When does a benefit period for Medicare begin and end?
Jan 20, 2022 · A benefit period under Part A begins the day you’re admitted to the hospital and ends when you’ve been discharged for at least 60 days. If you’ve been out of the hospital for more than 60 days and are admitted again, a new benefit period begins. Each benefit period requires that you meet a deductible. It’s $1,556 in 2022, but can change each year.
What does Medicare mean by benefit period?
Your benefit period begins the very day you enter a hospital for care or a skilled nursing facility. The benefit period ends when 60 days have passed since you last received either hospital care or care from a skilled nursing facility. The concept of a benefit period is important because the Medicare Part A deductible is based on the benefit period, rather than a calendar year.
Does Medicare Advantage have benefit periods?
Dec 16, 2021 · Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of …
Do I have to pay for Medicare Part?
The Part A benefit runs from the day you’re admitted to a hospital or skilled nursing facility and ends once you’ve gone 60 consecutive days without needing care from either one. During that time, you have 100 days of coverage for SNF care at your disposal. This maximum resets with each benefit period.
What is considered a Medicare benefit period?
A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins.
How long is a Part A benefit period?
60 daysMedicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you've been out of the facility for at least 60 days.
What is a benefit period in insurance?
A benefit period is the length of time during which an insurance policyholder or their dependents may file and receive payment for a covered event. All insurance plans will include a benefit period, which can vary based on policy type, insurance provider, and policy premium.
How are Medicare days counted?
A part of a day, including the day of admission and day on which a patient returns from leave of absence, counts as a full day. However, the day of discharge, death, or a day on which a patient begins a leave of absence is not counted as a day unless discharge or death occur on the day of admission.
What is Medicare Part A deductible for 2021?
Medicare Part A Premiums/Deductibles The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.Nov 6, 2020
What is Part A deductible for 2021?
$1,484The Medicare Part A inpatient hospital deductible that beneficiaries pay if admitted to the hospital will be $1,556 in 2022, an increase of $72 from $1,484 in 2021.Nov 12, 2021
What does policy period mean?
Policy Period — the term of duration of the policy. The policy period encompasses the time between the exact hour and date of policy inception and the hour and date of expiration.
Do Medicare days reset every year?
Yes, Medicare's deductible resets every calendar year on January 1st. There's a possibility your Part A and/or Part B deductible will increase each year. The government determines if Medicare deductibles will either rise or stay the same annually.
How long can you stay in the hospital under Medicare?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.May 29, 2020
Does Medicare have a maximum lifetime benefit?
A. In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
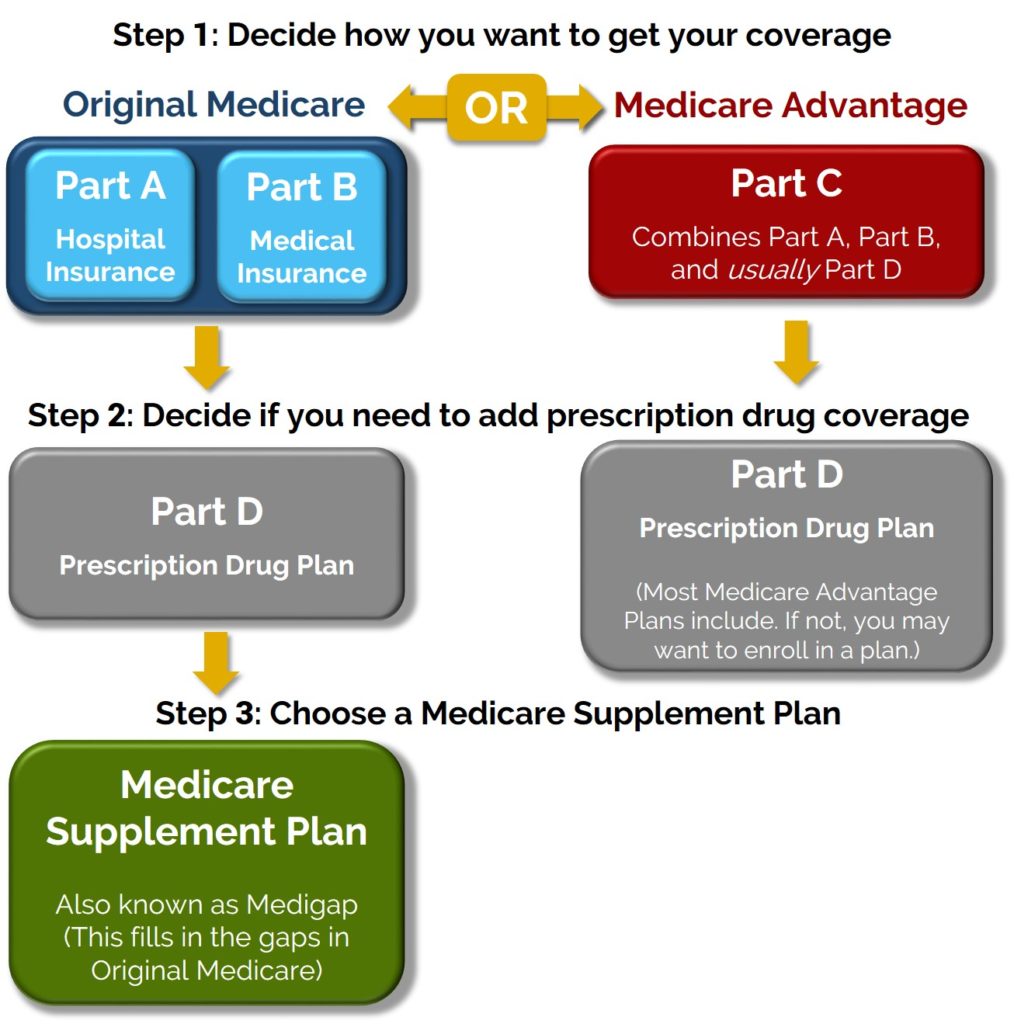
Which part of Medicare covers prescription drugs?
health coverage Medicare drug coverage (Part D) helps you pay for both brand-name and generic drugs. Medicare drug plans are offered by insurance companies and other private companies approved by Medicare.
What percentage of benefit is covered by Medicare Part B?
Medicare Part B covers 80 percent of the Medicare-approved costs of certain services. Most, though not all, of these services are administered on an outpatient basis. This means you don't receive them as a patient in a hospital.Nov 19, 2021
Guide to Explaining The Medicare Hospital Benefit Period
Under Medicare, the hospital benefit period starts once you’ve been admitted to the hospital and expires once you’ve been at home for 60 consecutiv...
Traditional Medicare Hospital Coverage
Here is a breakdown of how much Medicare will cover and how much you’ll owe out-of-pocket for individual hospital benefit periods: 1. You will be e...
Skilled Nursing With Traditional Medicare Coverage
In an Original Medicare plan, you have to stay for a minimum of three days, or more than two nights, to officially be admitted as a patient in a ho...
Options With Medicare Advantage
You are subject to Medicare’s hospital benefit periods if you have a Medicare Advantage health plan. However, the costs for skilled nursing and hos...
What are the benefits of Medicare Part A?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility.
How long does Medicare pay for care?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days ...
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
How much is Medicare deductible for 2021?
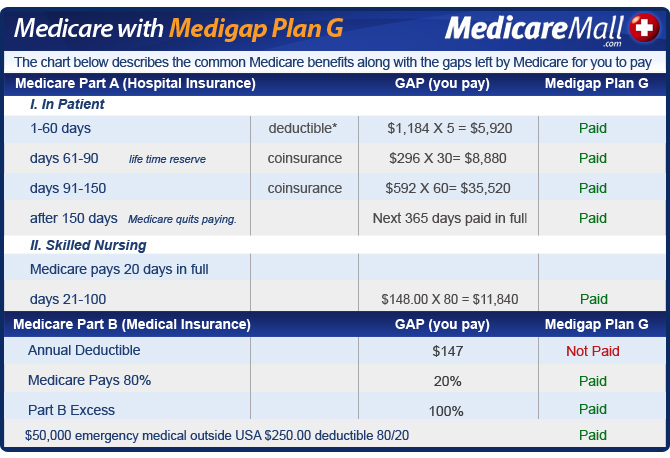
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
How long can you use your lifetime reserve days?
After 90 days, you’ll start to use your lifetime reserve days. These are 60 additional days beyond day 90 that you can use over your lifetime. They can be applied to multiple benefit periods. For each lifetime reserve day used, you’ll pay $742 in coinsurance.
How much is coinsurance for skilled nursing in 2021?
Here is the breakdown of those costs in 2021: Initial deductible. The same Part A deductible of $1,484 applies during each benefit period is $1,484. Days 1 through 20.
How long do you have to be in a hospital to get a new benefit?
You get sick and need to go to the hospital. You haven’t been in a hospital or skilled nursing facility for 60 days. This means you’re starting a new benefit period as soon as you’re admitted as in inpatient.
How much is Medicare coinsurance?
The Medicare recipient is charged a daily coinsurance for any lifetime reserve days used. The standard coinsurance amount is $682 per day. If you’re enrolled in a supplemental Medicare insurance program, also known as “Medigap,” you will receive another 365 days in your lifetime reserve with no additional copayments.
How long do you have to stay in a hospital?
In an Original Medicare plan, you have to stay for a minimum of three days, or more than two nights, to officially be admitted as a patient in a hospital. Only then will Medicare start to pay for your care in a skilled nursing center for additional treatment, like physical therapy or for regular IV injections. The amount of time you spend in the hospital as well as the skilled nursing center will be counted as part of your hospital benefit period. Furthermore, you are required to have spent 60 days out of each in order to be eligible for another benefit period.#N#However, the portion you are expected to pay for the costs of a skilled nursing center differs from the portion you pay for hospital care. In facilities like these, you must pay in any given benefit period: 1 $0 for your room, bed, food and care for all days up to day 20 2 A daily coinsurance rate of $161 for days 21 through 100 3 All costs starting on day 101
Do you have to be hospitalized for 3 days to be eligible for Medicare?
Furthermore, each plan may have rules that differ from the ones found under Original Medicare policies. For instance, with most policies, you don’t have to be hospitalized for three days before you can be moved to a skilled nursing center. If you have one of these policies, refer to the documentation for your coverage. You could also call your provider to find out exactly what hospitalization or a stay in a skilled nursing center will cost you as well as the rules surrounding it.
Call us
Licensed Humana sales agents are available Monday - Friday, 8 a.m. to 8 p.m., local time.
See plans in your area
Enter your ZIP code below to see plans with their premiums, copays, and participating doctors and pharmacies.
Request a call
Our licensed Humana sales agents are available to help you select the coverage that best meets your needs.
How long does Medicare Part A cover?
Once you’ve met your deductible, you’re fully covered for the first 60 days of care and partially covered for 30 days beyond that. Your benefit period will only reset once you’ve been out of the hospital for 60 days.
What is Medicare Part A?
Medicare beneficiaries who are admitted to a hospital for care are covered under Medicare Part A, which covers inpatient care, hospice care, nursing home care, and home health care. Some patients may be covered for additional care with a supplemental Medigap policy or a Medicare Advantage plan, which offers more extensive coverage ...
How much is coinsurance for skilled nursing?
If you are admitted to a skilled nursing facility instead of a hospital, your coinsurance will be $170.50 per day from day 21 up to day 100. Medicare only covers the full cost for days 1 through 20, so while the amount you’ll pay in coinsurance is lower, the number of days you’ll be fully covered is fewer. If you move from a hospital ...
Does Medicare Advantage cover deductible?
Instead, you pay a flat-rate copayment for a set number of days, after which your costs will be covered. Although each plan is different, many Medicare Advantage plans will cover your Part A deductible entirely, so you won’t have to pay it again each time you visit a hospital.
How long does a hospital stay in a SNF?
It starts on the day you are admitted for care at a hospital or skilled nursing facility (SNF) and continues for 60 days after you leave the hospital and no longer receive care. Your Part A deductible, which is $1,364 as of 2019, ...
Does Medigap cover nursing home care?
Most, but not all, Medigap plans cover skilled nursing home care, and several Medigap plans cover your Part A deductible. So while Medigap plans don’t do away with all of your Part A expenses, they can decrease your out-of-pocket costs significantly for long-term hospital stays.
How long does a skilled nursing facility stay in a hospital?
Regardless of whether you are in a hospital or a skilled nursing facility, your benefit period lasts until 60 days after you’ve left the facility and stopped receiving care. This can be confusing if you are readmitted to the hospital or are moved between a hospital and a nursing facility. Keep a record of all of your hospital visits to ensure ...
:max_bytes(150000):strip_icc()/benefitperiod_GettyImages-519516073-2dc70a07fea8477583bceaaa46c4315a.jpg)