How much can you make to qualify for Medicare?
What Are the Medicare Income Limits in 2021?
- There are no income limits to receive Medicare benefits.
- You may pay more for your premiums based on your level of income.
- If you have limited income, you might qualify for assistance in paying Medicare premiums.
What are the income limits for Medicare?
- When it comes to receiving Medicare benefits, there are no income restrictions.
- You may be asked to pay more money for a premium depending on your income.
- If you have a minimal income, you may be eligible for Medicare premium assistance.
What income is used to determine Medicare premiums?
- You married, divorced, or became widowed.
- You or your spouse stopped working or reduced your work hours.
- You or your spouse lost income-producing property because of a disaster or other event beyond your control.
- You or your spouse experienced a scheduled cessation, termination, or reorganization of an employer’s pension plan.
Does my income affect my Medicare cost?
Your 2018 income as reported on your tax return in 2019 will determine your 2020 Medicare premiums. If your income declines this year, it should automatically reduce your premiums beginning in 2021. The lag is related to how long it takes Social Security to receive complete tax-return records from the IRS.

What is the threshold of income for Medicare?
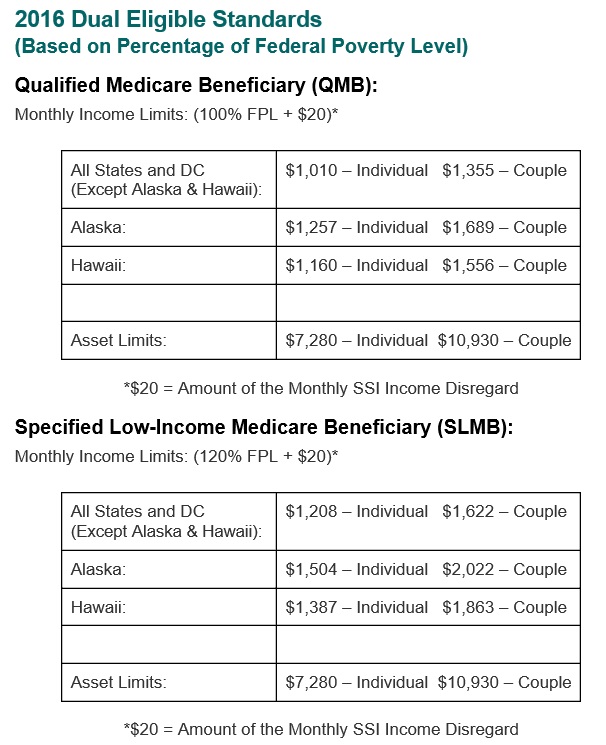
Qualified Medicare Beneficiary (QMB) program You can qualify for the QMB program if you have a monthly income of less than $1,094 and total resources of less than $7,970. For married couples, the limit is less than $1,472 monthly and less than $11,960 in total.
What are the Medicare income brackets for 2020?
Fact sheet 2020 Medicare Parts A & B Premiums and DeductiblesBeneficiaries who file individual tax returns with income:Beneficiaries who file joint tax returns with income:Total monthly premium amountGreater than $87,000 and less than or equal to $109,000Greater than $174,000 and less than or equal to $218,000202.405 more rows•Nov 8, 2019
What is the Medicare earnings limit for 2021?
“The higher premiums are referred to as an Income-Related Monthly Adjustment Amount or IRMAA, and in 2021, IRMAA surcharges apply to individual Medicare beneficiaries who earn more than $88,000, and to couples who earn more than $176,000.
What are the eligibility criteria for the Medicare program?
Be age 65 or older; Be a U.S. resident; AND. Be either a U.S. citizen, OR. Be an alien who has been lawfully admitted for permanent residence and has been residing in the United States for 5 continuous years prior to the month of filing an application for Medicare.
Are Medicare premiums based on income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
Does Social Security count as income for Medicare?
All types of Social Security income, whether taxable or not, received by a tax filer counts toward household income for eligibility purposes for both Medicaid and Marketplace financial assistance.
Do 401k withdrawals count as income for Medicare?
The distributions taken from a retirement account such as a traditional IRA, 401(k), 403(b) or 457 Plan are treated as taxable income if the contribution was made with pre-tax dollars, Mott said.
Who is not eligible for Medicare Part A?
Why might a person not be eligible for Medicare Part A? A person must be 65 or older to qualify for Medicare Part A. Unless they meet other requirements, such as a qualifying disability, they cannot get Medicare Part A benefits before this age. Some people may be 65 but ineligible for premium-free Medicare Part A.
How do you qualify for $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
How many credits can you earn on Medicare?
Workers are able to earn up to four credits per year. Earning 40 credits qualifies Medicare recipients for Part A with a zero premium.
What is the premium for Part B?
Part B premium based on annual income. The Part B premium, on the other hand, is based on income. In 2020, the monthly premium starts at $144.60, referred to as the standard premium.
How does Medicare affect late enrollment?
If you do owe a premium for Part A but delay purchasing the insurance beyond your eligibility date, Medicare can charge up to 10% more for every 12-month cycle you could have been enrolled in Part A had you signed up. This higher premium is imposed for twice the number of years that you failed to register. Part B late enrollment has an even greater impact. The 10% increase for every 12-month period is the same, but the duration in most cases is for as long as you are enrolled in Part B.
What is Medicare's look back period?
How Medicare defines income. There is a two-year look-back period, meaning that the income range referenced is based on the IRS tax return filed two years ago. In other words, what you pay in 2020 is based on what your yearly income was in 2018. The income that Medicare uses to establish your premium is modified adjusted gross income (MAGI).
When will Medicare Part B and Part D be based on income?
If you have Part B and/or Part D benefits (which are optional), your premiums will be based in part on your reported income level from two years prior. This means that your Medicare Part B and Part D premiums in 2021 may be based on your reported income in 2019.
How much is the 2021 Medicare Part B deductible?
The 2021 Part B deductible is $203 per year. After you meet your deductible, you typically pay 20 percent of the Medicare-approved amount for qualified Medicare Part B services and devices. Medicare typically pays the other 80 percent of the cost, no matter what your income level may be.
What is Medicare Part B based on?
Medicare Part B (medical insurance) premiums are based on your reported income from two years prior. The higher premiums based on income level are known as the Medicare Income-Related Monthly Adjustment Amount (IRMAA).
Does Medicare Part D cover copayments?
There are some assistance programs that can help qualified lower-income beneficiaries afford their Medicare Part D prescription drug coverage. Part D plans are sold by private insurance companies, so additional costs such as copayment amounts and deductibles can vary from plan to plan.
Does income affect Medicare Part A?
Medicare Part A costs are not affected by your income level. Your income level has no bearing on the amount you will pay for Medicare Part A (hospital insurance). Part A premiums (if you are required to pay them) are based on how long you worked and paid Medicare taxes.
Does Medicare Part B and D have to be higher?
Learn more about what you may pay for Medicare, depending on your income. Medicare Part B and Part D require higher income earners to pay higher premiums for their plan.
Does Medicare Advantage have a monthly premium?
Some of these additional benefits – such as prescription drug coverage or dental benefits – can help you save some costs on your health care, no matter what your income level may be. Some Medicare Advantage plans even feature $0 monthly premiums, though $0 premium plans may not be available in all locations.
How much does Medicare pay for Part D?
If you earn more than $88,000 but less than $412,000, you’ll pay $70.70 on top of your plan premium. If you earn $412,000 or more, you’ll pay $77.10 in addition to your plan premium. Medicare will bill you for the additional Part D fee every month.
How much do you have to pay in taxes if you make more than $412,000 a year?
If you earn more than $412,000 per year, you’ll have to pay $504.90 per month in taxes. Part B premiums will be cut off directly from your Social Security or Railroad Retirement Board benefits. Medicare will send you a fee every three months if you do not receive either benefit.
What is SLMB in Medicare?
SLMB, or Specified Low-Income Medicare Beneficiary. If you earn less than $1,296 per month and have less than $7,860 in assets, you may be eligible for SLMB. Married couples must make less than $1,744 per month and have less than $11,800 in debt to qualify. This plan covers your Part B premiums.
What happens if you retire in 2020 and only make $65,000?
Loss of income from another source. If you were employed in 2019 and earned $120,000 but retired in 2020 and now only make $65,000 from benefits, you may want to challenge your IRMAA. To keep track of your income fluctuations, fill out the Medicare Income-Related Monthly Adjustment Amount – Life-Changing Event form.
What is the income limit for QDWI?
You must meet the following income criteria if you want to enroll in your state’s QDWI program: Individuals must have a monthly income of $4,339 or less and a $4,000 resource limit. A married couple’s monthly income must be less than $5,833. A married couple’s resource limit must be less than $6,000.
How much do you have to pay for Part B?
If this is the case, you must pay the following amounts for Part B: If you earn less than $88,000 per year, you must pay $148.50 per month. If you earn more than $88,000 but less than $412,000 per year, you must pay $475.20 per month.
Is there a higher income limit for Medicaid in Hawaii?
The income limits are higher in Alaska and Hawaii for all programs. Furthermore, even if your income is slightly above the cap, you may be eligible for these programs if it comes from a job and benefits. If you believe you may qualify for Medicaid, contact the Medicaid office in your state.
What are the expenses that go away when you receive Medicaid at home?
When persons receive Medicaid services at home or “in the community” meaning not in a nursing home through a Medicaid waiver, they still have expenses that must be paid. Rent, mortgages, food and utilities are all expenses that go away when one is in a nursing home but persist when one receives Medicaid at home.
How long does it take to get a medicaid test?
A free, non-binding Medicaid eligibility test is available here. This test takes approximately 3 minutes to complete. Readers should be aware the maximum income limits change dependent on the marital status of the applicant, whether a spouse is also applying for Medicaid and the type of Medicaid for which they are applying.
Is income the only eligibility factor for Medicaid?
Medicaid Eligibility Income Chart by State – Updated Mar. 2021. The table below shows Medicaid’s monthly income limits by state for seniors. However, income is not the only eligibility factor for Medicaid long term care, there are asset limits and level of care requirements.
What is QI in Medicare?
Qualifying Individual (QI) Programs are also known as additional Low-Income Medicare Beneficiary (ALMB) programs. They offer the same benefit of paying the Part B premium, as does the SLMB program, but you can qualify with a higher income. Those who qualify are also automatically eligible for Extra Help.
What is Medicare Savings Program?
A Medicare Savings Program (MSP) can help pay deductibles, coinsurance, and other expenses that aren’t ordinarily covered by Medicare. We’re here to help you understand the different types of MSPs. Below, we explain who is eligible for these programs and how to get the assistance you need to pay for your Medicare.
Does Medicare savers have a penalty?
Also, those that qualify for a Medicare Savings Program may not be subject to a Part D or Part B penalty. Although, this depends on your level of extra help and the state you reside in. Call the number above today to get rate quotes for your area.
Does MAGI include SSI?
Tax-exempt interest. MAGI does not include Supplemental Security Income (SSI) See how to make an estimate of your MAGI based on your Adjusted Gross Income. The chart below shows common types of income and whether they count as part of MAGI.
Is Marketplace Savings based on income?
Marketplace savings are based on total household income, not the income of only household members who need insurance. If anyone in your household has coverage through a job-based plan, a plan they bought themselves, a public program like Medicaid, CHIP, or Medicare, or another source, include them and their income on your application.