If you have countable financial resources (or assets) at or below two-times the standard allowed by the SSI program and an annual income not higher than 120% of the Federal Poverty Level (FPL
Florida Power & Light
Florida Power & Light Company, the principal subsidiary of NextEra Energy Inc., is a Juno Beach, Florida-based power utility company serving roughly 4.9 million accounts and 10 million people in Florida. It generates, transmits, distributes and sells electric energy.
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Medicare Part D
Medicare Part D, also called the Medicare prescription drug benefit, is an optional United States federal-government program to help Medicare beneficiaries pay for self-administered prescription drugs through prescription drug insurance premiums. Part D was originally propo…
What are the eligibility requirements for slmb programs?
To be eligible for a SLMB program, you must also be eligible for Medicare Part A and meet certain income or resource requirements to qualify. To be eligible for Medicare Part A, you must be 65 years or older or have a qualifying disability, end stage renal disease (ESRD), or amyotrophic lateral sclerosis (ALS).
Should I apply for Medicare slmb?
According to Medicare.gov, you should still apply for SLMB benefits if your income and resources are slightly higher than what’s listed above. What other Medicare Savings Programs are there?
What is slmb (specified low-income Medicare beneficiary)?
One of these Medicare Savings Programs is called SLMB, or Specified Low-income Medicare Beneficiary, which we’ll review below. What does SLMB cover? SLMB benefits cover the cost of the monthly Medicare Part B premium.
Are Me-pickle and Me-disabled adult child recipients eligible for slmb?
Note: ME-Pickle and ME-Disabled Adult Child recipients cannot be dually eligible for SLMB as the Medicare Part B premium is already paid. To be eligible for SLMB, a person must meet the eligibility criteria for QMB (see Section Q-2000 ), except the person must have an income that is greater than 100% but less than 120% of the federal poverty level.
Is SLMB the same as QMB?
QMB: Net countable income at or below 100% of the Federal Poverty Level (FPL) (at or below $908* for a single person, or $1,226* for a couple). SLMB: Net countable income below 120% of the FPL (below $1,089* for a single person, or $1,471* for a couple).
What does SLMB mean in Medicare?
Specified Low-Income Medicare BeneficiarySpecified Low-Income Medicare Beneficiary (SLMB): Pays only the monthly Medicare Part B premiums. • Qualifying Individual (QI): Pays only the monthly Medicare Part B. premiums. However, money for the QI program is limited.
What is the difference between Qi and SLMB?
Specified Low-income Medicare Beneficiary (SLMB): Pays for Medicare Part B premium. Qualifying Individual (QI) Program: Pays for Medicare Part B premium.
What is SLMB only?
Specified Low-Income Medicare Beneficiaries (SLMBs) without other. Medicaid (SLMB Only) - These individuals are entitled to Medicare Part A, have income of greater than 100% FPL, but less than 120% FPL and resources that do not exceed twice the limit for SSI eligibility, and are not otherwise eligible for Medicaid.
How do you qualify for SLMB?
In order to qualify for SLMB benefits you must meet the following income requirements, which can also be found on the Medicare Savings Programs page:Individual monthly income limit: $1,269.Married couple monthly income limit: $1,711.Individual resource limit: $7,730.Married couple resource limit: $11,600.
Does SLMB pay deductible?
Specifically, the program pays for: your Medicare Part A deductible. your Medicare Part B deductible and monthly premiums. other coinsurance and copay costs associated with Medicare Part A and Part B coverage.
Is SLMB retroactive?
If you are enrolled in the SLMB program, you may receive up to three months of retroactive reimbursement for Part B premiums. Unlike QI, you may be reimbursed for premiums from the previous calendar year.
Does Social Security count as income for QMB?
An individual making $1,000 per month from Social Security is under the income limit. However, if that individual has $10,000 in savings, they are over the QMB asset limit of $8,400.
Which program helps individuals whose assets are not low enough to qualify them for Medicaid?
Medicare offers several Medicare Savings Programs (MSPs) that assist people with low income and assets: Qualified Medicare Beneficiary (QMB), Specified Low-Income Medicare Beneficiary (SLMB), Qualified Individual (QI) and Qualified Disabled Working Individual (QDWI). California also offers the 250% California Working ...
How can I reduce my Medicare premiums?
How Can I Reduce My Medicare Premiums?File a Medicare IRMAA Appeal. ... Pay Medicare Premiums with your HSA. ... Get Help Paying Medicare Premiums. ... Low Income Subsidy. ... Medicare Advantage with Part B Premium Reduction. ... Deduct your Medicare Premiums from your Taxes. ... Grow Part-time Income to Pay Your Medicare Premiums.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is SLMB Wisconsin?
The Specified Low Income Medicare Beneficiary (SLMB) Program is a Medicare Savings Program that helps pay for Medicare Part B premiums.
What does SLMB cover?
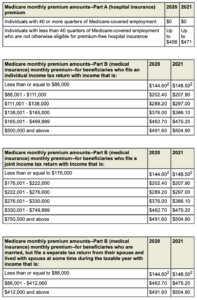
SLMB benefits cover the cost of the monthly Medicare Part B premium. The standard Part B premium in 2021 is $148.50 per month and is required of all Medicare Part B beneficiaries.
How do you qualify for SLMB?
Each state Medicaid program has its own rules concerning qualification.
What other Medicare Savings Programs are there?
SLMB is just one of the available Medicare Savings Programs. Others include:
How do you apply for SLMB?
Contact your state Medicaid program for information and assistance with applying for the SLMB program.
Is there Medicaid assistance for Medicare Advantage beneficiaries?
Individuals who qualify for both Medicare and Medicaid are considered “dual eligible” and may qualify for a certain type of Medicare Advantage plan called a Special Needs Plan. And one particular type of Special Needs Plan is a Dual Eligible Special Needs Plan (D-SNP).
What is the eligibility for SLMB?
SLMB eligibility. To be eligible for a SLMB program, you must also be eligible for Medicare Part A and meet certain income or resource requirements to qualify. To be eligible for Medicare Part A, you must be 65 years or older or have a qualifying disability, end stage renal disease (ESRD), or amyotrophic lateral sclerosis (ALS).
What is SLMB in Medicare?
A Specified Low-Income Medicare Beneficiary (SLMB) program is a state-sponsored program that provides financial assistance in paying for Medicare Part B premiums. To qualify, you or your spouse must have limited income and resources.
What to do if you don't receive a notification from Medicare?
If for some reason you don’t receive a notification, contact your Medicaid office to ensure your benefits don’t run out. When you qualify for the SLMB program, you will receive a notice from Medicare saying that you qualify for Extra Help.
How much is Medicare Part B premium for 2021?
For 2021, the lowest premium amount is $148.50 per month . However, an SLMB program will cover these expenses and lower your overall healthcare costs. If you or a loved one qualifies for an SLMB program, ...
What documents are needed to get Medicaid?
These typically include your Medicare card, Social Security card, birth certificate or other proof of citizenship, proof of address, proof of income, and a bank statement that outlines your assets .
Does medicaid pay for Medicare?
If your application has been approved, Medicaid will start paying for your Medicare Part B premium and will let you know in when coverage will begin. Confirm that Social Security no longer takes out this premium out of your monthly check. Sometimes, it can take time for Medicaid to start paying Medicare directly.
Does a SLMB qualify for a medicaid card?
Specified Low Income Medicare Beneficiaries (SLMB) and Qualifying Individuals (QI) These programs may help pay your Medicare Part "B" Premiums. For a SLMB or a QI, Healthy Connections is required to pay the Medicare Part B premium only. These individuals are not entitled to any other Medicaid benefits; therefore, they do not receive a Medicaid card.
Do you have to pay Medicare Part B for Healthy Connections?
For a SLMB or a QI, Healthy Connections is required to pay the Medicare Part B premium only. These individuals are not entitled to any other Medicaid benefits; therefore, they do not receive a Medicaid card.
What is SLMB in Medicare?
The Specified Low-Income Medicare Beneficiary (SLMB) program is a Medicare Savings Program (MSP) that pays for an enrollee’s Medicare Part B premiums. MSPs are federal programs that are administered by Medicaid in each state. As of 2020, most Medicare beneficiaries pay $144.90 a month for Part B.
How long does it take to get SLMB?
Individuals who are approved for SLMB will receive three months of retroactive benefits. It can take two to three months between being approved for MSP benefits and the time Part B premiums are no longer deducted from Social Security income.
How much does Medicare pay in 2020?
As of 2020, most Medicare beneficiaries pay $144.90 a month for Part B. SLMB enrollees no longer have this amount deducted from their Social Security benefit – amounting to an annual increase of over $1,738. Individuals who are approved for SLMB will receive three months of retroactive benefits.
Does SLMB pay for Part A?
Unlike the Qualified Medicare Beneficiary (QMB) program, SLMB does not pay for Parts A and B cost sharing (e.g. deductibles, co-pays and coinsurance) or for Part A premiums (if an enrollee owes them).
When is the SLMB updated?
These figures are usually updated in April of each year and can be found in the Federal Register, the official government source for administrative changes.
What is the maximum amount of money you can have in 2021?
The resources limits in 2021 is $7,970 for individuals and $11,960 for a married couple. Check the Medicare website for the latest amounts. These limits apply to personal assets including cash, bank accounts, stocks, and bonds.
Does Maryland pay Medicare?
The State of Maryland may assist you in paying for your Medicare premiums. Specified Low Income Medicare Beneficiary program (SLMB) and the Qualified Individual program (QI) program are state programs that helps pay for Medicare Part B (Medical Insurance) premiums for people who have Part A (Hospital insurance) and limited income and resources.
4 kinds of Medicare Savings Programs
Select a program name below for details about each Medicare Savings Program. If you have income from working, you still may qualify for these 4 programs even if your income is higher than the income limits listed for each program.
How do I apply for Medicare Savings Programs?
If you answer yes to these 3 questions, call your State Medicaid Program to see if you qualify for a Medicare Savings Program in your state:.
What is this program?
The Specified Low-Income Medicare Beneficiary (SLMB) Program is one of the four Medicare Savings Programs that allows you to get help from your state to pay your Medicare premiums.
Who is eligible for this program?
In order to qualify for SLMB benefits you must meet the following income requirements, which can also be found on the Medicare Savings Programs page:
Didn't find what you were looking for?
Take our Benefit Finder questionnaire to view a list of benefits you may be eligible to receive.