What is a Medicare Coverage Determination?
- Your request must be in writing and marked clearly as “A Formal Request for National Coverage Determination”.
- Your request must identify the benefit category (as CMS statutorily defines it) that the service or item applies to. ...
- Your request must include sufficient documentation to support the evidence for an NCD.
Full Answer
What if Medicare denies coverage?
Understanding a Medicare denial letter
- Reasons for coverage denial. It is beneficial for an individual to understand why they have received a Medicare denial letter. ...
- Different types of denial letter. Medicare issues several types of denial letters. ...
- Appeals. ...
- Levels of appeal. ...
- Additional support. ...
- Summary. ...
What are local coverage determinations?
- What item or service you need
- Why the LCD is incorrect
- Why you’re challenging the LCD
What is the definition of coverage determination?
Coverage Determinations. A coverage determination is any decision made by the Part D plan sponsor regarding: Receipt of, or payment for, a prescription drug that an enrollee believes may be covered; A tiering or formulary exception request (for more information about exceptions, click on the link to "Exceptions" located on the left hand side of ...
What is the Order of benefit determination rules?
The order in which the various Plans that cover you pay a claim is called order of benefit determination or coordination of benefits. It follows strict industry and, in some cases, federal rules. 1. Medicaid and Tricare (military insurance) are always secondary to everything. Tricare used to be called CHAMPUS and some places still call it that.
What is a coverage determination request?
A coverage determination is a decision about whether a drug prescribed for you will be covered by us and the amount you'll need to pay, if any. If a drug is not covered or there are restrictions or limits on a drug, you may request a coverage determination.
What does coverage determination by Medicare indicate?
A National Coverage Determination (NCD) is a nationwide determination of whether Medicare will pay for an item or service.
What is a Part D coverage determination?
A coverage determination is an initial coverage decision made by SCAN regarding your Medicare Part D prescription drug. Coverage determinations you can request about your Part D drugs include: You can ask whether a drug is covered for you and whether you satisfy any applicable coverage rules.
What is a coverage decision?
A coverage decision is a decision we make about your benefits and coverage or about the amount we will pay for your medical services or prescription drugs. A coverage decision about medical care or Medicare Part B prescription drugs is called an organization determination.
How long does it take to get a local coverage determination?
The LCD will become effective a minimum of 45 days after the final LCD is published on the MCD. Unless extended by the MAC issuing the LCD, the effective date of the LCD is the 46thcalendar day after the notice period began.
What is CMS local coverage determination?
This section states: “For purposes of this section, the term 'local coverage determination' means a determination by a fiscal intermediary or a carrier under part A or part B, as applicable, respecting whether or not a particular item or service is covered on an intermediary- or carrier-wide basis under such parts, in ...
Can you be turned down for Medicare Part D?
To disenroll from a Medicare drug plan during Open Enrollment, you can do one of these: Call us at 1-800 MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Mail or fax a signed written notice to the plan telling them you want to disenroll.
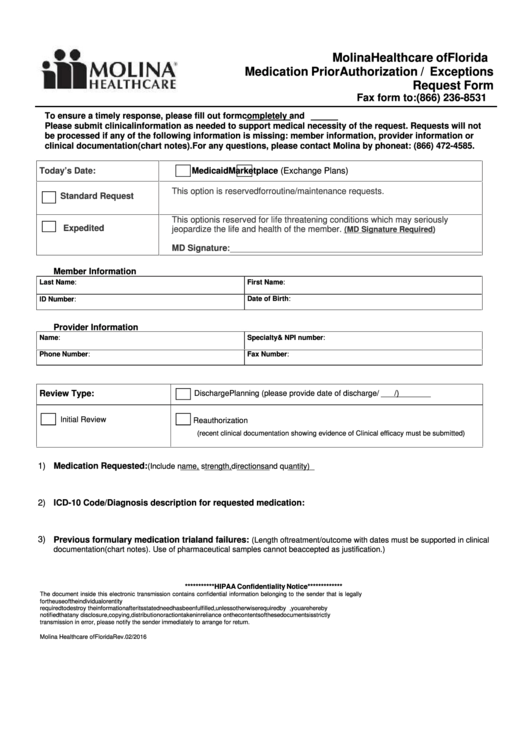
What coverage determination Type S are considered exceptions?
An exception request is a type of coverage determination. An enrollee, an enrollee's prescriber, or an enrollee's representative may request a tiering exception or a formulary exception.
What is the type of coverage determination that is requested for non formulary medications?
A formulary exception is a type of coverage determination request whereby a Medicare plan member asks the plan to cover a non-formulary drug or amend the plan's usage management restrictions that are . . .
How do I get a Medicare Summary Notice?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage. You'll come to the "My communication preferences" page where you can select "Yes" under "Change eMSN preference," then "Submit."
What is prior authorization?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
What is a formulary exception?
A formulary exception is a type of coverage determination used when a drug is not included on a health plan's formulary or is subject to a National Drug Code (NDC) block.
What is a Part D coverage determination?
A coverage determination is any decision made by the Part D plan sponsor regarding: Receipt of, or payment for, a prescription drug that an enrollee believes may be covered;
How to request a standard or expedited coverage determination?
An enrollee, an enrollee's prescriber, or an enrollee's representative may request a standard or expedited coverage determination by filing a request with the plan sponsor. Standard or expedited requests for benefits may be made verbally or in writing. Standard requests for payment must be made in writing, unless the plan sponsor accepts requests ...
What is a prior authorization?
A requirement that an enrollee try another drug before the plan sponsor will pay for the requested drug and the enrollee disagrees with the requirement; or. A decision whether an enrollee has, or has not, satisfied a prior authorization or other utilization management requirement.
How long does it take for a plan sponsor to make a decision?
For requests for benefits that do not involve exceptions, a plan sponsor must provide notice of its decision within 24 hours after receiving an expedited request or 72 hours after receiving a standard request.
What is a local coverage determination?
What’s a "Local Coverage Determination" (LCD)? LCDs are decisions made by a Medicare Administrative Contractor (MAC) whether to cover a particular item or service in a MAC’s jurisdiction (region) in accordance with section 1862 (a) (1) (A) of the Social Security Act. MACs are Medicare contractors that develop LCDs and process Medicare claims.
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. , or both. You need the item (s) or service (s) determined not covered by the LCD.
What is MAC in Medicare?
MACs are Medicare contractors that develop LCDs and process Medicare claims. The MAC’s decision is based on whether the service or item is considered reasonable and necessary.
What Is the Medicare Determination Process?
Original Medicare is meant to cover items, treatments and services that are medically necessary. A nine-month process determines the final decision. The first phase of the process lasts six months.
National Coverage Determinations (NCDs)
A national coverage determination (NCD) decides coverage for a treatment or service that applies to the entire nation. An NCD is also determined through a nine-month process.
What Is a Medicare NCD?
An NCD defines coverage for a particular item (e.g., a brace or hearing aid) or service (e.g., therapy or screenings) nationwide. For example, a Medicare national coverage decision might specify coverage restrictions based on certain clinical conditions, prerequisite treatments and other factors.
What Is a Medicare LCD?
An LCD defines Medicare coverage for items and services for which no NCD exists. For example, there might be a local coverage determination for a new service or an item for which Medicare hasn’t yet published an national coverage determination.
Is There One Place I Can Go to Find Information About NCDs and LCDs?
Yes. The Medicare Coverage Database includes both LCDs and NCDs that are currently in place. Medicare provides a guide to help beneficiaries navigate the database.
What Should I Keep in Mind When Reading an NCD or LCD?
It’s easy to become overwhelmed when reading an NCD or LCD because they usually include a lot of clinical language. The “coverage guidance” is an important one to read, because that will explain any indications, limitations or medical necessity for a given service or item.
Can I Challenge an NCD or LCD?
Yes. If you don’t agree with an LCD or NCD, you can challenge it if you have Medicare Part A or B (or both) and you need the item or service not covered by the NCD or LCD.
