Dual eligible beneficiaries are the most chronically ill patients within both Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
What is the Max income for Medi Cal?
Sep 24, 2020 · Accordingly, dual-eligible enrollees must be age 65 and over, or if under age 65, have been receiving disability benefits for 24 months from the Social Security Administration. In order to qualify for Medi-Cal, dual-eligible enrollees also must have low …
How is Medicare different from Medi-Cal?
Mar 22, 2021 · Dual Eligibles Coordinated Care Demonstration - Cal MediConnect. California's Medi-Cal program and the Centers for Medicare & Medicaid Services (CMS) partnered to launch a financial alignment demonstration to promote coordinated health care delivery for Californians who are dually eligible for both Medicare and Medi-Cal. The demonstration – known as Cal …
How to apply for Medi Cal?
total expenditures for dual eligible beneficiaries in California, for both Medicare and Medi-Cal spending, was $20.9 billion. Dual eligible beneficiaries are the most chronically ill patients within both Medicare and Medicaid, requiring a complex array of services from multiple providers. Despite the complexity of their needs, the vast majority of dual eligibles remain in the …
Is Medi Cal good insurance?
Jun 16, 2020 · Dual-eligible enrollees are requiredto enroll in a Medi-Cal plan in all 22 COHS counties and in the seven CCI counties (two of which — Orange and San Mateo Counties — are also COHS counties). As of June 2020, 1,011,086 dual-eligible enrollees reside in the 27 counties in which Medi-Cal enrollment is mandatory.35.
What is a dual-eligible Medi-Cal?
Dual-Eligible Enrollees Defined In this paper, dual-eligible enrollees are those who qualify for both Medicare and full Medi-Cal benefits. (Some people qualify for Medicare and partial Medi-Cal benefits; they are not included in the data in this paper.)Sep 24, 2020
Can a person have both Medicare and Medi-Cal?
People who qualify for both Medicare and full Medi-Cal are known as “dual eligibles” or “Medi-Medis.”
How do you qualify for both Medicaid and Medicare?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).Feb 11, 2022
Can you have Medicare and Medicaid at the same time in California?
The short answer to whether some seniors may qualify for both Medicare and Medi-Cal (California's Medicaid program) is: yes. Although some people under age 65 qualify for Medicare, such as individuals with end-stage renal disease (ESRD), our focus in this post is on seniors age 65 and older.Mar 9, 2015
When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
What is the difference between Medicaid and Medi-Cal in California?
Actually, the good news is – there is no difference between the two. Medi-Cal health insurance is merely California's Medicaid program, which is paid for with federal and state tax revenues.
Can you switch from Medicare to Medicaid?
You can qualify for both Medicaid and Medicare. If you're eligible for both, most of your health care costs will have coverage. Anyone eligible for both at the same time is dual-eligible. Further, Nearly 20% of Medicare recipients can get full Medicaid.
Do I need supplemental insurance if I have Medicare and Medicaid?
Do You Need Medicare Supplement Insurance if You Qualify for Medicare and Medicaid? The short answer is no. If you have dual eligibility for Medicare and full Medicaid coverage, most of your health costs are likely covered.
What are the disadvantages of Medicaid?
Disadvantages of MedicaidLower reimbursements and reduced revenue. Every medical practice needs to make a profit to stay in business, but medical practices that have a large Medicaid patient base tend to be less profitable. ... Administrative overhead. ... Extensive patient base. ... Medicaid can help get new practices established.
What happens to my Medicaid when I turn 65?
To be clear, Medicaid remains available after age 65 and many older adults rely on it — for example, the majority of nursing home residents in the United States have Medicaid coverage in addition to their Medicare coverage. But once you turn 65, eligibility for Medicaid is based on both income and assets.Oct 14, 2021
What are the differences between Medicare and Medicaid?
Medicare is a federal program that provides health coverage if you are 65+ or under 65 and have a disability, no matter your income. Medicaid is a state and federal program that provides health coverage if you have a very low income.
Will Medicaid pay for my Medicare Part B premium?
Medicaid can provide premium assistance: In many cases, if you have Medicare and Medicaid, you will automatically be enrolled in a Medicare Savings Program (MSP). MSPs pay your Medicare Part B premium, and may offer additional assistance.
What is DMHC in California?
California’s Department of Managed Health Care (DMHC) also provides oversight of managed care plans in the state, including Medicare plans and most Medi-Cal plans.21. In California, dual-eligible enrollees represent just 25% of all Medicare enrollees, but account for 39% of Medicare expenditures. Payment and Spending.
What is California Health Care Foundation?
The California Health Care Foundation is dedicated to advancing meaningful, measur- able improvements in the way the health care delivery system provides care to the people of California, particularly those with low incomes and those whose needs are not well served by the status quo.
Does Medicare pay for nursing home care?
Medicare also pays for limited long-term services and supports (LTSS), including up to the first 100 days in a nursing facility and home health care when an individual is deemed home-bound ( see Appendix A).
What is Medicare dual eligible?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program for seniors and disabled persons, Medicaid is a state and federal medical assistance program for financially needy persons of all ages. Both programs offer a variety of benefits, including physician visits and hospitalization, but only Medicaid provides long-term nursing home care. Particularly relevant for the purposes of this article, Medicaid also pays for long-term care and supports in home and community based settings, which may include one’s home, an adult foster care home, or an assisted living residence. That said, in 2019, Medicare Advantage plans (Medicare Part C) began offering some long-term home and community based benefits.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
How old do you have to be to apply for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
Does Medicare provide long term care?
Long-Term Care Benefits. Medicaid provides a wide variety of long-term care benefits and supports to allow persons to age at home or in their community. Medicare does not provide these benefits, but some Medicare Advantage began offering various long term home and community based services in 2019. Benefits for long term care may include ...
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Is there an age limit for Medicare?
Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
What is dual eligible?
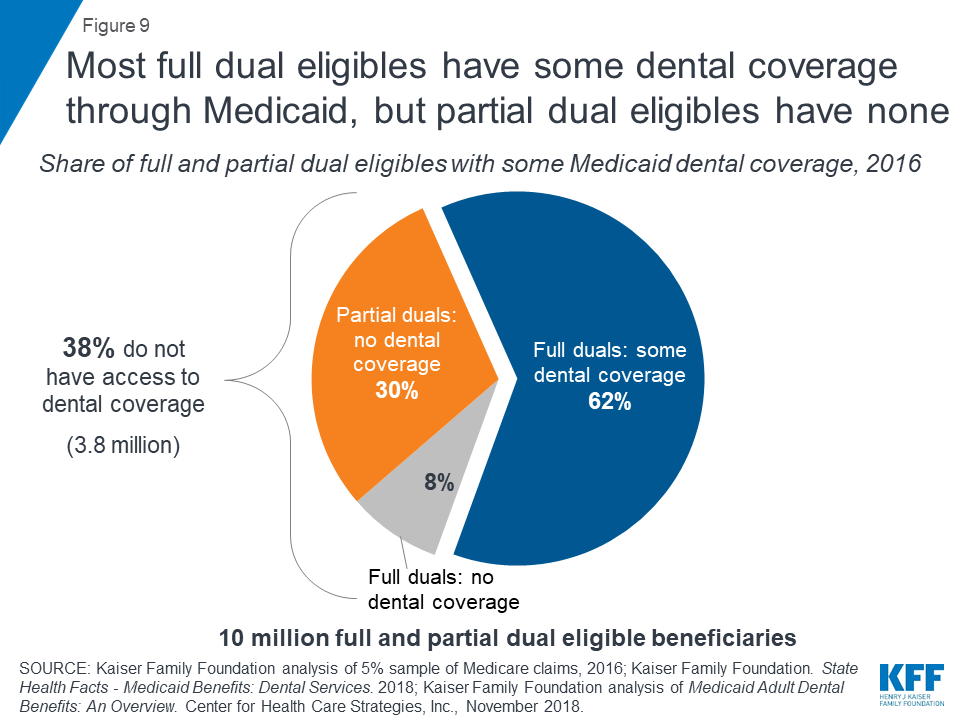
The term “full dual eligible” refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as “partial dual eligible.”.
Does Medicare pay for out of pocket?
If you are dual eligible, Medicaid may pay for your Medicare out-of-pocket costs ...
What is Medicare Advantage?
Medicare Advantage plans are private insurance health plans that provide all Part A and Part B services. Many also offer prescription drug coverage and other supplemental benefits. Similar to how Medicaid works with Original Medicare, Medicaid wraps around the services provided by the Medicare Advantage plan andserves as a payer of last resort.
Is Medicaid a payer of last resort?
Medicaid is known as the “payer of last resort.”. As a result, any health care services that a dual eligible beneficiary receives are paid first by Medicare, and then by Medicaid.
What is Medicaid managed care?
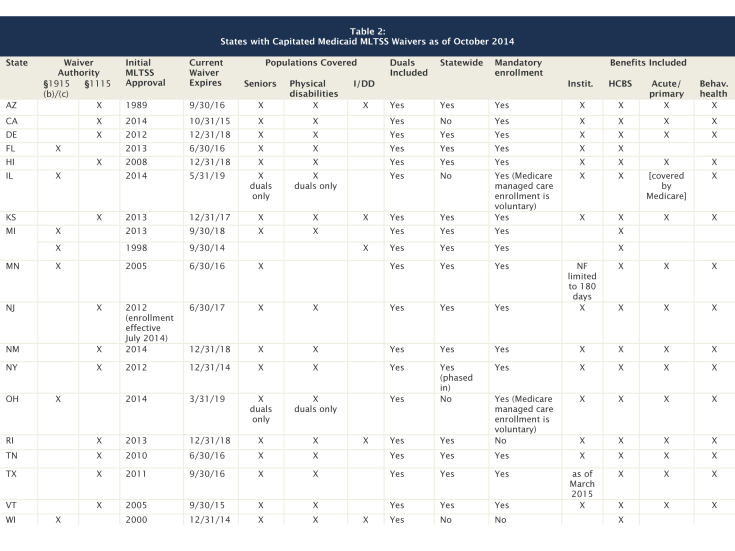
Medicaid managed care is similar to Medicare Advantage, in that states contract with private insurance health plans to manage and deliver the care. In some states, the Medicaid managed care plan is responsible for coordinating the Medicare and Medicaid services and payments.
Does Medicare cover Part A and Part B?
Some Medicare beneficiaries may choose to receive their services through the Original Medicare Program. In this case, they receive the Part A and Part B services directly through a plan administered by the federal government, which pays providers on a fee-for-service (FFS) basis. In this case, Medicaid would “wrap around” Medicare coverage by paying for services not covered by Medicare or by covering premium and cost-sharing payments, depending on whether the beneficiary is a full or partial dual eligible.
What is dual eligible for medicaid?
Qualifications for Medicaid vary by state, but, generally, people who qualify for full dual eligible coverage are recipients of Supplemental Security Income (SSI). The SSI program provides cash assistance to people who are aged, blind, or disabled to help them meet basic food and housing needs.
What is Medicaid in California?
Medicaid in California is called Medi-Cal. While Medicaid is often thought of as a health care program, Medicaid long term care in California pays for many non-medical support services that help frail seniors remain living in their homes. The American Council on Aging now offers a free, quick and easy Medicaid eligibility test for seniors.
What are countable assets?
Countable assets include cash, stocks, bonds, investments, credit union, savings, and checking accounts, and real estate in which one does not reside. However, for Medicaid eligibility, there are many assets that are considered exempt (non-countable).
Does Medi-Cal pay for nursing home care?
In addition to paying for nursing home care, Medi-Cal offers five programs / HCBS Waivers relevant to the elderly that helps them to remain living in their homes or in assisted living residences.
Is the stimulus check considered income?
Covid-19 stimulus checks (both previous and subsequent payments) are not considered income and do not impact Medicaid eligibility. When just one spouse of a married couple is applying for nursing home Medicaid or a Medicaid waiver, only the income of the applicant is counted.