Does Medicaid pay for insulin pumps?
Insulin Coverage Insulin Medicare Part B (Medical Insurance) doesn’t cover these: Insulin (unless use of an insulin pump is medically necessary ) Insulin pens Syringes Needles Alcohol swabs Gauze Your costs in Original Medicare You pay 100% for insulin (unless used with an insulin pump, then you pay 20% of the Medicare-Approved Amount
How much insulin would I get from an insulin pump?
Sep 30, 2021 · Medicare Coverage For Insulin And Diabetic Insulin Pumps Patients with Type 1 and Type 2 diabetes that cannot be treated with diet, exercise or oral medication may have to have insulin injections. Insulin injections can be given via a syringe, a pre-filled injectable device called an insulin pen or by using an insulin pump.
Does health insurance cover an insulin pump?
Oct 18, 2021 · Summary Of Information Relating To Insulin And Medicare. Some diabetes pump not covered by Medicare for seniors. The bottom line here is that you must get Part D coverage or a Medicare Advantage insurance plan if you need insulin. With the exception of insulin pumps, Original Medicare will not cover insulin.
What insulin other than NovoLog can I use in pump?
The type of insulin pump you use will determine how much Medicare pays. Medicare Part B is the portion of Medicare that covers a tubed insulin pump. Part B …

Can I get insulin pump on Medicare?
How do I get an insulin pump? If you need to use an insulin pump, your doctor will prescribe it for you. Note: In Original Medicare, you pay 20% of the Medicare-approved amount after the yearly Part B deductible. Medicare will pay 80% of the cost of the insulin and the insulin pump.
Does Medicare pay for insulin pump for Type 2 diabetes?
Medicare will pay 80% of the cost of the insulin and the insulin pump. For more information about durable medical equipment and diabetes supplies, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
What brand of CGM is covered by Medicare 2021?
The Dexcom G6 Continuous Glucose Monitoring (CGM) System is covered by Medicare for patients who meet the Medicare coverage criteria. Medicare coverage for therapeutic CGM includes certain beneficiaries who have either type 1 or type 2 diabetes and intensively manage their insulin.Jan 31, 2022
Is Medtronic Guardian CGM covered by Medicare?
No, the Guardian™ Connect system will not be covered through Medicare because it does not have a durable receiver to meet Medicare benefit requirements. The CGM Access Discount program will still be available for qualifying individuals wanting Guardian™ Connect and who do not have coverage.
What brand of glucose meter does Medicare 2022 cover?
Accu-Chek ® is ALWAYS COVERED on Medicare Part B.
How do I qualify for an insulin pump?
You may be a candidate for insulin pump therapy if you:Are taking insulin injections.Have an A1C greater than 7%Forget to take your insulin injections.Have frequent high or low blood sugars.Enjoy an active lifestyle.Desire to spend less time managing your diabetes.
How can I get Medicare cheaper on insulin?
In 2021, Medicare launched the Part D Senior Savings Model which allowed beneficiaries to enroll in a participating plan to receive their insulin at $35 or less for a 30-day supply.Nov 4, 2021
Are insulin syringes covered by Medicare Part B?
Insulin syringes and needles are not a Part B covered benefit. There may be coverage available under the beneficiary's Medicare Part D Prescription Drug Plan.Feb 9, 2022
How do people afford insulin on Medicare?
For Medicare coverage of insulin, you'll need to enroll in a Medicare Part D prescription drug plan or be enrolled in a Medicare Advantage plan. Some of the most popular types of insulins are covered under Part D plans, including: Lantus.Nov 30, 2021
Why is Medtronic CGM not covered by Medicare?
Why doesn't Medicare cover all CGM? Medicare has historically denied that CGM fits their definition of durable medical equipment (Medicare is required to cover anything that fits in this category). Their criteria for DME are as follows: Durable (can withstand repeated use)Dec 4, 2017
Does Kaiser Cover Medtronic?
Kaiser Permanente's DME office selects the suppliers of these devices. The current insulin pump suppliers are Animas, Tandem, and Medtronic Minimed. Insulin pumps from these companies are covered under your Health Plan benefits. How often can I get a new insulin pump?
How often does Medicare pay for CGM?
Yes, Medicare generally pays 80% of the cost of CGM accessories and supplies. Under the guidelines, Medicare Part B covers: Patch refills based on the recommended replacement schedule. For example, if you use a CGM that requires a new patch every 14 days, Medicare will pay for two patches every 28 days.Oct 12, 2021
How much does an insulin pump cost?
According to a 2018 article in Modern Healthcare, the Omnipod tubeless insulin pump may cost as much as $3,000 to $4,000 per month. Both of these costs are before Medicare pays a portion. Insulin pump costs can vary by manufacturer and model.
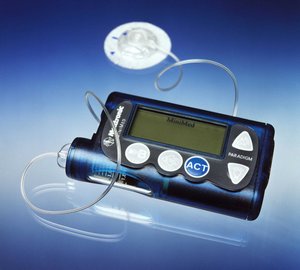
What is tubeless insulin pump?
These are newer devices than tubed insulin pumps. With a tubeless pump, you wear a patch that usually contains several hundred units of insulin. The patch typically works with a smart device to monitor blood sugar levels and deliver insulin.
What is Part B for Medicare?
Part B typically covers doctor’s office visits and durable medical equipment, such as wheelchairs or crutches. Medicare considers an insulin pump a piece of durable medical equipment. You must meet certain requirements for a doctor to prescribe the pump.
How often do you need to check your blood sugar?
needing to check your blood sugar at least four times a day. Medicare Part B also covers the costs of the insulin that tubed pumps use. If you have original Medicare (parts A and B), you’ll pay 20 percent of the Medicare-approved amount for the insulin pump. The Part B deductible applies.
What is Medicare Advantage?
Medicare Part C, or Medicare Advantage, is an alternative to traditional Medicare. It’s when you receive your Medicare benefits through a private insurer that contracts with Medicare. Many Medicare Advantage plans offer additional coverage compared to traditional Medicare, such as vision, dental, or hearing benefits.
Why do you need insulin?
As a result, you may need extra insulin to maintain your blood sugar and prevent negative effects, such as nerve damage, that can result from blood sugar that’s too high. Insulin pumps deliver a continuous or sometimes bolus (all at once) dose of insulin to help you better regulate your blood sugar levels.
How does a tube pump work?
You wear the pump outside your body, and a portion of the pump transfers insulin from the pump to an insert in your subcutaneous (outer layer) of tissue. In this way, it delivers insulin into your body. Tubed pumps have a small tube or tubes that extend from the insulin in the pump to deliver the insulin to you.
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
How long can you have Medicare Part B?
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
What is part B?
Part B covers a once-per-lifetime health behavior change program to help you prevent type 2 diabetes. The program begins with weekly core sessions in a group setting over a 6-month period. In these sessions, you’ll get:
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
What is coinsurance in insurance?
Coinsurance: An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).
