Those who do not sign up for Medicare Part B when they’re first eligible and don’t qualify for a Special Enrollment Period may be subject to a late enrollment penalty. This could mean paying a 10% higher monthly premium for every 12-month period that you were eligible for Part B but didn’t enroll.
What happens if I don't have Medicare Part B?
Aug 31, 2021 · So if you don’t have Medicare Part B and have a $10,000 medical event, you would be responsible for $8,000 before his retirement program kicked in, she said. She said that’s a big risk to take given the cost of healthcare today. Always make sure to get clarification on your specific situation from your plan administrator.
Do I pay a late enrollment penalty for Medicare Part B?
Part B late enrollment penalty. If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B. And, the penalty increases the longer you go without Part B coverage.
When can I sign up for Medicare Part B?
Aug 31, 2021 · So if you don’t have Medicare Part B and have a $10,000 medical event, you would be responsible for $8,000 before his retirement program kicked …
Do you qualify for Medicare Part B extra help?
Jan 02, 2021 · Employer coverage, retiree coverage, COBRA, TFL and Medicaid all function as your secondary insurance only if do your part and first enroll in Part B. Failure to enroll in Part B means you will also owe a penalty if you decide to enroll later on. Related Article: Do I Need to Sign Up for Medicare if I am Still Working at 65?

Is Part B mandatory on Medicare?
Medicare Part B is optional, but in some ways, it can feel mandatory, because there are penalties associated with delayed enrollment. As discussed later, you don't have to enroll in Part B, particularly if you're still working when you reach age 65.
Can I opt out of paying Medicare Part B?
You can voluntarily terminate your Medicare Part B (medical insurance). However, since this is a serious decision, you may need to have a personal interview. A Social Security representative will help you complete Form CMS 1763.Nov 24, 2021
What parts of Medicare are mandatory?
There are four parts to Medicare: A, B, C, and D. Part A is automatic and includes payments for treatment in a medical facility. Part B is automatic if you do not have other healthcare coverage, such as through an employer or spouse.
You Always Need Part B If Medicare Is Primary
Once you retire and have no access to other health coverage, Medicare becomes your primary insurance. While Part A pays for your room and board in...
You Need Part B to Be Eligible For Supplemental Coverage
Medigap plans do not replace Part B. They pay secondary to Part B.Part B works together with your Medigap plan to provide you full coverage. This m...
Do I Need Medicare Part B If I Have Other Insurance?
Many people ask if they should sign up for Medicare Part B when they have other insurance. At a large employer with 20 or more employees, your empl...
Enrolling Into Part B on A Delayed Basis
If you have delayed Part B while you were still working at a large employer, you’ll still need to enroll in Part B eventually. When you retire and...
Do I Need Medicare Part B If I’M A Veteran?
Some people have 2 different coverages that they can choose independent of one another. Federal employees who can opt to use their FEHB instead of...
Most Common Mistakes Regarding Part B
The most common mistake we see is from people who confuse Part B and Medigap. Just this week, a reader on our Facebook page commented that she was...
What happens if you opt out of Part B?
Be aware that if you opt out of Part B and then later decide to join, you will pay a Part B late penalty. You’ll also need to wait until the next General Enrollment Period to enroll, which means there could be a delay before your coverage becomes active. In my opinion, most Veterans should sign up for Part B.
How long do you have to enroll in Part B if you retire?
When you retire and lose your employer coverage, you’ll be given a 8-month Special Enrollment Period to enroll in Part B without any late penalty.
How much does Medicare pay for outpatients?
Your healthcare providers will bill Medicare, and Part B will then pay 80% of your outpatient expenses after your small deductible. Medicare then sends the remainder of that bill to your Medigap plan to pay the other 20%. The same goes for Medicare Advantage plans.
How much is Part B insurance?
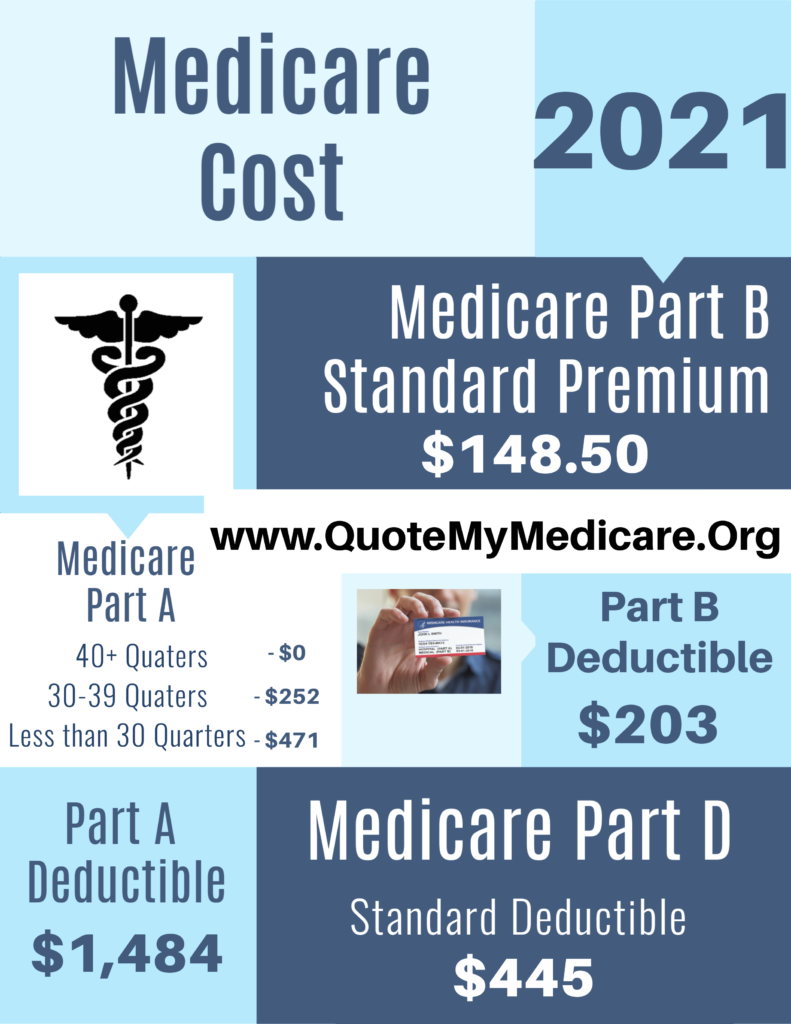
Most people delay Part B in this scenario. Your employer plan likely already provides good outpatient coverage. Part B costs at least $148.50/month for new enrollees in 2020.
Does Medigap replace Part B?
Medigap plans do not replace Part B. They pay secondary to Part B. Part B works together with your Medigap plan to provide you full coverage. This means you must be enrolled in Part B before you are even eligible to apply for a Medicare supplement.
Do you have to be enrolled in Part B for Medicaid?
When you are 65 or older and enrolled in Medicaid. All of these scenarios require you to be enrolled in Part B. Without it, you would be responsible for the first 80% of all outpatient charges. Even worse, your secondary coverage may not pay at all if you are not actively enrolled in Part B as your primary coverage.
Do all veterans qualify for VA?
Not all veterans qualify for VA coverage. Your length of military service and your discharge characterization affect your eligibility. If you plan to use VA healthcare coverage as your only coverage, be sure that you apply for VA coverage before your initial enrollment window for Medicare expires.
How much is Part B insurance?
That depends. The normal premium for Part B is $148.50, but that is for the “normal” premium. For high-income retirees (and I use the term “high-income” very loosely), that number escalates. It is remarkably easy for federal retirees, especially single retirees, to find themselves in this “high-income” category.
Does Part B replace FEHB?
Part B doesn’t replace the Federal Employees Health Benefits (FEHB), but rather supplements it.
Is Medicare Part B important?
The decision on whether or not to take Medicare Part B is an important one, and your income range should play a role in that decision. IRMAA is just one way that retirees can incur extra, unnecessary costs in retirement. Addressing seemingly little things like IRMAA can help you enjoy a fruitful retirement.
Does Aetna Direct cover dental?
The national Aetna Direct plan not only has a Medicare wraparound, but also lets you use your $900 a year per spouse personal care account to reimburse most of your Medicare Part B premium, or to offset dental and other expenses not covered by FEHB plans or Medicare.
Does a postal worker have health insurance?
Health insurance for postal workers is provided by the Federal Employee Health Benefits Program (FEHBP). It generally provides strong coverage and, I’m assuming, covered you as a retiree’s spouse while your husband was alive. The key question here is what happened to your coverage when your husband passed away.
Is Medicare correct to sign you up for Part B?
Further, your failure to return that card in a timely fashion does not necessarily mean that Medicare was correct to sign you up for Part B and begin to subtract the monthly premiums for Part B from your Social Security. However, it might have been correct.
Can I get Medicare if I turned 65?
You say you chose not to get Medicare, so I assume you already have turned 65. But if you just turned 65, it’s standard for Social Security to send you notice about Medicare enrollment. Social Security administers many aspects of Medicare including the enrollment process and handling the deduction of Part B premiums from monthly Social Security ...
What happens if you don't have Medicare Part B?
Going without Medicare Part B and not having other coverage might leave you paying high out-of-pocket costs for doctors’ visits, preventive care, and medical services. Health care needs tend to increase as people get older, and any potential savings from delaying enrollment in Part B could be offset if you get sick and don’t have medical coverage. If you wait to enroll and then contract an illness, you may not be able to sign up for Medicare Part B until the next General Enrollment Period. In the meantime, you may have to pay for all medical costs out-of-pocket.
What are the pros and cons of delaying Medicare Part B enrollment?
If you already have other coverage, the biggest advantage of delaying Part B enrollment is not paying an additional premium for benefits you may not need or use.
What type of coverage does not count as creditable?
The following types of coverage do not count as creditable coverage based on current employment and would not exempt you from paying the Part B penalty if you delay enrollment: COBRA. Retiree benefits. TRICARE (unless you, your spouse, or dependent child are an active-duty member)*. Veterans’ benefits.
How long do you have to work to get Medicare Part A?
Many individuals qualify for premium-free Medicare Part A (hospital insurance), provided that they have worked at least 10 years (or 40 quarters) and paid Medicare taxes during those time periods. For these individuals, it typically makes sense to keep Part A, since the coverage comes at no added cost. However, because Part B comes ...
Is it better to enroll in Part B or Part B?
For those who only spend part of the year living overseas, or those who foresee eventually moving back to the U.S., it may be safer to enroll in Part B when first eligible to avoid paying a large penalty later.
Do you have to pay for medical expenses out of pocket?
In the meantime, you may have to pay for all medical costs out-of-pocket. Those who do not sign up for Medicare Part B when they’re first eligible and don’t qualify for a Special Enrollment Period may be subject to a late enrollment penalty.
What happens if you opt out of Part B?
But beware: if you opt out of Part B without having creditable coverage—that is, employer-sponsored health insurance from your current job that’s as good or better than Medicare—you could face late-enrollment penalties (LEPs) down the line.
What to do if you drop Part B?
If you’re dropping Part B because you can’t afford the premiums, remember that you could save money on your health care costs in other ways. Consider adding a Medicare Advantage or Medigap plan instead of dropping Part B. Call us to learn more about these alternatives to disenrolling in Part B.
What happens if you don't have health insurance?
Without health insurance that’s as good or better than Medicare, you could start racking up late-enrollment penalties the longer you go without coverage. If you decide to re-enroll in Part B later, these penalties could make your premiums (what you pay for coverage) even less affordable.
How to schedule an interview with Social Security?
Call a Licensed Agent: 833-271-5571. You can schedule an in-person or over-the-phone interview by contacting the SSA. If you prefer an in-person interview, use the Social Security Office Locator to find your nearest location. During your interview, fill out Form CMS 1763 as directed by the representative.
Is it easy to cancel Medicare Part B?
Disenrolling in Medicare Part B isn’t an easy process because it requires an in-person or phone interview. But this is intentional. Canceling Part B could have negative consequences for your wallet (in the form of late-enrollment penalties) and your health (in the form of a gap in coverage).
Can Medicare tack late enrollment penalties?
If you have a gap in coverage, the Medicare program could tack late-enroll ment penalties onto your Part B premiums if you re-enroll in coverage again later. Avoid this pitfall by working with your human resources department to ensure that your company's insurance is indeed creditable (meaning that it’s as good or better than Medicare Part B). You may need to provide documentation of creditable coverage during your Part B cancellation interview.
Does Medicare Advantage offer rebates?
Consider a Medicare Advantage plan that offers a rebate on your Part B premium. Here's how that works: A Medicare Advantage plan provides the same or better coverage than Part A (hospital insurance) and Part B (medical insurance). To receive this coverage, most enrollees pay a premium for their Medicare Advantage plan in addition to the cost ...
What is Medicare Part B?
Medicare Part B covers most of the services people expect in a health plan – such as outpatient physician visits , mental health services, lab tests, and physical therapy. It’s important to sign up at the correct time for this part of Medicare – because simple enrollment mistakes can result in gaps in coverage and lifelong premium penalties.
How long is the Medicare Part B enrollment period?
If you meet these criteria, you’ll receive an 8-month long special enrollment period (SEP) during which you can enroll in Part B without penalty. The Medicare Part B SEP begins the sooner of when: ...
How much is the Part B premium for 2020?
The Part B premium in 2020 is $144.60 per month for most people. Consider an individual who qualified for Part B five years ago but didn’t enroll until this year – ...
Can Medicare beneficiaries buy individual market policies?
In fact, Medicare beneficiaries are not allowed to purchase individual market policies other than Medigap plans. Many Americans are enrolled in the individual market when they qualify for Medicare – and can keep their individual market plan after becoming Medicare eligible.
Do you have to pay for Medicare if you have an individual market plan?
But once you’re eligible for Medicare, an individual market plan may pay little or nothing toward your care. This is why it’s important to enroll in Medicare (and a Medigap or Medicare Advantage plan) when you’re first eligible for the benefit.
Do large companies have to enroll in Medicare?
Employees of large companies (i.e., usually one with more than 20 employees) do not have to enroll in Medicare. However, if they choose to sign up for Part A and B, Medicare will act as secondary coverage and pay for care after the GHP pays.
Can you get a cobra if you don't have Medicare?
Furthermore, COBRA carriers may recoup what they paid toward your medical bills when they discover you were eligible for Medicare but not enrolled in it. This is because COBRA plans cover only the portion of your health care claims Medicare wouldn’t be responsible for paying – even if you don’t have Medicare.
What happens if you don't get Medicare at 65?
If you didn’t get Medicare at 65, you would not be later charged with late-enrollment penalties, so long as your employer signed this form indicating you’ve had insurance coverage. The form would be presented when you later needed Medicare. There is an eight-month special enrollment period that begins on the date a person aged 65 ...
How long does Medicare cover after you stop working?
It sounds like you will have retiree coverage and Medicare for five years after you stop working. It would be a good idea for you to find out exactly what your retiree plan covers and how it and Medicare would coordinate payment of any covered insurance claims.
How old do you have to be to qualify for unemployment if you die?
If he died at age 60 or younger, she would qualify for benefits because the agency would adjust the hours needed. Thirty-eight quarters of so-called covered earnings would be enough to qualify for someone who died two years before reaching the earliest age at which benefits normally are available.
Does Cobra continue to provide primary coverage?
Your COBRA insurer, for example, may not continue to provide primary coverage when you turn 65 and would expect Medicare to become your primary insurer then. I urge you to speak with your COBRA insurer to find out if this will be the case.
Can I collect Social Security at 66?
When you apply for your benefit at age 66, she will be eligible for a spousal benefit. If it’s larger than her survivor benefit, she’d receive an additional payment equal to the difference. If not, her benefit would stay the same. Frank: I’m planning to collect Social Security at age 66 this fall.
Can my wife file for spousal benefits at 62?
Under new rules passed in late 2015, there is no way she can file for a spousal benefit while deferring her own retirement filing.
Can my mother get a survivor benefit if my father dies?
Phil Moeller: If your father died after reaching age 62, there is no basis for your mother receiving a survivor benefit, and the rules do not permit another person to contribute credits to his account. If he died at age 60 or younger, she would qualify for benefits because the agency would adjust the hours needed.

How It Works
How Does This Correlate with FEHB?
- It may help to look at an example of a recent retiree: State department Jane retired from a high paying federal career and went on to a second career as a contract worker. Her second career is paying a salary of $160,000 and she is collecting a FERS Annuity of over $50,000. This puts Jane in the IRMAA category where she has to pay $475.20 a month for Part B. Jane’s FEHB plan has …
What About A Roth Conversion?
- If you are over age 65 and paying for Part B, you could increase your IRMAA by performing Roth conversions. A Roth conversion may still be beneficial but be careful. It may end up costing you more than just income taxes to perform the conversion. Plus, there are other tax planning strategiesthat you can use to help reduce AGI as well.
What Can You Do Prior to Age 65?
- One big takeaway for those that aren’t yet Medicare age is the benefit of a lower income. This is something that can be achieved through contributions to Roth TSP, Roth IRAs, and Roth conversions. Distributions from these accounts are not considered taxable income nor are they added to your AGI or used in calculations for IRMAA. If you look at law ...