Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Full Answer
Is Medicare always your primary insurance?
Medicare is always primary if it’s your only form of coverage. When you introduce another form of coverage into the picture, there’s predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
When does Medicare become primary?
There are a number of situations when Medicare is primary. Learning about them ahead of time will help you avoid costly enrollment deadlines. You are 65 or Older and Your Employer is a Small Business. Medicare is primary when your employer has less than 20 employees. Medicare will pay first and then your group insurance will pay second.
Who is primary over Medicare?
• If you have Medicare because you’re 65 or over or because you have a disability other than End-Stage Renal Disease (ESRD), Medicare pays first . • If you have Medicare due to ESRD, COBRA pays first and Medicare pays second
When Medicare is primary and secondary?
Medicare is often the primary payer when working with other insurance plans. A primary payer is the insurer that pays a healthcare bill first. A secondary payer covers remaining costs, such as coinsurances or copayments.
How do I know if my Medicare is primary or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Is Medicare primary or secondary insurance?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Does Medicare become primary?
), Medicare pays first. If you have Medicare due to ESRD, COBRA pays first and Medicare pays second during a coordination period that lasts up to 30 months after you're first eligible for Medicare. After the coordination period ends, Medicare pays first.
Is a Medicare Supplement secondary to Medicare?
Medicare Supplements provide extra coverage for what Medicare includes. Thus, your Medigap plan will always be secondary to Medicare. Supplemental insurance is available for what doesn't get coverage. For example, Part D is drug coverage, which is supplemental insurance.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
Can you combine Medicare with private insurance?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
Is Medicare Part D always primary?
Usually Medicare Part D coverage pays first. For example: Are you retired and have prescription drug coverage through your or your spouse's former employer's or union's retiree Group Health Plan and Medicare Part D coverage? If so, your Medicare Part D coverage is primary and the Group Health Plan is secondary.
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
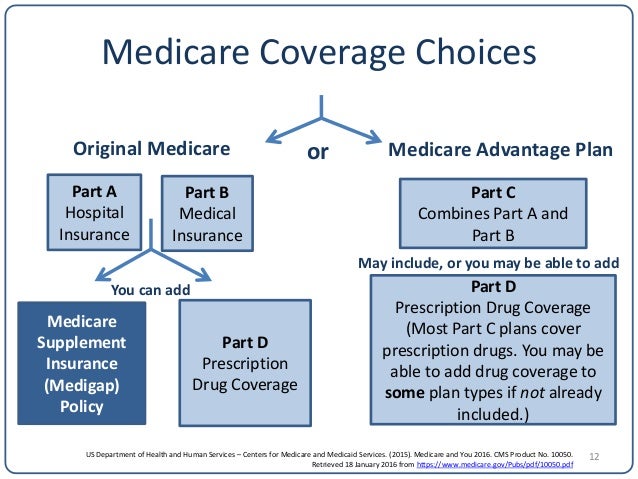
What is the difference between a Medicare Advantage plan and a Medicare Supplement?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
Is supplemental insurance secondary?
It helps cover you for care and services that your primary medical plan may not. This secondary insurance could be a vision plan, dental plan, or an accidental injury plan, to name a few. These are also called voluntary or supplemental insurance plans. Some secondary insurance plans may pay you cash.
Is Medicare Part B the same as supplemental insurance?
Part B is part of what's called Original Medicare, along with Part A. Plan B refers to Medicare supplement insurance commonly called Medigap. Part A covers hospital bills and Part B, for which a standard premium is paid, covers outpatient care, medical equipment, and other services.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
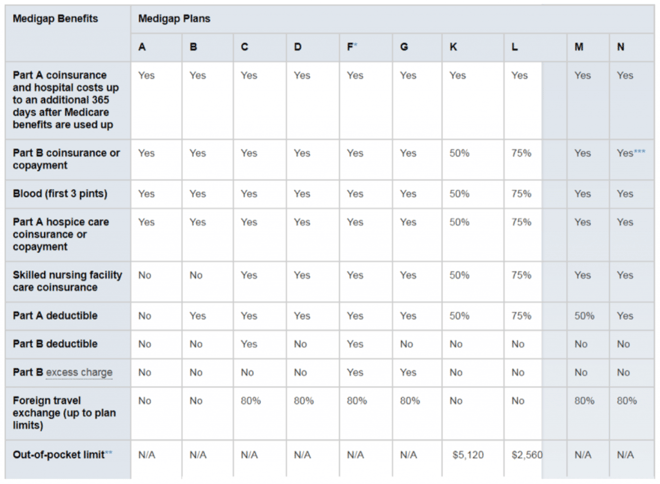
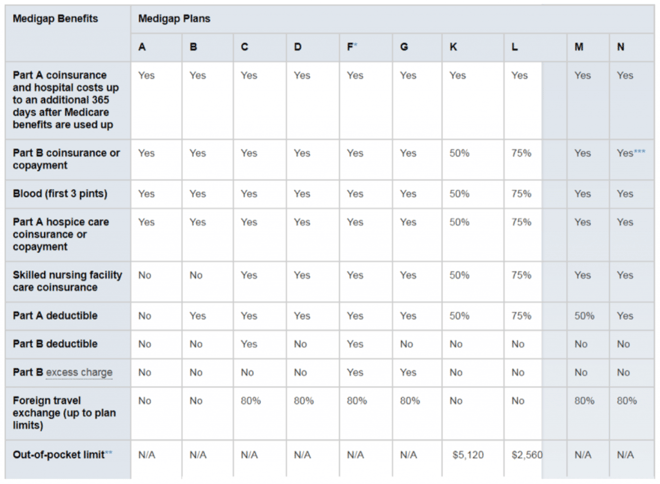
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
Does Medigap cover everything?
Medigap policies don't cover everything. Medigap policies generally don't cover. long-term care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (also called Medigap) and Medicare Advantage plans (Medicare Part C) are two very different private Medicare options that you may consider. This guide highlights the differences between Medicare Supplement Insurance and Medicare Advantage so you can better understand these two private Medicare coverage options.
How many Medicare Supplement plans will be available in 2021?
Medicare Supplement Insurance. Availability. 3,550 different plans available nationwide in 2021 1. 10 standardized plans available in most states, though all 10 may not be available to you in every state. Eligibility. Available to beneficiaries enrolled in Original Medicare who live in the plan’s service area.
How does a Medigap plan work?
Here are a few examples of how a Medigap plan can work: You schedule a doctor’s appointment with a doctor for services that are covered by Medicare Part B. The doctor accepts Medicare “assignment” — this means she accepts Medicare’s reimbursement rate for all covered services as payment in full.
What are the benefits of Medicare Part A and B?
Can offer additional benefits, such as dental, vision, hearing and prescription drug coverage, among other benefits.
How much is Medicare Part A deductible in 2021?
The Medicare Part A deductible is $1,484 per benefit period in 2021. The Medicare Part A deductible is not annual — you could potentially need to meet this deductible more than once in a given year. Medicare Part B deductible. The Medicare Part B deductible is $203 per year in 2021.
What is Medicare Advantage?
Medicare Advantage plans are a type of private Medicare insurance that offers all of the same benefits as Original Medicare. Most Medicare Advantage also offer benefits that are not covered by Original Medicare. Benefits and plan availability can vary from plan to plan.
What is the average Medicare premium for 2021?
The average monthly premium for a Medicare Advantage plan in 2021 is $33.57. 3. You’ll also still pay your Medicare Part B premium in addition to your Medicare Advantage plan premium. The average monthly premium for a Medicare Supplement Insurance plan in 2019 was $125.93. 4.
What is the difference between Medicare and Medicaid?
Eligible for Medicare. Medicare. Medicaid ( payer of last resort) 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided at a VA facility, and VA benefits typically do not work outside VA facilities.
Is Medicare a secondary insurance?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. Go Back. Type of Insurance. Conditions.
What does primary and secondary payer mean?
Each type of coverage you have is called a “payer.” When you have more than one payer, there are rules to decide who pays first, called the coordination of benefits. The “primary payer” pays what it owes on your bills first and sends the remaining amount to the second or “secondary payer.” There may also be a third payer in some cases. 1
When is Medicare primary or secondary?
A number of things can affect when Medicare pays first. The following chart explains some common scenarios. 3 For information on several other scenarios, check out how Medicare works with other insurance , opens new window .
How does Medicare know if I have other coverage?
Medicare doesn’t automatically know if you have other coverage. But your insurers must report to Medicare when they’re the primary payer on your medical claims.
Where to get more details
If you have additional questions about who pays your Medicare bills first, contact your insurance provider or call Medicare’s Benefits Coordination & Recovery Center (BCRC) at 855-798-2627 (TTY: 855-797-2627).
Key Takeaways
Medicare is the primary payer for beneficiaries who do not have other coverage through plans offered by employers, other groups, or unions, except under certain circumstances.
Can I have Medicare and Employer Health Insurance Together?
Yes, you can have both Medicare and employer health insurance together. When you have Medicare and other health insurance or coverage, you have more than one “payer.” In these instances, “coordination of benefits” rules will decide which payer pays first.
Does Medicare Cover Deductibles and Copays as Secondary Insurance?
The downside of having two insurance plans (group and Medicare) is that you pay two sets of premiums and deductibles. Your secondary insurance will not pay toward your primary health insurance deductible, and it’s likely you will still have to pay out-of-pocket costs.
Can I still use my Part A coverage even when I don't have Part B?
Yes, you can use Medicare Part A coverage even if you delay enrollment in Part B. However, unless you have other creditable coverage (like employer coverage) you should enroll in Part B, to avoid penalties in the future.
FAQs
Coordination of benefits (COB) is relevant for individuals with more than one primary payer. It is used to determine which insurance plan has the primary payment responsibility and the extent to which each plan covers an individual.
Medicare Advantage (Part C)
You pay for services as you get them. When you get a covered service, Medicare pays part of the cost and you pay your share.
You can add
You join a Medicare-approved plan from a private company that offers an alternative to Original Medicare for your health and drug coverage.
Most plans include
Some extra benefits (that Original Medicare doesn’t cover – like vision, hearing, and dental services)
Medicare drug coverage (Part D)
If you chose Original Medicare and want to add drug coverage, you can join a separate Medicare drug plan. Medicare drug coverage is optional. It’s available to everyone with Medicare.
Medicare Supplement Insurance (Medigap)
Medicare Supplement Insurance (Medigap) is extra insurance you can buy from a private company that helps pay your share of costs in Original Medicare.