What medical equipment is covered by Medicare?
Dec 02, 2021 · Medicare covers a wide variety of durable medical equipment. Covered items include (but are not limited to): Blood sugar monitors and test strips Canes, crutches, and walkers Commode chairs Hospital beds Infusion pumps and supplies Manual wheelchairs and power mobility devices (wheelchairs and scooters) when required inside the home
Is durable equipment covered by Medicare?
Generally, Medicare will also cover the cost of loaned equipment for items (like wheelchairs) during the time your equipment is being repaired. If you’re in a Medicare Advantage Plan or other Medicare health plan,
What medical supplies are covered by Medicaid?
En español | Medicare Part B helps to pay for many items of medical equipment and supplies that help you function — for example, wheelchairs, artificial limbs, pacemakers, commode chairs, hospital beds, appliances to help breathing, neck and back braces, oxygen supplies and many more. The equipment must be durable (long-lasting).
Does Medicare cover DME equipment?
What items will Medicare pay for?
DME that Medicare covers includes, but isn't limited to:Blood sugar meters.Blood sugar test strips.Canes.Commode chairs.Continuous passive motion devices.Continuous Positive Airway Pressure (CPAP) devices.Crutches.Hospital beds.More items...
Does Medicare pay for walkers and shower chairs?
A: Yes. Medicare Part B covers a portion of the cost for medically-necessary wheelchairs, walkers and other in-home medical equipment. (Medicare will not cover power wheelchairs that are only needed for use outside the home.) Talk with your doctor about your needs.
What equipment does Medicare cover for knee replacement?
knee CPM machinescovers knee CPM machines as durable medical equipment (DME) that your doctor prescribes for use in your home. For example, if you have knee replacement surgery, Medicare covers CPM devices for up to 21 days of use in your home.
Does Medicare pay for personal items?
With only a few exceptions, Medicare doesn't cover disposable items. To qualify for Medicare coverage, the equipment or supplies must be: Medically necessary for you — not just convenient. Prescribed by a doctor, a nurse practitioner or another primary care professional.
Does Medicare pay for elevated toilet seat?
Medicare generally considers toilet safety equipment such as risers, elevated toilet seats and safety frames to be personal convenience items and does not cover them. Medicare Advantage may offer some coverage if your plan includes supplemental OTC benefits.Oct 13, 2021
Is a wheelchair covered by Medicare?
Medicare Part B (Medical Insurance) covers power-operated vehicles (scooters), walkers, and wheelchairs as durable medical equipment (DME). Medicare helps cover DME if: The doctor treating your condition submits a written order stating that you have a medical need for a wheelchair or scooter for use in your home.
What medical expenses are not covered by Medicare?
Some of the items and services Medicare doesn't cover include:Long-Term Care. ... Most dental care.Eye exams related to prescribing glasses.Dentures.Cosmetic surgery.Acupuncture.Hearing aids and exams for fitting them.Routine foot care.
Does Medicare cover dental?
Dental services Medicare doesn't cover most dental care (including procedures and supplies like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices). Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Does Medicare pay for transport chairs?
Medicare can cover a transport chair, but to be covered, the use of one should be deemed medically necessary.Mar 15, 2022
Are Pleurx drainage kit covered by Medicare?
For patients with Medicare, the pleural vacuum drainage bottles are considered a “bundled” nonroutine supply and the home healthcare agency is responsible for the costs of supplying this equipment.Nov 5, 2021
Are incontinence supplies covered by Medicare?
Unfortunately, Medicare does not currently offer coverage for any absorbent incontinent products. This means that products such as bladder control pads, adult briefs, diapers, pull-ons, and others all must be paid for through other means.
Does Medicare cover over the counter items?
Generally, your Medicare drug plan only covers prescription drugs and won't pay for over-the-counter drugs, like aspirin or laxatives. Your Medicare drug plan will only cover prescription drugs that are on its formulary (drug list), unless it's covered by an exception.
Medicare Part B covers durable medical equipment costs, but it must be medically necessary and prescribed by a qualified healthcare provider
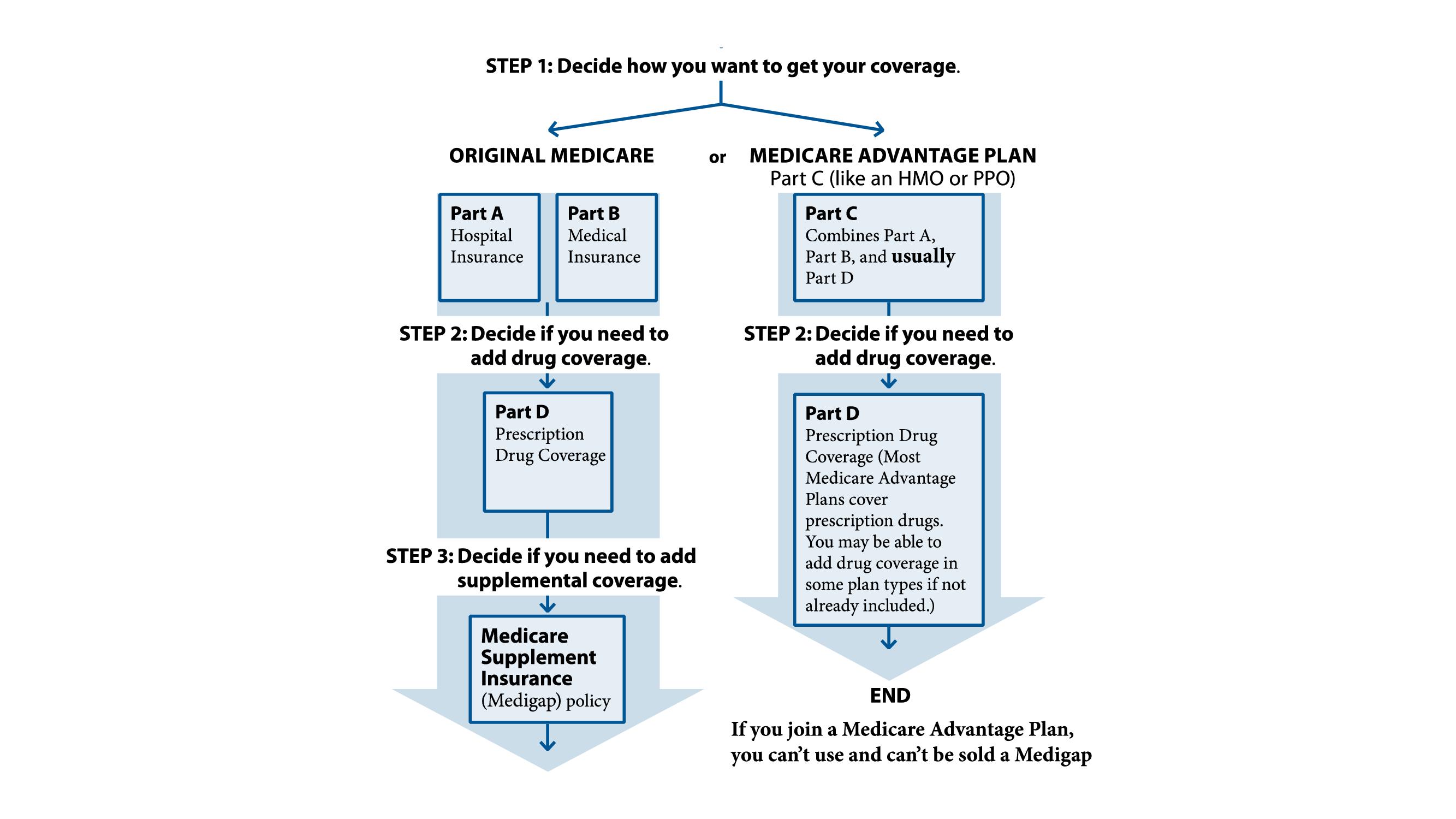
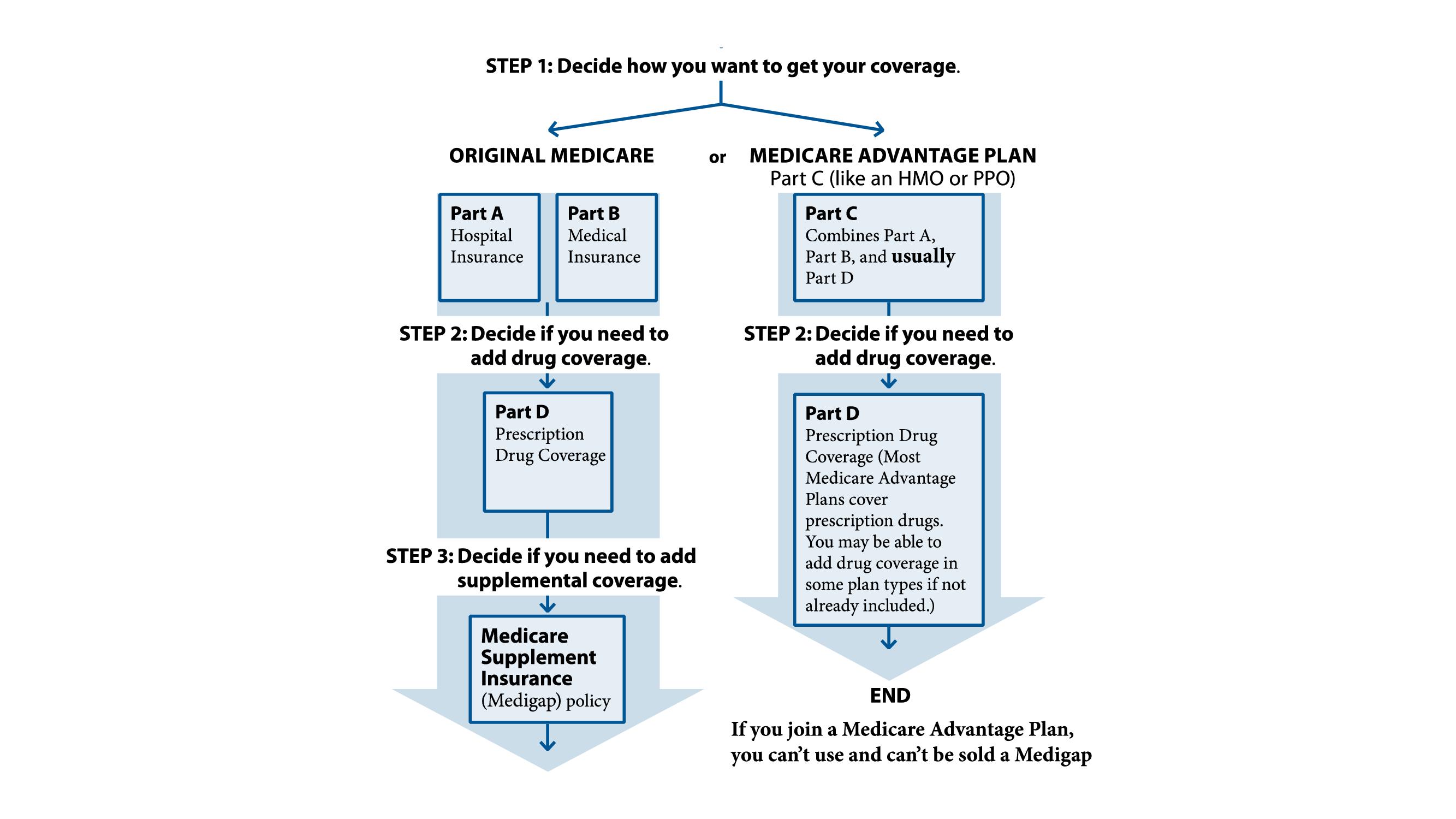
Original Medicare includes two parts: A and B. Medicare Part A covers inpatient services received in a hospital or skilled nursing facility (SNF) as well as hospice care. Medicare Part B provides coverage for doctor visits, lab work, durable medical equipment (DME), and more.
What Is Durable Medical Equipment?
As the name implies, durable medical equipment holds up against repeated or prolonged use. According to Medicare, it must be medically necessary, intended for home use, and of little use to someone unless they are sick or injured. Finally, durable medical equipment usually has an expected lifespan of 3 or more years.
How Does Medicare Cover Durable Medical Equipment?
Medicare Part B covers durable medical equipment. The Part B deductible applies and beneficiaries pay 20 percent of the Medicare-approved amount.
When Does Medicare Cover Durable Medical Equipment?
Medicare covers durable medical equipment when it has been prescribed by a qualified healthcare provider who deems it medically necessary for use in the home. Both the medical provider and DME supplier must be enrolled in Medicare.
How Much Does Durable Medical Equipment Cost with Medicare?
Your costs for durable medical equipment under Medicare are 20 percent of the Medicare-approved amount. This assumes both your medical provider and DME supplier participate in Medicare.
What Durable Medical Equipment Does Medicare Cover?
Medicare covers a wide variety of durable medical equipment. Covered items include (but are not limited to):
Does Medicare Advantage Cover Durable Medical Equipment?
Also known as Medicare Part C, Medicare Advantage plans must provide the same benefits as Medicare Parts A and B. However, details like out-of-pocket costs are determined by the insurance company that provides the plan.
What is assignment in Medicare?
Assignment —An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare pay for DME repairs?
Medicare will pay 80% of the Medicare-approved amount (up to the cost of replacing the item) for repairs. You pay the other 20%. Your costs may be higher if the supplier doesn’t accept assignment.
How much does Medicare pay for equipment?
If you are in the original Medicare program, Medicare pays 80 percent of the cost of covered equipment and supplies and you’re responsible for the remaining 20 percent, unless you have additional insurance (such as Medigap) that covers this cost.
What medical equipment does Medicare cover?
What medical equipment and supplies does Medicare cover? En español | Medicare Part B helps to pay for many items of medical equipment and supplies that help you function — for example, wheelchairs, artificial limbs, pacemakers, commode chairs, hospital beds, appliances to help breathing, neck and back braces, oxygen supplies and many more.
How to qualify for Medicare?
To qualify for Medicare coverage, the equipment or supplies must be: 1 Medically necessary for you — not just convenient 2 Prescribed by a doctor, a nurse practitioner or another primary care professional 3 Not easily used by anyone who isn’t ill or injured 4 Reusable and likely to last for three years or more 5 Appropriate for use within the home 6 Provided by suppliers that Medicare has approved
Does Medicare cover oxygen equipment?
Provided by suppliers that Medicare has approved. For some items — such as oxygen equipment or a seat lift to help you get into and out of a chair — Medicare requires a doctor to fill out and sign a certificate of medical necessity; without it, Medicare will deny coverage.
Does Medicare cover disposable items?
With only a few exceptions, Medicare doesn’t cover disposable items. To qualify for Medicare coverage, the equipment or supplies must be: Prescribed by a doctor, a nurse practitioner or another primary care professional.