The SNF PPS also includes an administrative presumption whereby a beneficiary who is correctly assigned one of the designated, more intensive case-mix classifiers on the initial 5-day, Medicare-required assessment is automatically classified as meeting the SNF level of care definition up to and including the assessment reference date (ARD) for that assessment.
| Assessment Type | AI | Medicare Payment Days |
|---|---|---|
| 5-day | 10 | Days 1–14 |
| 14-day | 20 | Days 15–30 |
| 30-day | 30 | Days 31–60 |
| 60-day | 40 | Days 61–90 |
How long does it take to complete the 5-day PPS?
the 5-Day. − Must be completed (Item Z0500B) within 14 days after the ARD (ARD + 14 days). − Authorizes payment for remainder of the PPS stay, beginning on the
What is the Medicare-required PPS assessment schedule?
The Medicare-required PPS assessment schedule includes 5-day, 14-day, 30-day, 60-day, and 90-day scheduled assessments. Except for the first assessment (5-day assessment), each assessment is scheduled according to the resident’s length of stay in Medicare-covered Part A care.
When is the Medicare Part A PPS discharge MDS completed?
The Medicare Part A PPS Discharge MDS is completed when a patient’s Medicare Part A stay ends: When the Medicare Part A stay ends and the patient remains in the facility When the Medicare Part A stay ends and the patient is physically discharged from the facility (the Part A PPS and OBRA Discharge assessments may be combined in this situation)
What does PPS stand for in Medicare?
A Prospective Payment System (PPS) is a method of reimbursement in which Medicare payment is made based on a predetermined, fixed amount. The payment amount for a particular service is derived based on the classification system of that service (for example, diagnosis-related groups for inpatient hospital services).
What is a 5-day PPS?
The SNF PPS establishes a Medicare-Required PPS Assessment schedule. Each required assessment supports reimbursement for a range of days of a Medicare Part A covered stay. The schedule includes assessments performed about Days 5, 14, 30, 60, and 90 of the stay.
What does SNF PPS mean?
The Balanced Budget Act of 1997 mandates the implementation of a per diem prospective payment system (PPS) for skilled nursing facilities (SNFs) covering all costs (routine, ancillary and capital) related to the services furnished to beneficiaries under Part A of the Medicare program.
When completing a Medicare 5-day PPS assessment with an OBRA admission assessment CAAS must be completed no later than which day?
14 daysA: Per CMS long standing policy, the ARD of the PPS Discharge assessment can be set anytime during the completion period. A SNF PPS Discharge assessment is required to be completed no later than 14 days after the date at A2400C (End Date of Most Recent Medicare Stay).
What is a PPS MDS?
Effective October 1st, Medicare requires a Medicare Part A PPS Discharge Assessment. This MDS contains the required data elements used to calculate current and future Skilled Nursing Facility Quality Reporting Program (SNF QRP) quality measures under the IMPACT Act.
What is PPS healthcare?
A Prospective Payment System (PPS) is a method of reimbursement in which Medicare payment is made based on a predetermined, fixed amount. The payment amount for a particular service is derived based on the classification system of that service (for example, diagnosis-related groups for inpatient hospital services).
What is a PPS stay?
The SNF PPS establishes a Medicare-required PPS assessment schedule. Each required assessment supports reimbursement for a range of days of a Part A covered stay. The schedule includes assessments performed around Days 5, 14, 30, 60, and 90 of the stay.
Can you combine 5 day and discharge assessment?
Answer to question 2: The 5-day assessment, the OBRA admission assessment, and the discharge assessment can be combined when the ARD of the discharge assessment is also compatible with the ARD of the 5-day and OBRA admission assessment.
When must a care plan be completed?
The basic care plan includes: A health assessment (a review of your health condition) that begins on the day you're admitted, and must be completed within 14 days of admission. A health assessment at least every 90 days after your first review, and possibly more often if your medical status changes.
How soon after a resident is admitted does an MDS need to be completed by a nurse?
The timing requirements for a comprehensive assessment apply to both completion of the MDS (R2b) and the completion of the RAPs (VB2). For example, an Admission assessment must be completed within 14 days of admission. This means that both the MDS and the RAPs (R2b and VB2 dates) must be completed by day 14.
Do you need 5 days of therapy with PDPM?
Some of these includes: If therapy is going to “count” as a skilled reason for Medicare Part A coverage, it must be delivered 5 days per week. Nursing documentation should demonstrate one or more of the following to support reasonable and necessary skilled care: Management and Evaluation of the Care Plan.
Which of the following assessments is used to support PPS reimbursement?
5-Day assessmentThe SNF PPS establishes a schedule of PPS assessments. The 5-Day assessment is the only required PPS assessment that is used to support PPS reimbursement.
What is an ARD date in MDS?
The ARD is defined as the specific end point of look-back periods in the MDS assessment process. It allows for those who complete the MDS to refer to the same period of time when reporting the condition of the resident. For SNF PPS assessments, this date also determines payment.
Zipcode to Carrier Locality File
This file is primarily intended to map Zip Codes to CMS carriers and localities. This file will also map Zip Codes to their State. In addition, this file contains an urban, rural or a low density (qualified) area Zip Code indicator.
Provider Center
For a one-stop resource web page focused on the informational needs and interests of Medicare Fee-for-Service (FFS) providers, including physicians, other practitioners and suppliers, go to the Provider Center (see under "Related Links" below).
What is the SNF PPS?
The SNF PPS establishes a Medicare-required PPS assessment schedule. Each required assessment supports reimbursement for a range of days of a Part A covered stay. The schedule includes assessments performed around Days 5, 14, 30, 60, and 90 of the stay. Additional unscheduled assessments are required under specific circumstances. The next sections discuss the types of scheduled and unscheduled assessments.
What happens if you conduct an assessment earlier than the schedule indicates?
If you conduct an assessment earlier than the schedule indicates (that is, the ARD is not in the assessment window), you’ll receive the default rate for the number of days the assessment was out of compliance.
What is a short stay policy?
The short stay policy allows assignment into a Rehabilitation Plus Extensive Services or Rehabilitation category when a resident received rehabilitation therapy and was not able to receive 5 days of therapy due to discharge from Medicare Part A. For more information on the requirements for a short stay, refer to Chapter 6 of the “MDS 3.0 RAI Manual” available to download
Does Medicare pay for ARD?
Medicare will pay the default rate for an assessment with an ARD outside the prescribed assessment window for the number of days the ARD is out of compliance. Frequent early or late assessment scheduling practices may result in review.
Can you change your MDS 3.0 assessment?
Once completed, edited, and accepted into the QIES ASAP system, you may not change a previously completed MDS 3.0 assessment as the resident’s status changes during the course of the stay. The MDS must be accurate as of the ARD. You should note minor status changes in the resident’s record. A significant change in the resident’s status warrants a new comprehensive assessment.
What is the PPS in nursing?
The Balanced Budget Act of 1997 mandates the implementation of a per diem prospective payment system (PPS) for skilled nursing facilities (SNFs) covering all costs (routine, ancillary and capital) related to the services furnished to beneficiaries under Part A of the Medicare program. Major elements of the system include:
When will CMS-1746-P be released?
Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program and Value-Based Purchasing Program for Federal Fiscal Year 2022 ( CMS-1746-P) is on public display at the Federal Register and will publish on April 15, 2021.
When is Medicare Part A PPS discharge completed?
The Medicare Part A PPS Discharge MDS is completed when a patient’s Medicare Part A stay ends: When the Medicare Part A stay ends and the patient remains in the facility. When the Medicare Part A stay ends and the patient is physically discharged from the facility (the Part A PPS and OBRA Discharge assessments may be combined in this situation) ...
What is a PPS discharge assessment?
Effective October 1st, Medicare requires a Medicare Part A PPS Discharge Assessment. This MDS contains the required data elements used to calculate current and future Skilled Nursing Facility Quality Reporting Program (SNF QRP) quality measures under the IMPACT Act. The IMPACT Act directs the Secretary to specify quality measures on which post-acute care (PAC) providers (which includes SNFs) are required to submit standardized patient assessment data. Section 1899B (2) (b) (1) (A) (B) of the Act delineates that patient assessment data must be submitted with respect to a resident’s admission to and discharge from a Medicare Part A Assessment.
When is a Medicare Part A discharge MDS required?
In other words, the Medicare Part A Discharge MDS is required any time a Medicare Part A stays ends with the only exception being when a patient expires during a Part A stay. Note that section GG is not required and will not appear on the MDS for any unplanned discharges (e.g. unexpected acute care hospital discharges).
When did the Home Health PPS rule become effective?
Effective October 1, 2000, the home health PPS (HH PPS) replaced the IPS for all home health agencies (HHAs). The PPS proposed rule was published on October 28, 1999, with a 60-day public comment period, and the final rule was published on July 3, 2000. Beginning in October 2000, HHAs were paid under the HH PPS for 60-day episodes ...
What is PPS in home health?
The Balanced Budget Act (BBA) of 1997, as amended by the Omnibus Consolidated and Emergency Supplemental Appropriations Act (OCESAA) of 1999, called for the development and implementation of a prospective payment system (PPS) for Medicare home health services.
When will HHAs get paid?
30-Day Periods of Care under the PDGM. Beginning on January 1 2020, HHAs are paid a national, standardized 30-day period payment rate if a period of care meets a certain threshold of home health visits. This payment rate is adjusted for case-mix and geographic differences in wages. 30-day periods of care that do not meet ...
What happens if you are not physically discharged from Medicare?
If the individual is not physically discharged from the facility at the termination of their Medicare Part A stay, then only SNF PPS Discharge assessment is completed (as long as they do not resume Part A covered services within the 3-day interruption window).
How long does it take for a SNF to return to your SNF?
A: It is not really important to know if they are admitted to another SNF. If they do not return to YOUR SNF within 3 days, then the interruption policy does not apply.
How long do you have to be gone to complete an OBRA discharge?
A: If they are gone more than 24 hours, then you would complete an OBRA Discharge assessment. Whether they are admitted to the hospital or under observation is not the deciding factor on determining an “interrupted stay”.
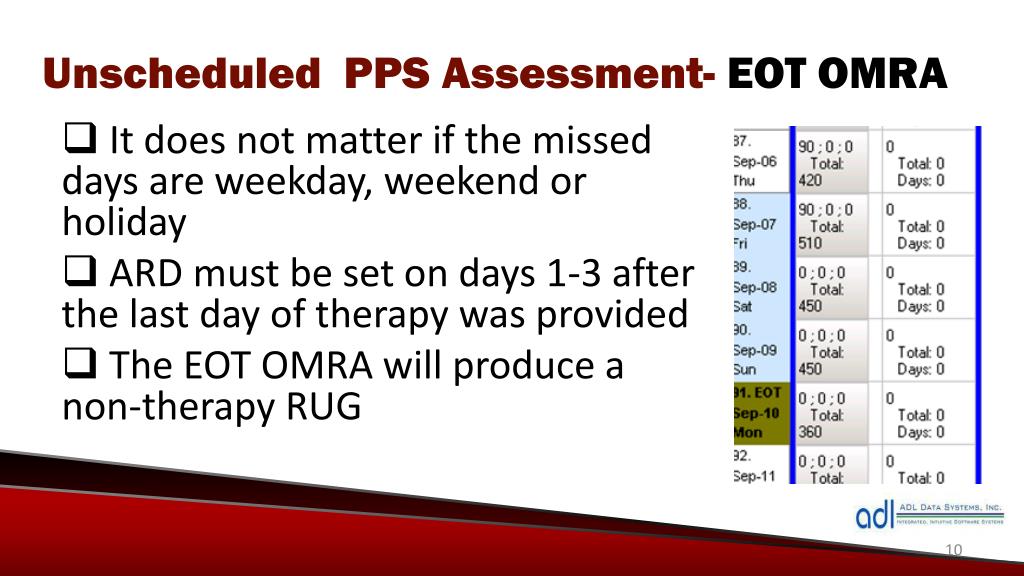
When are EOT and SOT assessments no longer required?
For Medicare purposes, EOT, SOT, and COT assessments will no longer exist as of 10/1/2019. No assessments are required when there is an end of therapy, start of therapy, or a change in therapy intensity.
Is day 25 a non covered day?
A: Technically yes, they are not considered part of the residents 100 days. If a person is discharged to the hospital on day 25, this day now becomes a non-covered day and the day they return would be the new day 25.
Do interrupted stays go against Medicare?
A: No, the days under an interrupted stay do not go against the 100 Medicare days. The Entry Tracking record is required since you would had completed an OBRA Discharge assessment and the resident was subsequently readmitted to the SNF.