing recovery directly from a liability insurer (including a self-insured entity), no-fault insurer or workers’ compensation entity. For more information on the processes used by the CRC to recover conditional payments, see the Insurer NGHP Recovery page.
Medicare’s Demand Letter
- In general, CMS issues the demand letter directly to: 1. The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. 2. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals ...
Assessment of Interest and Failure to Respond
- Interest accrues from the date of the demand letter, but is only assessed if the debt is not repaid or otherwise resolved within the time period specified in the recovery demand letter. Interest is due and payable for each full 30-day period the debt remains unresolved; payments are applied to interest first and then to the principal. Interest is assessed on unpaid debts even if a debtor is pu…
Right to Appeal
- It is important to note that the individual or entity that receives the demand letter seeking repayment directly from that individual or entity is able to request an appeal. This means that if the demand letter is directed to the beneficiary, the beneficiary has the right to appeal. If the demand letter is directed to the liability insurer, no-fault insurer or WC entity, that entity has the ri…
Waiver of Recovery
- The beneficiary has the right to request that the Medicare program waive recovery of the demand amount owed in full or in part. The right to request a waiver of recovery is separate from the right to appeal the demand letter, and both a waiver of recovery and an appeal may be requested at the same time. The Medicare program may waive recovery of the amount owed if the following con…