Is the Medicare penalty forever?
Generally, once Medicare determines a person's penalty amount, the person will continue to owe a penalty for as long as they're enrolled in Medicare drug coverage. This means that even if the person decides to join another Medicare plan, they will still have to pay the penalty once enrolled in a new plan.
How do I get rid of Medicare late enrollment penalty?
3 ways to avoid the Part D late enrollment penaltyEnroll in Medicare drug coverage when you're first eligible. ... Enroll in Medicare drug coverage if you lose other creditable coverage. ... Keep records showing when you had other creditable drug coverage, and tell your plan when they ask about it.
Can Medicare penalty be waived?
You may qualify to have your penalty waived if you were advised by an employee or agent of the federal government – for example by Social Security or 1-800-MEDICARE – to delay Part B. Asking for the correction is known as requesting equitable relief.Apr 27, 2020
How do I avoid Medicare Part B penalty?
One way to avoid the Medicare Part B Penalty is to enroll during your Initial Enrollment Period. If you're turning 65, you can enroll in Medicare Part B during this enrollment period. Your Initial Enrollment Period begins on the first day of the month, three months before you turn 65.
How long is a member responsible for a late enrollment penalty?
For most people, you have to pay the LEP as long as you are enrolled in the Medicare prescription drug benefit. There are some exceptions: If you receive Extra Help, your penalty will be permanently erased. If you are under 65 and have Medicare, your LEP will end when you turn 65.
How do I dispute a late enrollment penalty?
Part D Late Enrollment Penalty Reconsideration Request Form An enrollee may use the form, “Part D LEP Reconsideration Request Form C2C” to request an appeal of a Late Enrollment Penalty decision. The enrollee must complete the form, sign it, and send it to the Independent Review Entity (IRE) as instructed in the form.Dec 1, 2021
What will Irmaa be in 2021?
C. IRMAA tables of Medicare Part B premium year for three previous yearsIRMAA Table2021More than $222,000 but less than or equal to $276,000$297.00More than $276,000 but less than or equal to $330,000$386.10More than $330,000 but less than $750,000$475.20More than $750,000$504.9012 more rows•Dec 6, 2021
Why is there a penalty for Medicare Part B?
The Medicare Part B late enrollment penalty is in place to help guide Medicare seniors to enroll in Part B at the right time.
What is the grace period for Medicare payment?
a 90-dayUnder rules issued by the Centers for Medicare and Medicaid Services (CMS), consumers will get a 90-day grace period to pay their outstanding premiums before insurers are permitted to drop their coverage.
Does Medicare affect credit score?
Medical debt does not affect your credit score unless it's reported to a credit bureau, and virtually no hospital or medical provider will report the debt directly, according to the National Consumer Law Center (NCLC).Aug 8, 2019
Can I decline Medicare Part B?
Declining Part B Coverage You can decline Medicare Part B coverage if you can't get another program to pay for it and you don't want to pay for it yourself. The important thing to know about declining Part B coverage is that if you decline it and then decide that you want it later, you may have to pay a higher premium.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.Jan 3, 2022
What happens if you don't get Part B?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
How much is the penalty for Part B?
Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B. (Even though you weren't covered a total of 27 months, this included only 2 full 12-month periods.) Find out what Part B covers.
What happens if Medicare pays late enrollment?
If Medicare’s contractor decides that your late enrollment penalty is correct, the Medicare contractor will send you a letter explaining the decision, and you must pay the penalty.
What happens if Medicare decides the penalty is wrong?
What happens if Medicare's contractor decides the penalty is wrong? If Medicare’s contractor decides that all or part of your late enrollment penalty is wrong, the Medicare contractor will send you and your drug plan a letter explaining its decision. Your Medicare drug plan will remove or reduce your late enrollment penalty. ...
What is the late enrollment penalty for Medicare?
Part D late enrollment penalty. The late enrollment penalty is an amount that's permanently added to your Medicare drug coverage (Part D) premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there's a period of 63 or more days in a row when you don't have Medicare drug coverage or other.
What is creditable prescription drug coverage?
creditable prescription drug coverage. Prescription drug coverage (for example, from an employer or union) that's expected to pay, on average, at least as much as Medicare's standard prescription drug coverage. People who have this kind of coverage when they become eligible for Medicare can generally keep that coverage without paying a penalty, ...
How long do you have to pay late enrollment penalty?
You must do this within 60 days from the date on the letter telling you that you owe a late enrollment penalty. Also send any proof that supports your case, like a copy of your notice of creditable prescription drug coverage from an employer or union plan.
How long does it take for Medicare to reconsider?
In general, Medicare’s contractor makes reconsideration decisions within 90 days. The contractor will try to make a decision as quickly as possible. However, you may request an extension. Or, for good cause, Medicare’s contractor may take an additional 14 days to resolve your case.
Does Medicare pay late enrollment penalties?
, you don't pay the late enrollment penalty.
How long does it take to enroll in Medicare Part D?
You can enroll in Medicare Part D without incurring a late enrollment penalty during the 3-month period that begins when your Medicare parts A and B become active. If you wait past this window to enroll, a late enrollment penalty for Medicare Part D will be added to your monthly premium. This fee is 1 percent of the average monthly prescription ...
What happens if you don't sign up for Medicare?
If you’re not automatically enrolled and don’t sign up for Medicare Part A during your initial enrollment period, you’ll incur a late enrollment penalty when you do sign up. The late enrollment penalty amount is 10 percent of the cost of the monthly premium. You’ll have to pay this additional cost each month for twice the number ...
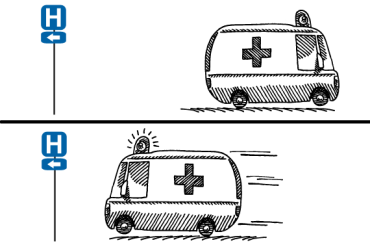
What happens if you delay Medicare enrollment?
Delaying enrollment in Medicare can subject you to long-lasting financial penalties added to your premiums each month. A late enrollment penalty can significantly increase the amount of money you’re required to pay for each part of Medicare for years. Share on Pinterest.
How long does Medigap last?
This period starts on the first day of the month you turn 65 and lasts for 6 months from that date. If you miss open enrollment, you may pay a much higher premium for Medigap.
Why is Medicare charging late fees?
Charging late fees helps to reduce these costs overall and encourage people to enroll on time.
How long does Medicare Part B take to enroll?
Part B late enrollment penalty. You’re eligible for Medicare Part B starting 3 months before your 65th birthday until 3 months after it occurs. This period of time is known as the initial enrollment period.
How long do you have to enroll in Medicare?
make sure to enroll during the 8-month period when your current coverage ends, known as a special enrollment period.
How long does it take to pay Medicare premiums after disenrollment?
If your request is approved, you’ll have to pay your outstanding premiums within three months of disenrollment to resume coverage. If you’re disenrolled from Medicare Advantage, you’ll be automatically enrolled in Original Medicare. During this time, you may lose drug coverage.
What happens if you fail to make your Medicare payment?
Only once you fail to make your payment by the end of your grace period do you risk disenrollment from your plan. In some cases, you’ll be given the option to contact your plan administrator if you’re behind on payments due to an underlying financial difficulty.
How long do you have to pay Medicare Part B?
All told, you’ll have a three-month period to pay an initial Medicare Part B bill. If you don’t, you’ll receive a termination notice informing you that you no longer have coverage. Now if you manage to pay what you owe in premiums within 30 days of that termination notice, you’ll get to continue receiving coverage under Part B.
What happens if you don't pay Medicare?
What happens when you don’t pay your Medicare premiums? A. Failing to pay your Medicare premiums puts you at risk of losing coverage, but that won’t happen without warning. Though Medicare Part A – which covers hospital care – is free for most enrollees, Parts B and D – which cover physician/outpatient/preventive care and prescription drugs, ...
What happens if you miss a premium payment?
But if you opt to pay your premiums manually, you’ll need to make sure to stay on top of them. If you miss a payment, you’ll risk having your coverage dropped – but you’ll be warned of that possibility first.
How long is the grace period for Part C and D?
All Part C and D plans must have a grace period that’s at least two months in length, and some plans have a longer grace period. If you fail to make a premium payment, your plan must send you a written notice of non-payment and tell you when your grace period ends.
When is Medicare Part B due?
Your Medicare Part B payments are due by the 25th of the month following the date of your initial bill. For example, if you get an initial bill on February 27, it will be due by March 25. If you don’t pay by that date, you’ll get a second bill from Medicare asking for that premium payment.
What is Medicare premium based on?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That’s your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS. To set your Medicare cost for 2021, Social Security likely relied on the tax return you filed in 2020 that details your 2019 ...
What is a hold harmless on Medicare?
If you pay a higher premium, you are not covered by “hold harmless,” the rule that prevents most Social Security recipients from seeing their benefit payment go down if Medicare rates go up. “Hold harmless” only applies to people who pay the standard Part B premium and have it deducted from their Social Security benefit.
What is the Medicare Part B rate for 2021?
If your MAGI for 2019 was less than or equal to the “higher-income” threshold — $88,000 for an individual taxpayer, $176,000 for a married couple filing jointly — you pay the “standard” Medicare Part B rate for 2021, which is $148.50 a month.
Do you pay Medicare Part B if you are a high income beneficiary?
If you are what Social Security considers a “higher-income beneficiary,” you pay more for Medicare Part B, the health-insurance portion of Medicare. (Most enrollees don’t pay for Medicare Part A, which covers hospitalization.) Medicare premiums are based on your modified adjusted gross income, or MAGI. That’s your total adjusted gross income ...
Can you ask Social Security to adjust your premium?
You can ask Social Security to adjust your premium if a “life-changing event” caused significant income reduction or financial disruption in the intervening tax year — for example, if your marital status changed , or you lost a job , pension or income-producing property. You’ll find detailed information on the Social Security web page “Medicare ...
What is the Medicare doughnut hole?
The Medicare Doughnut Hole Returns. Since 2011 the ACA has been steadily closing the prescription drug coverage gap , known as the doughnut hole, in Medicare Part D by requiring drug manufacturers and insurers to pick up more of the cost.
How long will the ACA last?
A study cited in the amicus brief filed by the Center for Medicare Advocacy found that the ACA extended the solvency of the program’s trust fund by eight years to 2026, mostly by finding new sources of revenue and slowing the growth of payments to all providers.
What is California v Texas?
Texas, which was filed by 20 Republican-leaning states, challenges whether the Affordable Care Act can exist without the individual mandate to buy health insurance. A Republican-controlled Congress removed the financial penalty for those without insurance in 2017. “If the ACA was repealed or rescinded in full, ...
What is the significance of Ruth Bader Ginsburg's death?
Supreme Court Justice Ruth Bader Ginsburg’s death heightened the stakes in a case scheduled to appear before the court Nov. 10 that could reverse improvements to Medicare and raise out-of-pocket costs for beneficiaries. The case, California v. Texas, which was filed by 20 Republican-leaning states, challenges whether the Affordable Care Act can exist without the individual mandate to buy health insurance. A Republican-controlled Congress removed the financial penalty for those without insurance in 2017.
Will Medicare premiums rise faster?
Medicare Premiums and Medicare Deductibles Will Rise Faster. Curbing provider payments also lowered costs for seniors, helping to keep Medicare Part A deductibles and copayments in check. Similarly, Part B premiums and deductibles are much lower than projected before the ACA became law.
Does Medicare Advantage charge more for chemo?
The ACA requires Medicare Advantage plans to spend 85% of premium dollars on health care, not profits or overhead. The plans also can’t charge more than traditional Medicare for chemotherapy , renal dialysis, skilled nursing care and other specialized services.
