If the amount is greater than your monthly payment from Social Security, or you don’t get monthly payments, you’ll get a separate bill from another federal agency. This agency may be the Centers for Medicare & Medicaid
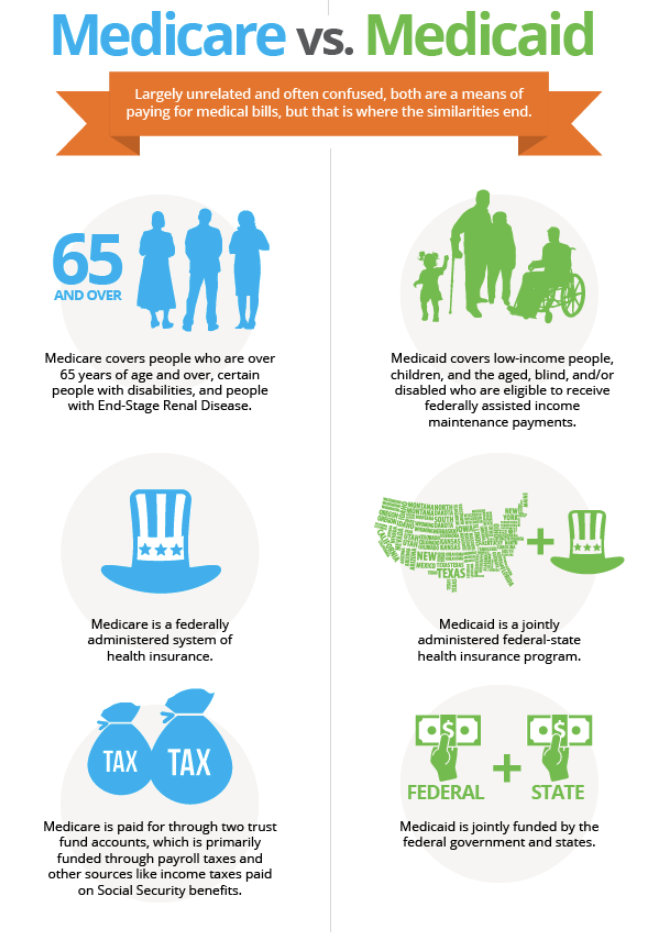
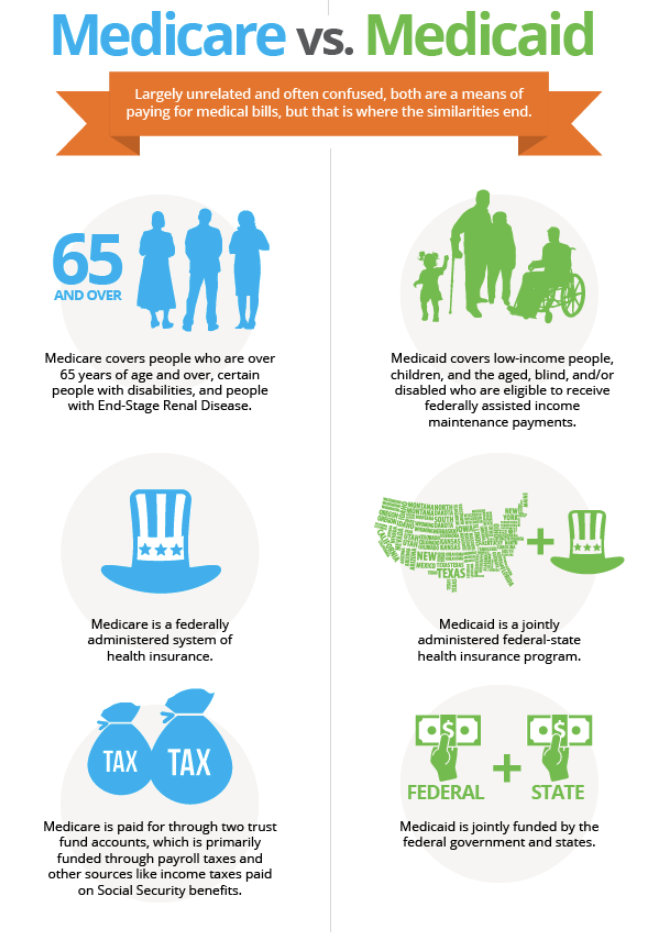
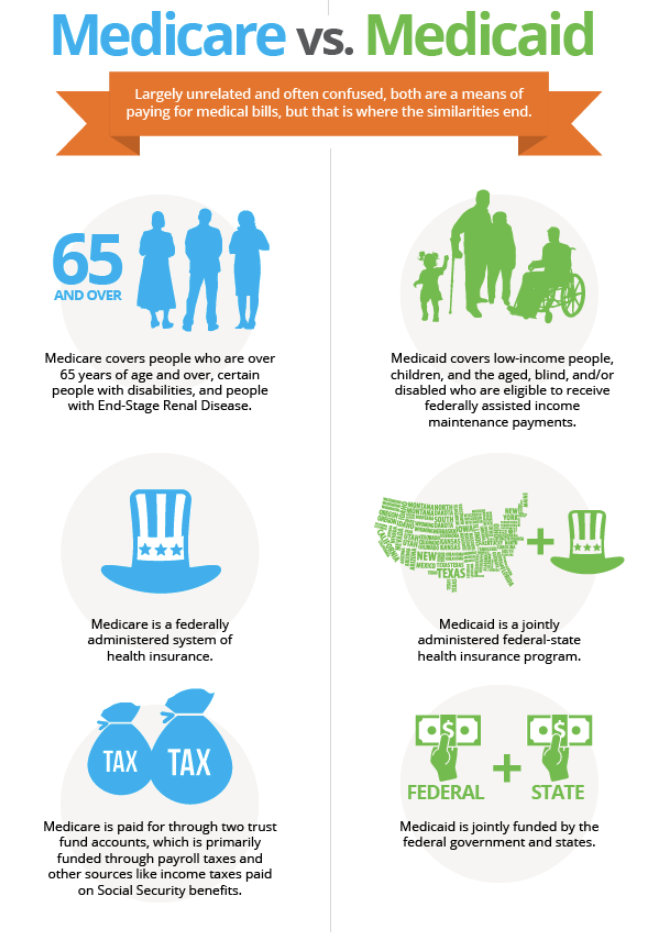
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
How does Social Security affect my Medicare eligibility?
If you’re receiving Social Security benefits, you’ll be automatically enrolled in Medicare once you’re eligible. Medicare premiums can be deducted from your Social Security benefit payment.
What happens to my Medicare card if I join an advantage?
If you join a Medicare Advantage Plan, you’ll still have Medicare but you’ll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare. You must use the card from your Medicare Advantage Plan to get your Medicare-covered services. Keep your red, white and blue Medicare card in a safe place
Can I use my Social Security benefits to pay for Medicare?
Your Social Security benefits can be used to pay some of your Medicare premiums. In some cases, your premiums can be automatically deducted If you receive Social Security Disability Insurance (SSDI) or Social Security retirement benefits. However, this doesn’t apply to all Medicare premiums.
What is the additional amount on my Medicare premium?
We call the additional amount the income-related monthly adjustment amount. Visit Medicare Premiums: Rules For Higher-Income Beneficiaries to see if the adjustment amount applies to you.
Can Medicare Advantage premiums be deducted from Social Security?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
What if I overpaid my Medicare premium?
When Medicare identifies an overpayment, the amount becomes a debt you owe the federal government. Federal law requires we recover all identified overpayments. When you get an overpayment of $25 or more, your MAC initiates overpayment recovery by sending a demand letter requesting repayment.
What income level triggers higher Medicare premiums?
In 2022, higher premium amounts start when individuals make more than $91,000 per year, and it goes up from there. You'll receive an IRMAA letter in the mail from SSA if it is determined you need to pay a higher premium.
How do you qualify for $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
How do I get a refund from Medicare premiums?
Call 1-800-MEDICARE (1-800-633-4227) if you think you may be owed a refund on a Medicare premium. Some Medicare Advantage (Medicare Part C) plans reimburse members for the Medicare Part B premium as one of the benefits of the plan. These plans are sometimes called Medicare buy back plans.
How do I claim Medicare refund?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How much does Social Security take out for Medicare each month?
In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.
Do 401k withdrawals count as income for Medicare?
The distributions taken from a retirement account such as a traditional IRA, 401(k), 403(b) or 457 Plan are treated as taxable income if the contribution was made with pre-tax dollars, Mott said.
Do you still pay Medicare Part B with an Advantage plan?
You continue to pay premiums for your Medicare Part B (medical insurance) benefits when you enroll in a Medicare Advantage plan (Medicare Part C). Medicare decides the Part B premium rate. The standard 2022 Part B premium is estimated to be $158.50, but it can be higher depending on your income.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Who is eligible for Medicare Part B reimbursement?
1. How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B.
What percentage of Medicare Part B is covered by Social Security?
When the “standard” rate for Medicare Part B (health insurance) rises, as it does most years, the roughly 70 percent of Part B enrollees protected by the rule get what amounts to a discount so that their Social Security payment doesn’t decrease.
How much did Medicare Part B cost in 2017?
That happened in 2018, after two straight years of Medicare Part B premium hikes with almost no Social Security COLA. While the base rate for Part B was $134 a month in 2017, most enrollees paid less ($109, on average) to keep their Social Security benefits from decreasing.
Does Social Security go down?
For most Social Security recipients, no. That’s due to the “hold harmless” provision of the Social Security Act, which prevents Social Security payments from going down because Medicare premiums go up.
Does Medicare Part B reduce Social Security?
When the “standard” rate for Medicare Part B (health insurance) rises, as it does most years, the roughly 70 percent of Part B enrollees protected by the rule get what amounts to a discount so that their Social Security payment doesn’t decrease. But … rising Medicare premiums can prevent your Social Security benefits from going up, ...
How many credits do you need to work to get Medicare?
You’re eligible to enroll in Medicare Part A and pay nothing for your premium if you’re age 65 or older and one of these situations applies: You’ve earned at least 40 Social Security work credits. You earn 4 work credits each year you work and pay taxes.
How much is Medicare Part B in 2021?
Your Part B premiums will be automatically deducted from your total benefit check in this case. You’ll typically pay the standard Part B premium, which is $148.50 in 2021. However, you might have a higher or lower premium amount ...
What is Medicare Part C and Part D?
Medicare Part C and Part D. Medicare Part C (Medicare Advantage) and Medicare Part D (prescription drug coverage) plans are sold by private companies that contract with Medicare. Medicare Advantage plans cover everything that Medicare parts A and B do and often include coverage for extra services.
What is the income for Part B in 2021?
Conversely, you’ll pay a higher premium if you have a higher income. In 2021, if you have an individual income of $88,000 or more or joint income of $176,00 or more, you’ll pay more for Part B. This adjusted amount is called an income-related monthly adjustment amount (IRMAA). Both your Part B IRMAA and premium can be automatically taken out ...
Why do people pay less for Part B?
Some people will pay less because the cost increase of the Part B premium is larger than the cost-of-living increase to Social Security benefits. You might also be eligible to receive Part B at a lower cost — or even for free — if you have a limited income.
Is Medicare premium tax deductible?
Medicare premiums are tax deductible. However, you can deduct premiums only once your out-of-pocket medical expenses reach a certain limit.
Can a deceased spouse receive Medicare?
You can also receive Part A without paying a premium if you qualify because of a disability. You can qualify for Medicare because of a disability at any age.
What happens if you don't get Social Security?
If the amount is greater than your monthly payment from Social Security, or you don’t get monthly payments, you’ll get a separate bill from another federal agency , such as the Centers for Medicare & Medicaid Services or the Railroad Retirement Board.
How to determine 2021 Social Security monthly adjustment?
To determine your 2021 income-related monthly adjustment amounts, we use your most recent federal tax return the IRS provides to us. Generally, this information is from a tax return filed in 2020 for tax year 2019. Sometimes, the IRS only provides information from a return filed in 2019 for tax year 2018. If we use the 2018 tax year data, and you filed a return for tax year 2019 or did not need to file a tax return for tax year 2019, call us or visit any local Social Security office. We’ll update our records.
What happens if you file taxes as married filing jointly?
If you file your taxes as “married, filing jointly” and your MAGI is greater than $176,000, you’ll pay higher premiums for your Part B and Medicare prescription drug coverage. If you file your taxes using a different status, and your MAGI is greater than $88,000, you’ll pay higher premiums (see the chart below, Modified Adjusted Gross Income (MAGI), for an idea of what you can expect to pay).
What is the number to call for Medicare prescriptions?
If we determine you must pay a higher amount for Medicare prescription drug coverage, and you don’t have this coverage, you must call the Centers for Medicare & Medicaid Services (CMS) at 1-800-MEDICARE ( 1-800-633-4227; TTY 1-877-486-2048) to make a correction.
What happens if your MAGI is greater than $88,000?
If you file your taxes using a different status, and your MAGI is greater than $88,000, you’ll pay higher premiums (see the chart below, Modified Adjusted Gross Income (MAGI), for an idea of what you can expect to pay).
How to determine 2021 income adjustment?
To determine your 2021 income-related monthly adjustment amounts, we use your most recent federal tax return the IRS provides to us. Generally, this information is from a tax return filed in 2020 for tax year 2019. Sometimes, the IRS only provides information from a return filed in 2019 for tax year 2018. If we use the 2018 tax year data, and you filed a return for tax year 2019 or did not need to file a tax return for tax year 2019, call us or visit any local Social Security office. We’ll update our records.
What happens if you amend your tax return?
If you amended your tax return, and it changes the income we count to determine the income-related monthly adjustment amounts (your MAGI), let us know. Social Security needs to see a copy of the amended tax return you filed and your acknowledgment receipt from IRS. We’ll update our records with the information you provide, and correct or remove your income-related monthly adjustment amounts, as appropriate.
What happens when your Medicare premium ends?
Once your premium free Medicare ends, you will get a notice that will tell you when you can file an application to purchase Medicare coverage. There is a program that may help you with your Medicare Part A premiums if you decide to purchase Part A after your extended coverage terminates.
How long does Medicare coverage last?
You will get at least 7 years and 9 months of continued Medicare coverage, as long as your disabling condition still meets our rules.
How long can you keep Medicare after you return to work?
As long as your disabling condition still meets our rules, you can keep your Medicare coverage for at least 8 ½ years after you return to work. (The 8 ½ years includes your nine month trial work period.)
How to find out about Medicare buy in?
To find out more about this program, contact your county, local or State Social Services or medical assistance office. Ask about the Medicare buy-in program for Qualified Disabled and Working Individuals .
What is special enrollment period?
The special enrollment period is a period of time, during which you may enroll. If you did not enroll during your initial enrollment period because you are covered under a group health plan based on your own current employment or the current employment of any family member.
When did Medicare extend to 4 1/2 years?
On October 1, 2000, a new law extended Medicare coverage for an additional 4 1/2 years beyond the current limit. This law is for people who receive Social Security disability benefits and who go to work.
Is Medicare a second payer?
Medicare is often the "secondary payer" when you have health care coverage through your work. Notify your Medicare contractor right away. Prompt reporting may prevent an error in payment for your health care services.
When will I get Medicare if I am already on Social Security?
You’ll get Medicare automatically if you’re already receiving Social Security retirement or SSDI benefits. For example, if you took retirement benefits starting at age 62, you’ll be enrolled in Medicare three months before your 65th birthday. You’ll also be automatically enrolled once you’ve been receiving SSDI for 24 months.
What is the difference between Medicare and Social Security?
Both programs help people who have reached retirement age or have a chronic disability. Social Security provides financial support in the form of monthly payments, while Medicare provides health insurance. The qualifications for both programs are similar.
Who is eligible for Medicare?
You’ll need to be a United States citizen or have been a permanent legal resident for at least five years. In order to get full coverage, you or your spouse need to meet a work requirement. Meeting the work requirement verifies that you’ve paid into the system.
Who is eligible for SSI?
Social Security Disability Insurance is a type of Social Security benefit for those with disabilities or health conditions that prevent them from working.
How long do you have to wait to get Medicare?
Waiting period. You can also qualify for full Medicare coverage if you have a chronic disability. You’ll need to qualify for Social Security disability benefits and have been receiving them for two years. You’ll be automatically enrolled in Medicare after you’ve received 24 months of benefits.
How much does Medicare cost in 2020?
In 2020, the standard premium amount is $144.60. This amount will be higher if you have a large income.
What is Medicare Part A?
Medicare Part A (hospital insurance). Part A covers services such as hospital stays, long-term care stays, and hospice care.
When can you start receiving survivor benefits?
Normal retirement benefits cannot be started before the age of 62, whereas survivor benefits can begin at age 60 . The fact that your benefits began at age 60 leads me to think that you are receiving a survivor benefit and that you can later switch to your own retirement benefit.
What does "credible" mean in Medicare?
Credibility means that the retiree plan is comparable to a typical Medicare Part D plan.
Does Medicare deduct Medicare premiums?
Once a person is on Medicare, the premiums for Part B of Medicare are deducted from their Social Security payments for people who already have claimed Social Security.
Does Medicare cover assisted living?
Phil Moeller: Your note says she would lose her Medicare, but I think what’s at stake here is whether she would lose her eligibility for Medicaid. Medicare does not cover assisted living, but Medicaid does. States pay a substantial share of Medicaid expenses and require income and assets tests to qualify.
Can you get reduced Social Security if you work?
As far as limits on your earnings are concerned, someone gave you bad information. It is true that your Social Security benefits may be reduced because of outside wage earnings. But any reductions caused by what’s known as Social Security’s earnings test will disappear when you reach your full retirement age. At that time, there will be no reduction in your Social Security benefits due to income from work.
Can a widow defer their own Social Security?
Under Social Security rules, a person who takes a survivor (widow) benefit can defer their own retirement benefit, allowing it to grow until the age of 70, when it reaches its maximum value. Under Social Security rules, a person who takes a survivor benefit can defer their own retirement benefit.