What is a Medicare expansion?
Medicare expansion refers to broadening the benefits of the program, as the parts in which beneficiaries enroll through the government provide limited coverage. Throughout the years, extensions of the program have been uncommon, with one of the most notable instances being coverage of disabled individuals under 65.
Should the federal government expand Medicare?
On the other hand, the federal government solely runs Medicare, so expansion would need to happen nationwide. Therefore, there must be majority support for the expansion of Medicare, and the bill must pass for it to be possible.
What changes are coming to Medicare in 2018?
As we head into the 2018 enrollment period, you should be aware of three notable changes to Medicare or the Medicare Advantage market, along with one aspect of Medicare that surprisingly didn't change for some folks. 1. Rejoice! Part D premiums are going down
What is the last year of the Medicare EHR Incentive Program?
It is important to note that 2018 is the last year of downward payment adjustments for clinicians in the Medicare EHR Incentive Program. There are approximately 180,000 clinicians subject to a downward payment adjustment in 2018 under Medicare for failing to demonstrate meaningful use.

What is the downside of Medicaid expansion?
Very few studies reported that Medicaid expansion was associated with negative consequences, such as increased wait times for appointments—and those studies tended to use study designs not suited for determining cause and effect.
What does Medicare expansion do?
Medicare expansion refers to broadening the benefits of the program, as the parts in which beneficiaries enroll through the government provide limited coverage. Throughout the years, extensions of the program have been uncommon, with one of the most notable instances being coverage of disabled individuals under 65.
When did Medicare expand?
1972For example, in 1972, Medicare was expanded to cover the disabled, people with end-stage renal disease (ESRD) requiring dialysis or kidney transplant, and people 65 or older that select Medicare coverage. More benefits, like prescription drug coverage, have been offered.
Can Medicare be extended?
More Information. On October 1, 2000, a new law extended Medicare coverage for an additional 4 1/2 years beyond the current limit. This law is for people who receive Social Security disability benefits and who go to work. Under this law, how long will I get to keep Medicare if I return to work?
What is Biden's plan for Medicare expansion?
The Medicare expansion in President Joe Biden's $1.75 trillion spending plan included fewer new benefits than some Democrats had hoped for. Medicare benefits would be expanded to include hearing coverage under a framework for a $1.75 trillion spending plan released by President Joe Biden on Thursday.
Does ND Medicaid expansion cover dental?
For recipients under the age of 21, ND Medicaid covers re-treatment of bicuspid root canals and molar root canals (D3347 and D3348). Periodontal scaling, four or more teeth, per quadrant (D4341) or one to three teeth, per quadrant (D4342) requires service authorization for adults age 21 and older.
How has Medicare changed over the years?
Medicare has expanded several times since it was first signed into law in 1965. Today Medicare offers prescription drug plans and private Medicare Advantage plans to suit your needs and budget. Medicare costs rose for the 2021 plan year, but some additional coverage was also added.
What changes may occur for Medicare benefits in the next 20 years?
8 big changes to Medicare in 2020Part B premiums increased. ... Part B deductible increased. ... Part A premiums. ... Part A deductibles. ... Part A coinsurance. ... Medigap Plans C and F are no longer available to newly eligible enrollees. ... Medicare Plan Finder gets an upgrade for the first time in a decade.More items...
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What changes are coming to Medicare in 2021?
The Medicare Part B premium is $148.50 per month in 2021, an increase of $3.90 since 2020. The Part B deductible also increased by $5 to $203 in 2021. Medicare Advantage premiums are expected to drop by 11% this year, while beneficiaries now have access to more plan choices than in previous years.
What happens when you run out of Medicare days?
For days 21–100, Medicare pays all but a daily coinsurance for covered services. You pay a daily coinsurance. For days beyond 100, Medicare pays nothing. You pay the full cost for covered services.
What changes are coming to Medicare in 2022?
Changes to Medicare in 2022 include a historic rise in premiums, as well as expanded access to mental health services through telehealth and more affordable options for insulin through prescription drug plans. The average cost of Medicare Advantage plans dropped while access to plans grew.
What is the alternative to Medicare?
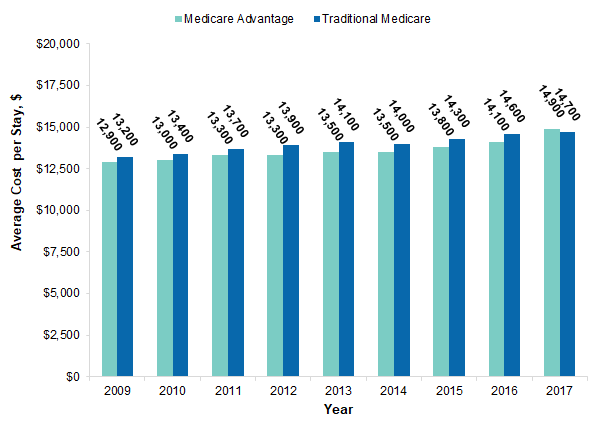
The aforementioned alternative to Medicare, known as Medicare Advantage (MA), has been an increasingly popular option for eligible enrollees. Between 2005 and 2015, the number of eligible Medicare enrollees who chose an MA plan instead of traditional Medicare rose from 13% to 30%.
Did Avalere Health drop Part D?
Normally, this data would take a long time to pore over, but Avalere Health did the grunt work, thankfully. When all is said and done, Avalere's experts found that Part D (prescription drug plan) premiums are set to drop slightly in 2018 as a result of higher-than-predicted rebates.
Is there a maximum out of pocket for Medicare?
Traditional Medicare doesn't offer these coverage options, and there is no maximum annual out-of-pocket expense. In 2018, MA providers will offer plenty of $0 monthly premium plans to act as a lure to attract seniors, but the number of plans with out-of-pocket expenses capped at $4,000 or less will be significantly lower, according to Avalere.
Is Part D insurance falling?
However, just because Part D premiums are falling doesn't mean you should blindly remain enrolled in the same Part D plan as you had in 2017. Premiums and coverage commonly change from year to year on most plans, meaning what offered the best value in 2017 may not be the best value for you in 2018. You'll want to closely examine ...
Will Part B premiums increase in 2018?
Lastly, it's worth pointing out what was brushed over above: Part B premiums aren't expected to increase in 2018. While that's great news for newly eligible enrollees, as well as those folks who haven't enrolled for Social Security as of yet, it's not necessarily great news for those protected by the hold harmless clause.
How long does a certified EHR stay on Medicare?
Eligible clinicians who successfully demonstrated meaningful use of certified EHR technology could have received incentive payments under Medicare for up to 5 consecutive years throughout the duration of the program. The program started in 2011, and payments continued under Medicare through 2016 with no Medicare incentive payments available ...
How to qualify for incentive payments under Medicare?
To qualify for incentive payments under Medicare, clinicians must have successfully demonstrated meaningful use for an applicable EHR reporting period for each payment year of the program. From 2015 through 2018, clinicians who do not successfully demonstrate meaningful use will be subject to a downward adjustment to Medicare physician fee schedule ...
How many clinicians are subject to downward payment adjustment in 2018?
There are approximately 180,000 clinicians subject to a downward payment adjustment in 2018 under Medicare for failing to demonstrate meaningful use.
How often do you have to demonstrate meaningful use in Medicare?
Clinicians must demonstrate meaningful use every year in order to avoid Medicare downward payment adjustments in the years identified above. For example, a clinician that demonstrated meaningful use for the first time in 2013 would have avoided the payment adjustment in 2015, but would have had to demonstrate meaningful use again in 2016 in order to avoid the payment adjustment in 2018. It is important to note that 2018 is the last year of downward payment adjustments for clinicians in the Medicare EHR Incentive Program.
Can a clinician participate in the EHR incentive program?
If a clinician is eligible to participate in the Medicare EHR Incentive Program, by law they must successfully demonstrate meaningful use in either the Medicare EHR Incentive Program or in the Medicaid EHR Incentive Program, to avoid a downward Medicare payment adjustment. Medicaid clinicians who do not furnish covered professional services ...
Will EHR incentive be reported to MIPS?
Clinicians who previously reported under the Medicare EHR Incentive Program will instead report to MIPS for 2017, and are subject to the program requirements and payment adjustments of that program. However, if a clinician has not successfully demonstrated meaningful use in a prior year and wants to avoid the 2018 downward payment adjustment ...
How many states have expanded Medicaid?
If all those states actually implement Medicaid expansion, that would bring the total number of states that have done so to 39. “We're clearly going to see Maine, Idaho, Utah, Nebraska and probably Kansas expanding in 2019, and I suspect you'll see it in other states, too,” said Matt Salo, executive director of the National Association ...
When did the Affordable Care Act get repealed?
With congressional action to repeal the Affordable Care Act off the table in 2018, the Trump administration and the states engaged in a tense tug of war through the year between expanding, not expanding and limiting Medicaid eligibility.
Medicare vs. Medicaid Expansion
While many states have expanded their Medicaid programs, the process for doing the same with Medicare would be very different. Medicaid is government health insurance for those with low incomes, which the federal and state governments collectively manage.
Who Pays for Medicare Expansion?
Medicare primarily receives funding through payroll taxes. Thus, more tax revenue will be necessary for an expansion to be possible.
FAQs
No state has the power to expand Medicare, as it is a federal program. However, states are able to expand their Medicaid programs within federal guidelines.
A sticking point
The expansion has become a major sticking point in talks for the bill. Sen. Bernie Sanders, I- Vt., has said that the new benefits must be included in legislation. He also demanded that the bill allow Medicare to negotiate lower drug prices with pharmaceutical companies.
Medicaid expansion also in danger
Other health-care costs are also on the chopping block. Plans to expand Medicaid to close a coverage gap for low-income Americans in states that did not expand the program under the Affordable Care Act may also be cut — the proposal would cost roughly $300 billion over the next decade.