If you had health coverage other than Medicare during the past tax year: Your other health coverage provider may send you a separate Form 1095-B. Contact the health care provider if you have questions about the coverage they provided.
When does Medicare send out 1095 B?
coverage is considered qualifying health coverage. If you have Part A, you may get IRS Form 1095-B from Medicare in the early part of the year. If you don't get Form 1095-B, don't worry. Not everyone will get this form from Medicare, and you don't need to have it to file your taxes.
Where can I get a copy of my 1095b form?
Form 1095-B. Consumers enrolled in Medicaid, Child Health Plus and Essential Plan (EP) may request a copy of Form 1095-B from the NYS Department of Health. For Medicaid, this includes individuals whose coverage is through Local Departments of Social Services (LDSS), Human Resources Administration (HRA), or NY State of Health. Health plans send the Form 1095-B to consumers who were enrolled in Catastrophic plans, purchased their plan directly from the insurer, or had coverage through the ...
Who issues a 1095 B?
Who Gets a Form 1095-B
- Who will get his or her own Form 1095-B? ...
- Are there people who have Medi-Cal but will not get Form 1095-B? ...
- How do I know if the Medi-Cal program I am or was enrolled in counts as MEC? ...
- Medi-Cal with an unmet Share of Cost
- Restricted Medi-Cal, (sometimes called “emergency" Medi-Cal)
- Family Planning, Access, Care, and Treatment (FPACT)
Do I have to report 1095 B?
The 1095-B will report which months everyone in your household had health insurance coverage. You usually don’t need this info for your return, and you probably already know when you were covered and won’t need to refer to a 1095-B.

What do I do if I didn't get my 1095-B?
If you do not receive a Form 1095-B and you would like a Form 1095-B for your records, you should contact your eligibility worker at your county human services agency to determine why and request a reprint.
How do I get a copy of my 1095-B from Medicare?
Medicare. Call 1-800-MEDICARE (1-800-633-4227) to ask for a copy of your IRS Form 1095-B.
What happens if I don't get my 1095?
Q: What should I do if I don't receive a Form 1095-A? If you purchased coverage through the Marketplace and you have not received your Form 1095-A, you should contact the Marketplace from which you received coverage. You should wait to receive your Form 1095-A before filing your taxes.
Will I get a 1095 if I'm on Medicare?
If you were enrolled in Medicare: For the entire year, your insurance provider will not send a 1095 form. Retirees that are age 65 and older, and who are on Medicare, may receive instructions from Medicare about how to report their health insurance coverage.
How can I get my 1095b online?
How to find your 1095-A onlineLog in to your HealthCare.gov account.Under "Your Existing Applications," select your 2021 application — not your 2022 application.Select “Tax Forms” from the menu on the left.Download all 1095-As shown on the screen.
Do I need my 1095-B to file taxes?
You do not need 1095-B form to file taxes. It is for your records. IRS 1095-B form is your proof of the month(s) during the prior year that you received qualifying health coverage.
What if I received a 1095-B instead of 1095-A?
You will not add this to your return, Form 1095-B is informational only the IRS does NOT need any details from this form. The form verifies you had health insurance coverage. You can keep any 1095-B forms that you get from your employer for your records.
Who sends out 1095-B?
Form 1095-B is sent out by health insurance carriers, government-sponsored plans such as Medicare, Medicaid, and CHIP, and self-insured small employers (large employers, including those that are self-insured, send out Form 1095-C instead). This form is mailed to the IRS and to the insured member.
Is 1095 the same as 1095-B?
Form 1095-A, Health Insurance Marketplace Statement, is provided by the Marketplace to individuals who enrolled or who have enrolled a family member in health coverage through the Marketplace. Form 1095-B, Health Coverage, is provided by insurance companies and other coverage providers.
How do I get my 1099 from Medicare?
Still have questions? If you have questions or need help understanding how to request your replacement SSA-1099 or SSA-1042S online, call our toll-free number at 1-800-772-1213 or visit your Social Security office.
Does Medicare send out tax statements?
Medicare sends a tax statement to beneficiaries between December and January of each year. The document shows a person had Medicare Part A during the tax year. Medicare Part A and Medicare Advantage are classed as qualifying health coverage, under the Affordable Care Act.
Does Medicare send a statement?
It's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the 3-month period.
What is a 1095-B form?
The 1095-B form is a tax document with proof of your coverage and should be stored with any of your other tax documents for the previous year.
What is a 1095A?
In short, the 1095-A form is the document provided to people who purchase their health insurance through the government-run healthcare Marketplace. The form includes basic personal information, such as your name, address, and insurance provider. It also lists anyone covered on the insurance policy, such as you, your spouse, and any children.
What is Medicare Advantage?
Original Medicare Part A and Medicare Advantage programs provide minimum essential coverage required by law as defined by the Affordable Care Act. The government provides a slightly different form to individuals with this coverage, which can include Medicare Part A, Medicare Advantage, Medicaid, CHIP, Tricare, and more.
Does the 1095-B cover insurance?
Since the 1095-B form also covers certain employer-sponsored plans, it provides space for other people covered by the insurance plan . These extra spaces typically shouldn’t apply to you or be a source of concern.
Does Medicare provide a 1095-A?
Since this form applies only to insurance coverage purchased through the Marketplace, Medicare and Medicare Advantage programs do not provide a 1095-A form.
What to do if you don't receive a 1095-B?
If you do not receive a Form 1095-B and you would like a Form 1095-B for your records, you should contact your eligibility worker at your county human services agency to determine why and request a reprint.
When do you get a 1095-B?
You should get a Form 1095-B in the mail by January 31 following the reported tax year. If the information reported on the Form 1095-B was different than what was reported on your state and/or federal taxes, you may need to amend your taxes.
What form do I get for Medi-Cal?
You will get a Form 1095-B for your Medi-Cal coverage from DHCS and you will also get a Form 1095‑A from Covered California. Each form will show the months of coverage that met the requirement for MEC for any months of coverage you got from either Medi‑Cal or Covered California. Some people in my home have Covered California ...
What is MEC on 1095?
The person or their tax preparer will use the information from Form 1095-B as proof of health coverage for that tax year. If you only had health coverage for part of the year or no health coverage at all, the tax penalty no longer applies.
How to obtain a 1095-B?
However, a Form 1095-B can be obtained by a family member with the appropriate documentation. The family member can contact the responsible county for the deceased's Medi-Cal coverage information and request a reprint of their Form 1095-B.
Do I need to file 1095B for ACA?
However, the ACA still requires most people to report to the IRS that they had MEC health coverage for the tax year. Although, you are not required to have Form 1095-B to file your taxes, please save this form for your record. DHCS will mail Form 1095-B to people who had Medi-Cal that met the health coverage requirement by January 31.
Who is required to send 1095-B?
The Department of Health Care Services (DHCS) is required by the state and federal law to send Form 1095-B information to the IRS and FTB for the purpose of validating months of health coverage reported by the person filing their state and/or federal taxes.
When is the 1095-A deadline?
The annual deadline for the Marketplace to provide Form 1095-A is January 31. The deadline for insurers, other coverage providers and certain employers to provide Forms 1095-B and 1095-C to individuals is January 31.
What is a 1095-A?
Form 1095-A, Form 1095-B , and some Forms 1095-C show who in your family enrolled in health coverage and for what months. Form 1095-A also provides premium information and other information you will need to reconcile advance payments of premium tax credit and claim the premium tax credit on Form 8962.
What is self insured form?
Certain employers send this form to certain employees, with information about what coverage the employer offered. Employers that offer health coverage referred to as “self-insured coverage” send this form to individuals they cover, with information about who was covered and when. 2.
What form do I use to get a health insurance premium credit?
Use Form 1095-C to help determine your eligibility for the premium tax credit. If you enrolled in a health plan in the Marketplace, you may need the information in Part II of Form 1095-C to help determine your eligibility for the premium tax credit.
Who provides 1095-A?
Form 1095-A, Health Insurance Marketplace Statement, is provided by the Marketplace to individuals who enrolled or who have enrolled a family member in health coverage through the Marketplace. Form 1095-B, Health Coverage, is provided by insurance companies and other coverage providers.
Can you hand deliver health insurance forms?
The Marketplace, health coverage providers and applicable large employers will mail (or hand deliver) these forms to you or provide them electronic ally to you , if you have consented to electronic delivery.
Do I have to file a 1095A?
You also must file an individual income tax return and submit a Form 8962 to claim the premium tax credit, even if no advance payments of the premium tax credit were made for your coverage. For more information, see the i PDF nstructions to Form 8962, Premium Tax Credit.
What is a 1095-B?
The 1095-B Qualifying Health Coverage Notice is a tax form that was developed in response to a provision of the 2010 Affordable Care Act (ACA). The ACA was phased in over several years, and in 2014, everyone was required to have health insurance through the individual mandate provision. If you had Medicare Part A or Medicare Part C, ...
What happens if you don't have Medicare?
If you had Medicare Part A or Medicare Part C, you met the individual mandate. If you didn’t have health insurance coverage, though, you were subject to a penalty fee, which was calculated as a percentage of your income. In 2019, the U.S. Department of Justice and federal appeals courts ruled that the individual mandate was unconstitutional.
When is the ACA decision due?
A decision on that question is due later in 2020.
When was the minimum essential coverage requirement abandoned?
As a result, the penalty was abandoned starting with the 2019 tax filing year. The minimal essential coverage requirement, which set a standard for what health plans had to cover, was also abandoned – as was the penalty for not meeting this requirement was.
Do you get a 1095B form if you have Medicare?
Here’s what you need to know about the 1095-B form.
Is Medicare Part A essential?
Medicare Part A and Medicare Part C were considered minimum essential coverage under the ACA. If you have one of these plans, the form was sent to prove compliance with the individual mandate and minimal essential coverage requirements.
Who gets a 1095-B form?
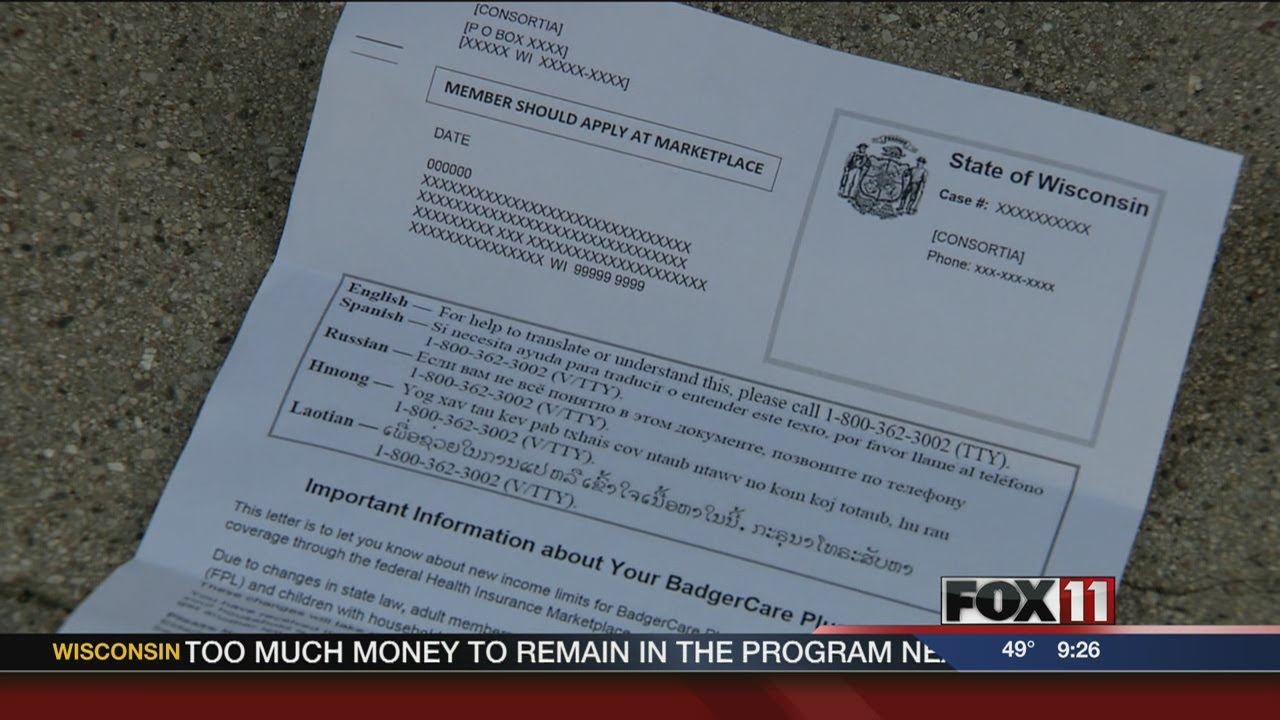
Who gets a 1095-B tax form? The 1095-B form is available for anyone who had at least one month of minimum essential coverage from a State of Wisconsin health care program.
How to get a 1095B?
What information you need to give us when requesting a form: 1 Your full name 2 The member’s full name (if different from the person requesting the form) 3 The member’s ForwardHealth ID, Social Security number, or case number 4 The member’s date of birth 5 The address the 1095-B form needs to be mailed to.
Does Wisconsin require 1095-B?
Some Wisconsin health care programs may not count as minimum essential coverage. The following programs are some of the more common programs that do not meet the requirements to be considered minimum essential coverage: DHS is required to send copies of members’ submitted 1095-B tax forms directly to the IRS.
Is there a penalty for not having health insurance?
Is there a penalty or fee from the IRS for not having health insurance? There is no longer a federal penalty or fine for not having health insurance, so people no longer need proof of insurance coverage when filing their taxes. Based on guidance from the IRS, DHS is not sending IRS 1095-B tax forms to members who had minimum essential coverage ...
What to do if you received a 1095-A?
If you received a Form 1095-A, you will need to enter the information in your tax return. If you have already filed your tax return, you will need to wait to see if it is accepted or rejected. If it is accepted, you will need to amend your tax return to include the Form 1095-A information in your tax return. Please see the steps below ...
How to get 1095-A on my 1095?
Click on Federal from the menu on the left-hand side of the screen. Click on "Deductions & Credits" at the top, scroll down to "Medical" and click on "Show More". Click on "Start" or "Revisit" to the right of "Affordable Care Act (Form 1095-A)". Click on "Yes" and then "Continue". Enter the information from your 1095-A.
How long does it take to update a 1095-B?
Once we receive your updated information, we'll create an updated 1095-B within approximately 30 days. If you have a non-Marketplace individual and family plan, please call us at 844-477-0450 and we will help you update your information. Once your information is updated, we'll create an updated 1095-B within 30 days.
What is a 1095?
SHOP (Small Business Health Options Program) plans. Fully insured plans provided through your large employer. If you have Kaiser Permanente coverage but are enrolled through Medicare, Medicaid, CHIP, or the Marketplace, you should expect to receive your 1095 from one of those government agencies.
Do I need to wait to get my 1095B?
Use the information on this form to help complete your tax return. However, you may not need to wait to receive your 1095 (s) to complete your taxes.
Does Kaiser pay 1095?
If you have Kaiser Permanente coverage but are enrolled through Medicare, Medicaid, CHIP, or the Marketplace, you should expect to receive your 1095 from one of those government agencies. If you receive your coverage from a l arge self-funded employer, you should expect to receive a 1095-C from your employer.