Medicare will also cover some or all the costs of seeing a GP or specialist outside of hospital, and some pharmaceuticals. Medicare does not cover private patient hospital costs, ambulance services, and other out of hospital services such as dental, physiotherapy, glasses and contact lenses, hearings aids.
Full Answer
What does Medicare not cover in hospitals?
What Medicare doesn’t cover. Personal comfort items : Medicare does not cover personal comfort items used during an inpatient hospital stay, such as shampoo, toothbrushes, or razors. It doesn’t cover the cost of a radio, television, or phone in your hospital room if there’s an extra charge for those items.
What does Medicare Part A not pay for?
You will generally be responsible for paying a portion of the inpatient care that Medicare Part A does not pay. Let’s break down these expenses. Deductible: This is an amount you have to spend before Medicare starts to pay for covered services. The deductible amount may change from year to year.
What hospital services are covered by Medicare?
Medicare-covered hospital services include: 1 Semi-private rooms 2 Meals 3 General nursing 4 Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) 5 Other hospital services and supplies as part of your inpatient treatment More ...
How much does Medicare pay for inpatient hospital care?
This coinsurance is set annually ($352 in 2020) and appears in your Medicare benefit coverage booklet. After 90 days of Medicare-covered inpatient hospital care in the same benefit period, you might be responsible for 100% of the costs. However, Medicare allows you a further 60 days of “lifetime reserve” days.
What Medicare Doesn’T Cover
Original Medicare, Part A and Part B, doesn’t generally cover the following services and supplies. This may not be a complete list.Alternative medi...
Can I Get Benefits That Pay For Services Medicare Does Not Cover?
Medicare Advantage plans may be an option to consider since they are required to have at least the same level of coverage as Original Medicare, but...
What Medicare Part D Doesn’T Cover
Medicare Part D is optional prescription drug coverage. You can enroll in this coverage through a stand-alone Medicare Part D Prescription Drug Pla...
Can you transfer financial liability to a patient?
To transfer potential financial liability to the patient, you must give written notice to a Fee-for-Service Medicare patient before furnishing items or services Medicare usually covers but you don’ t expect them to pay in a specific instance for certain reasons, such as no medical necessity .
Does Medicare cover non-physician services?
Medicare normally excludes coverage for non-physician services to Part A or Part B hospital inpatients unless those services are provided either directly by the hospital/SNF or under an arrangement that the hospital/SNF makes with an outside source.
Does Medicare cover dental care?
Medicare doesn’t cover items and services for the care, treatment, filling, removal, or replacement of teeth or the structures directly supporting the teeth, such as preparing the mouth for dentures, or removing diseased teeth in an infected jaw. The structures directly supporting the teeth are the periodontium, including:
Does Medicare cover personal comfort items?
Medicare doesn’t cover personal comfort items because these items don’t meaningfully contribute to treating a patient’s illness or injury or the functioning of a malformed body member. Some examples of personal comfort items include:
Does Medicare cover exceptions?
This booklet outlines the 4 categories of items and services Medicare doesn’t cover and exceptions (items and services Medicare may cover). This material isn’t an all-inclusive list of items and services Medicare may or may not cover.
What are the requirements for Medicare Part D?
Generally, Medicare Part D will cover certain prescription drugs that meet all of the following conditions: 1 Only available by prescription 2 Approved by the Food and Drug Administration (FDA) 3 Sold and used in the United States 4 Used for a medically accepted purpose 5 Not already covered under Medicare Part A or Part B
What is Medicare services?
Medicare considers services needed for the diagnosis, care, and treatment of a patient’s condition to be medically necessary. These supplies and services cannot be primarily for the convenience of the provider or beneficiary. Always ask your doctor to clarify if you’re not sure whether a specific service or item is covered by Medicare.
What happens if you take a medication that is not covered by Medicare?
If you are taking a medication that is not covered by Medicare Part D, you may try asking your plan for an exception. As a beneficiary, you have a guaranteed right to appeal a Medicare coverage or payment decision.
Does Medicare cover prescription drugs?
Generally, Medicare Part D will cover certain prescription drugs that meet all of the following conditions: Only available by prescription. Approved by the Food and Drug Administration (FDA) Sold and used in the United States. Used for a medically accepted purpose. Not already covered under Medicare Part A or Part B.
Does Medicare cover homemaker services?
You must be taking the most direct route and traveling “without unreasonable delay.”. Homemaker services : Medicare won’t cover homemaker services, such as cooking and cleaning. An exception is if the beneficiary is in hospice care, and the homemaker services are included in the care plan. Long-term care : Medicare doesn’t cover long-term ...
Does Medicare cover foot care?
Foot care : Medicare does not cover routine foot care (such as removal of calluses or nail-cutting), but Part B covers medically necessary podiatrist services to treat foot injuries or diseases. Hearing care : Medicare won’t cover routine hearing exams, hearing aids, and exams to get fitted for hearing aids. However, you may be covered ...
Does Medicare cover short term nursing?
However, Medicare does cover short-term skilled nursing care when it follows a qualifying inpatient hospital stay. Medicare Part A may cover nursing care in a skilled nursing facility (SNF) for a limited time if it’s medically necessary for you to receive skilled care.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What Can You Expect To Pay For An Approved Inpatient Surgery
Medicare Part A generally covers much of the cost related to your inpatient surgery and hospital stay. You may be responsible for a Medicare Part A deductible for each benefit period.
Is Medicare Part A Free At Age 65
Premium-free Part A coverage is available if you or your spouse paid Medicare taxes for a certain amount of time while working. You can receive this if:
Do You Have To Pay A Part A Premium
You may be wondering does Medicare Part A cover 100 percent? And while this is not the case, there are provisions in place to make Medicare affordable to beneficiaries.
Does Medicare Cover Inpatient Mental Health Treatment
You must have Medicare Part A to be covered for inpatient mental health treatment at a general or psychiatric hospital. Medicare will pay for most of your inpatient treatment services. However, you may still owe some out-of-pocket costs depending on your plan and the length of your stay.
Hospital Stay Coverage Under Medicare Advantage
You may choose to receive your Medicare Part A and Part B coverage through a local Medicare Advantage plan. Medicare Advantage plans are offered by private insurance companies that are approved by Medicare and cover at least the same level of benefits as Original Medicare Part A and Part B .
Hospital Observation Status And Medication Costs
Any prescription and over-the-counter drugs you receive in an outpatient setting arent covered by Part B. But if you have Medicare Part D , they may be covered in certain circumstances. If the drugs are covered, youll probably need to pay out of pocket and submit a claim to your drug plan for a refund.
What Medicare Part A Does Not Cover
While this part of Medicare covers stays in a nursing home, it will only do so if it is medically necessary. If you need non-medical long-term care, such as for chronic illness or disability, youâll have to consider other options like long-term care insurance.
How many days can you draw on Medicare?
However, Medicare allows you a further 60 days of “lifetime reserve” days. This means that for the rest of your life you can draw on any of these 60 days—but no more—to extend Medicare coverage in any benefit period. In 2021, you pay $742 coinsurance per day for each lifetime reserve day.
How long is Medicare coinsurance for 2021?
This coinsurance ($371 in 2021) may vary from year to year and appears in your Medicare benefit coverage booklet. After 90 days of Medicare-covered inpatient hospital care in the same benefit period, you might be responsible for 100% of the costs. However, Medicare allows you a further 60 days of “lifetime reserve” days.
How much is the Medicare deductible for 2021?
You are responsible for the Medicare Part A hospital deductible ($1,484 in 2021), which applies to each new benefit period. You must pay the deductible before Medicare Part A covers services you received in the hospital.
What is deductible in Medicare?
Deductible: This is an amount you have to spend before Medicare starts to pay for covered services. The deductible amount may change from year to year. Coinsurance: This is the part of the Medicare-approved costs for hospital care you may be required to pay after you’ve met your deductible.
How long does it take to get a coinsurance for a hospital stay?
All covered costs except the Part A deductible during the first 60 days. Coinsurance amounts for hospital stays from 61 to 90 days. After 91 days, a coinsurance amount usually applies for each “lifetime reserve day.”. You may get up to 60 lifetime reserve days during your lifetime.
How long do you have to stay in a hospital before you can get Medicare?
Hospital stay and skilled nursing facility care. Under the Original Medicare program, you must be admitted and spend at least 3 days in the hospital as an inpatient before Medicare will cover your stay in an approved skilled nursing facility (SNF) for further care.
How many days can you be in a hospital for mental health?
However, if you are hospitalized in a specialized hospital for mental health care, Medicare covers only 190 inpatient psychiatric days in your lifetime.
What happens if a healthcare provider is not in network?
If a healthcare provider is not in-network, you can likely end up paying higher out-of-network prices for those specific services. For planned procedures, you can find out in advance from your health plan whether your providers are contracted and if the services you will get are covered under your policy.
What is a facility fee?
This is charged to the patient by the hospital for use of their hospital facilities and equipment. Most insurance policies don’t cover facility fees, so to be prepared, or if possible, avoid this unexpected cost, ask your healthcare provider if you will be charged a facility fee or get a separate bill from the hospital.
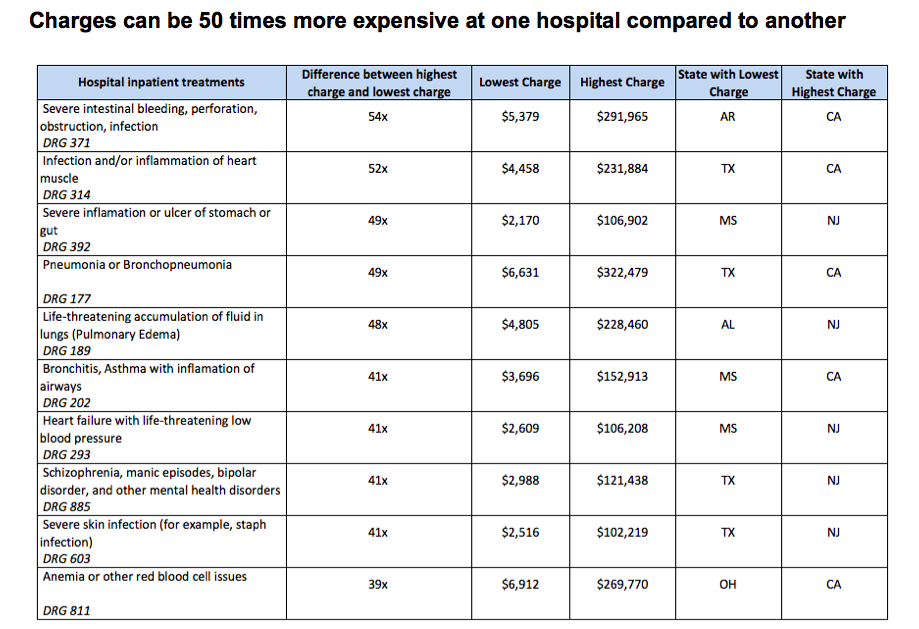
What to do if your health is not life threatening?
If your health situation is not life threatening or urgent, take the opportunity to find a cheaper solution. Consider seeking a second opinion and do your research before agreeing to treatment or surgery. Find out if there are recommended alternatives or options that are just as good and possibly cheaper.
Can a doctor be in network with Medicare?
Even though a hospital is in your health plan’s network, some doctors who provide services there might not be. While your doctor may accept assignment, other healthcare providers like radiologists, anesthesiologists, pathologists, and neonatologists may not. If you have Original Medicare, you are responsible for making sure that all of the providers involved in your care will accept assignment. If you are enrolled in a Medicare Advantage plan, your primary care physician will help manage your care and make certain all the medical professionals involved are within your plan’s network. Understand your plan and your options as you choose providers. You may choose an in-network hospital and surgeon, but the on-duty anesthesiologist can be out of network and your bloodwork can be sent to an out-of-network lab. This is why it’s important to know not only if the doctor you are interacting with is in your insurance network but also who else is working behind the scenes. If a healthcare provider is not in-network, you can likely end up paying higher out-of-network prices for those specific services.
Can you refuse unnecessary equipment?
You have the option to refuse unne cessary equipment like wheelchairs, slings, and splints which can often be purchased outside of a hospital or doctor’s office for less money. You may also refuse unnecessary care. If hospitalized, ask your healthcare providers about their role and who sent them to help determine if their check-ins are necessary for your health.
Do hospitals charge for private rooms?
Hospitals that have both private and semi-private rooms may charge you more for the single occupancy room. If you are comfortable sharing a room for a potentially lower cost, make it clear that you did not request the private room and that you are willing to occupy a room with another patient. The extra charge for a private room or suite may not be covered by your insurance policy and you may be able to save significantly by sharing.
Can you dispute a medical bill?
You may be able to negotiate or dispute your medical bill and reduce a large medical bill amount or settle on different payment terms. If you are concerned that you have been charged for unnecessary services, or for services you never received, please report the fraudulent behavior to Medicare.