If you use a drug that isn't on your plan's drug list, you'll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception.
What if my drug is not on the formulary?
If a medication is “non-formulary,” it means it is not included on the insurance company's “formulary” or list of covered medications. A medication may not be on the formulary because an alternative is proven to be just as effective and safe but less costly.Mar 7, 2021
Is the request for a non-formulary exception?
The non-formulary exception process provides physicians and members with access to non-formulary drugs and facilitates prescription drug coverage of medically necessary, non-formulary drugs as determined by the prescribing practitioner.
What is formulary override exception?
request letter. A formulary exception is a type of coverage determination used when a drug is not included on a health plan's formulary or is subject to a National Drug Code (NDC) block.
Do all Part D plans use the same formulary?
A Medicare Part D formulary is simply a list of covered prescription drugs and vaccines. The formulary may change at any time, but your plan will notify you when necessary. Formularies can differ form plan to plan, but Medicare dictates some medications that all Medicare Part D formularies must cover.
What is a formulary exception and how are formulary exceptions handled?
A formulary exception is a type of coverage determination request whereby a Medicare plan member asks the plan to cover a non-formulary drug or amend the plan's usage management restrictions that are placed on the drug (for example if the plan has a 30 pill per 30 day Quantity Limit, you might ask for a formulary ...
How does a formulary exception work?
Under a closed formulary pharmacy benefit, the health plan or payer provides coverage only for those drugs listed on the formulary. An exception procedure can be used by prescribers and patients to request coverage for drugs that are not included on a plan's drug formulary.
What are Medicare exceptions?
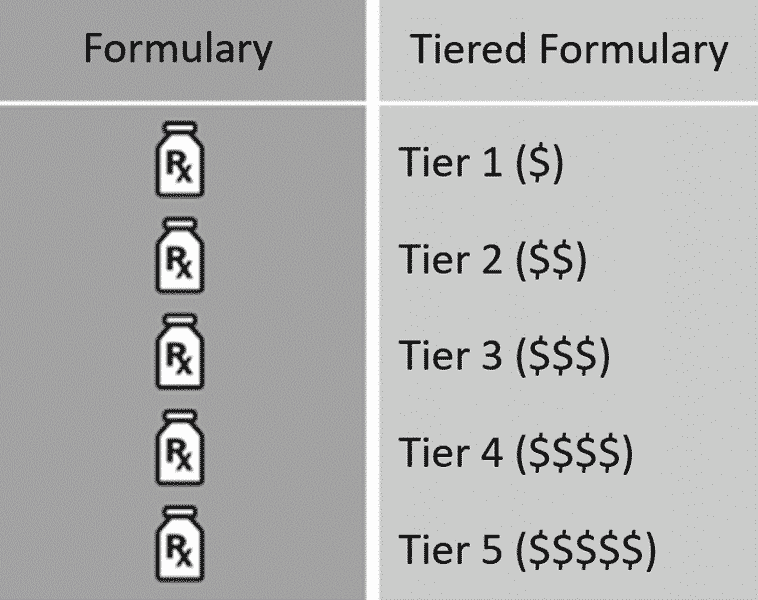
A type of Medicare prescription drug coverage determination. A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
Is the request for an exception to a step therapy edit for a formulary drug?
A step therapy exception request is needed when the prescriber is requesting coverage of a drug that has “step therapy” or requires a person to try the most cost-effective medication(s) in a certain order before coverage of (or “stepping up to”) the less cost-effective medication is granted.
What is a medical formulary?
A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
Do I need Medicare Part D if I don't take any drugs?
No. Medicare Part D Drug Plans are not required coverage. Whether you take drugs or not, you do not need Medicare Part D.Nov 3, 2021
Who determines drug formulary?
A drug formulary is a list of generic and brand-name prescription drugs covered by a health plan. The health plan generally creates this list by forming a pharmacy and therapeutics committee consisting of pharmacists and physicians from various medical specialties.Jan 8, 2019
When did Part D become mandatory?
Medicare Part D Prescription Drug benefit
The MMA also expanded Medicare to include an optional prescription drug benefit, “Part D,” which went into effect in 2006.Dec 1, 2021
The MMA also expanded Medicare to include an optional prescription drug benefit, “Part D,” which went into effect in 2006.Dec 1, 2021